Obstet Gynecol Sci.
2021 Jul;64(4):364-373. 10.5468/ogs.20373.
The rates of major malformations after gestational exposure to isotretinoin: a systematic review and meta-analysis
- Affiliations
-
- 1Korean Mothersafe Counselling Center, Pregnancy & Breastfeeding Medicines Information Center, Seoul, Korea
- 2Department of Obstetrics and Gynecology, Inje University Ilsan Paik Hospital, Goyang, Korea
- 3Department of Obstetrics and Gynecology, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul, Korea
- 4Department of Obstetrics and Gynecology, National Medical Center, Seoul, Korea
- 5Clinical Research Center, Asan Institute for Life Sciences, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 6Motherisk Israel and Adelson faculty of Medicine, Ariel University, Ariel, Israel
- KMID: 2518379
- DOI: http://doi.org/10.5468/ogs.20373
Abstract
Objective
Isotretinoin is among the most notorious human teratogens, documented originally as causing up to 30% of malformations. This systematic review and meta-analysis aimed to evaluate the rates of major malformation (MM) among isotretinoin-exposed pregnant women over the years through a systematic review and meta-analysis.
Methods
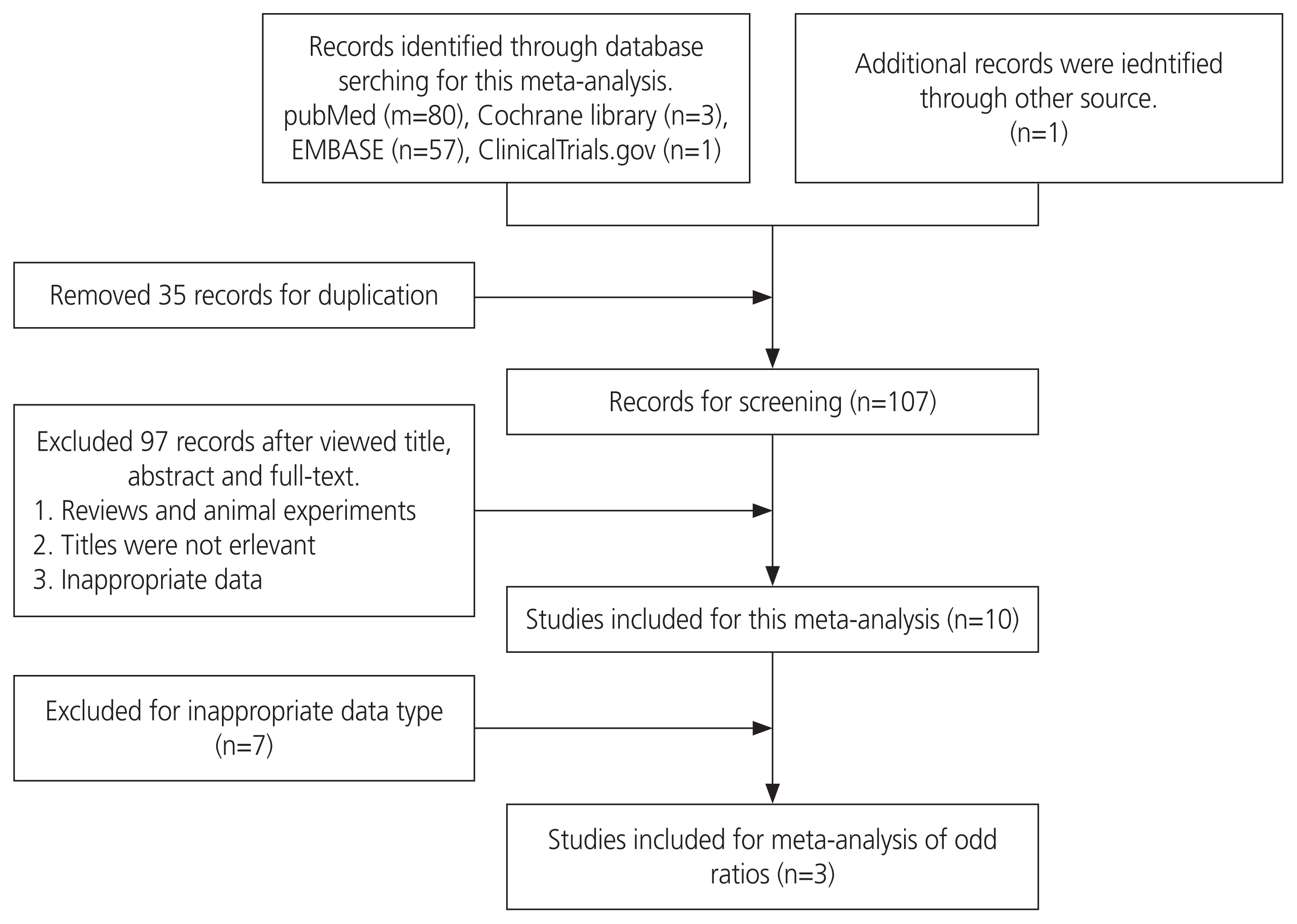
Eligible studies were searched and identified using various databases. Single-arm meta-analysis and meta-analysis of odd ratios among controlled studies were performed using Review Manager version 5.3.
Results
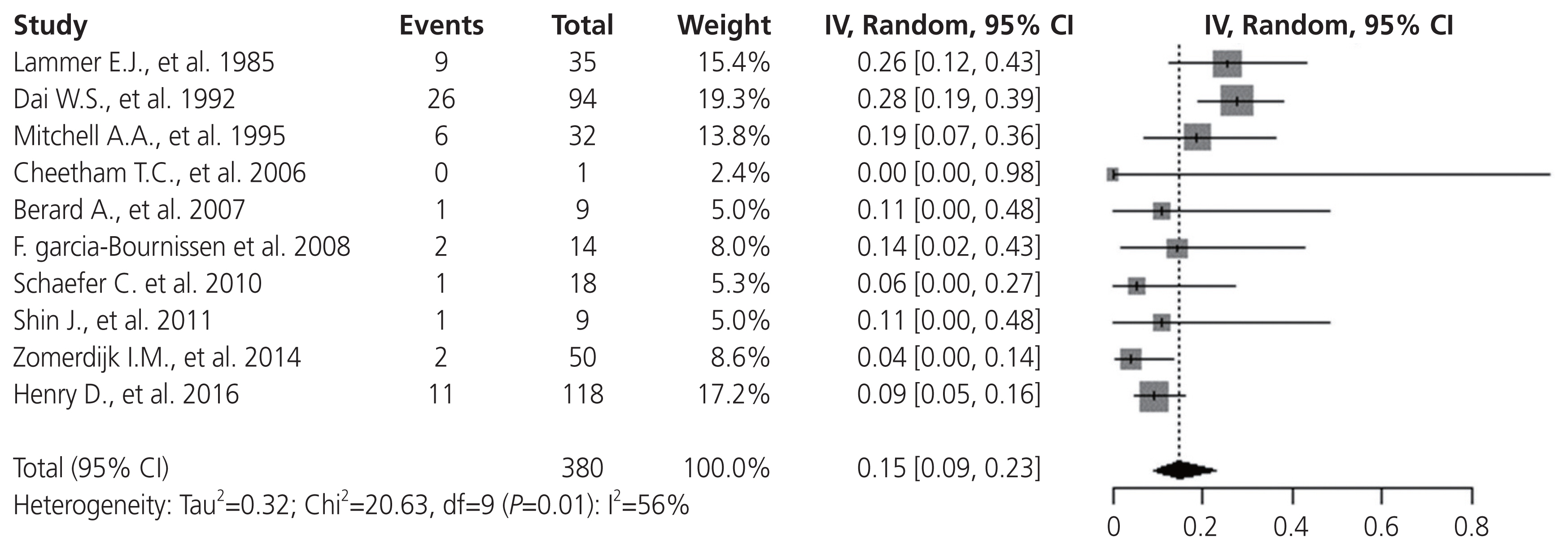
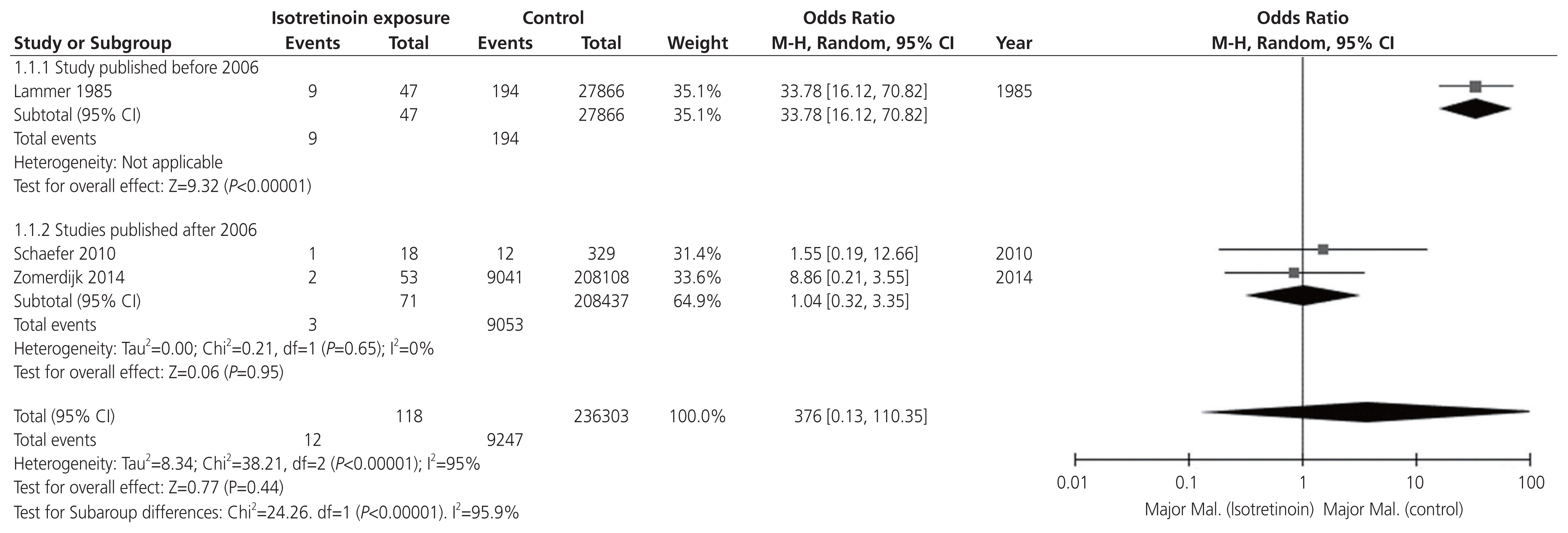
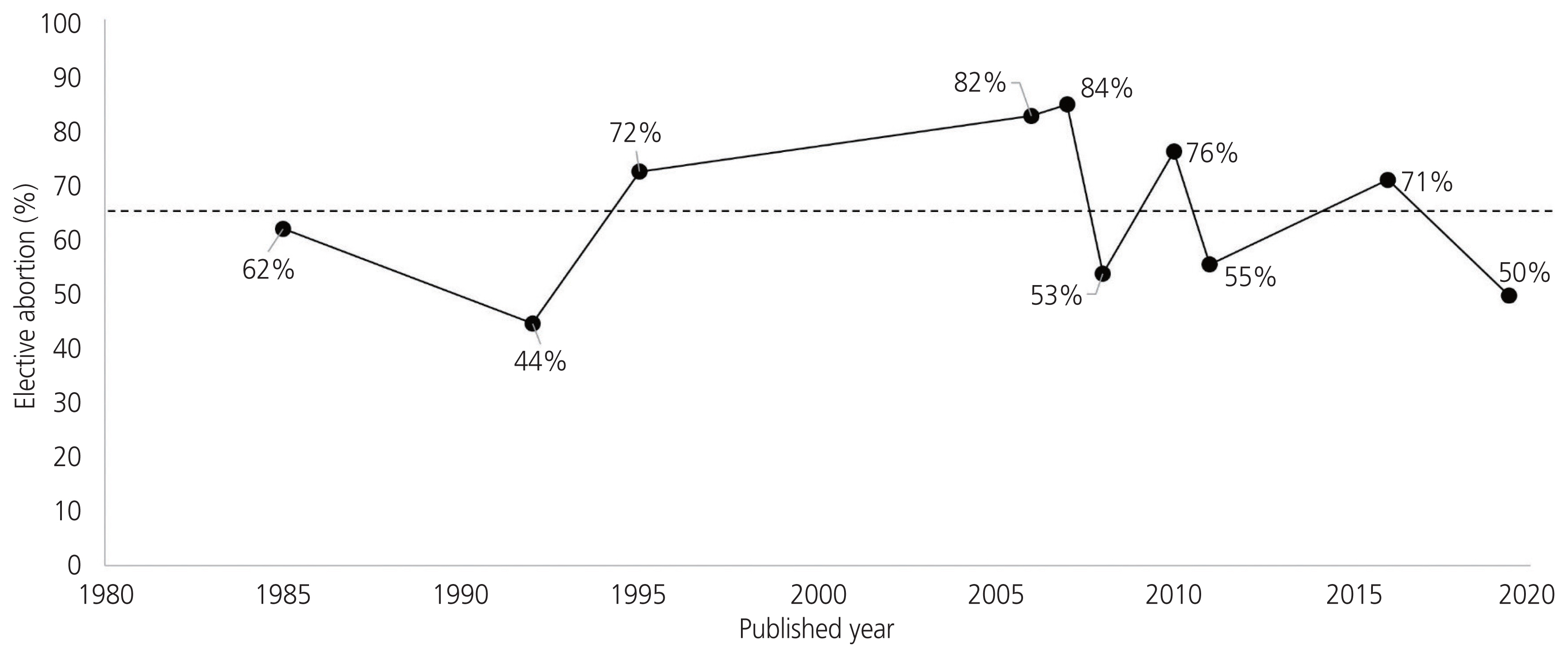
Ten eligible studies that combined 2,783 isotretinoin-exposed women were included in our study. The rate of MM weighted for the sample size was 15%. Three studies that included an unexposed comparison group were eligible for the meta-analysis. The pooled odds ratio of MM for isotretinoin-exposed women was 3.76. After 2006, the pooled odds ratio of MM for isotretinoin exposure was significantly lower at 1.04.
Conclusion
The current rate of MM in isotretinoin-exposed women was substantially lower after 2006.
Figure
Cited by 2 articles
-
Pregnancy and neonatal outcomes after periconceptional exposure to isotretinoin in Koreans
Eun-Hwan Cha, NaeRy Kim, Ho-Seok Kwak, Hae Ji Han, Sung Hong Joo, June-Seek Choi, Kyoung-Chul Chun, Young-Ah Kim, Jae-Whoan Koh, Jung Yeol Han
Obstet Gynecol Sci. 2022;65(2):166-175. doi: 10.5468/ogs.21354.Usefulness and limitations of Chat GPT in getting information on teratogenic drugs exposed in pregnancy
Jung Yeol Han
Obstet Gynecol Sci. 2025;68(1):1-8. doi: 10.5468/ogs.24231.
Reference
-
References
1. Layton A. The use of isotretinoin in acne. Dermatoendocrinol. 2009; 1:162–9.
Article2. Lammer EJ, Chen DT, Hoar RM, Agnish ND, Benke PJ, Braun JT, et al. Retinoic acid embryopathy. N Engl J Med. 1985; 313:837–41.
Article3. Dai WS, LaBraico JM, Stern RS. Epidemiology of isotretinoin exposure during pregnancy. J Am Acad Dermatol. 1992; 26:599–606.
Article4. Davis WL, Jacoby BH, Farmer GR, Cooper OJ. Changes in cytosolic calcium, bleb formation, and cell death in neural crest cells treated with isotretinoin and 4-oxoisotretinoin. J Craniofac Genet Dev Biol. 1992; 11:105–18.5. United Kingdom Teratology Information Service (UKTIS). Use of isotretinoin in pregnancy [Internet]. London (UK): UKTIS;c2018. [cited 2020 Nov 20]. Available from: http://www.uktis.org./index.html .6. Nulman I, Berkovitch M, Klein J, Pastuszak A, Lester RS, Shear N, et al. Steady-state pharmacokinetics of isotretinoin and its 4-oxo metabolite: implications for fetal safety. J Clin Pharmacol. 1998; 38:926–30.
Article7. Rademaker M. Isotretinoin: dose, duration and relapse. What does 30 years of usage tell us? Australas J Dermatol. 2013; 54:157–62.
Article8. Torzecka JD, Dziankowska-Bartkowiak B, Gerlicz-Kowalczuk Z, Wozniacka A. The use of isotretinoin in low doses and unconventional treatment regimens in different types of acne: a literature review. Postepy Dermatol Alergol. 2017; 34:1–5.
Article9. Crijns I, Straus S, Luteijn M, Gispen-de Wied C, Raine J, de Jong-van den Berg L. Implementation of the harmonized EU isotretinoin Pregnancy Prevention Programme: a questionnaire survey among European regulatory agencies. Drug Saf. 2012; 35:27–32.10. Shin J, Cheetham TC, Wong L, Niu F, Kass E, Yoshinaga MA, et al. The impact of the iPLEDGE program on isotretinoin fetal exposure in an integrated health care system. J Am Acad Dermatol. 2011; 65:1117–25.
Article11. Teichert M, Visser LE, Dufour M, Rodenburg E, Straus SM, De Smet PA, et al. Isotretinoin use and compliance with the Dutch Pregnancy Prevention Programme: a retrospective cohort study in females of reproductive age using pharmacy dispensing data. Drug Saf. 2010; 33:315–26.12. Bacino CA, Firth HV, Wilkins-Haug L, TePas E. Birth defects: epidemiology, types, and patterns [Internet]. Waltham (MA): UpToDate;c2017. [cited 2020 Nov 20]. Available from: https://www.uptodate.com/contents/birth-defects-epidemiology-types-and-patterns .13. Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses [Internet]. Ottawa (CA): Ottawa Hospital Research Institute;c2011. [cited 2020 Nov 20]. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp .14. Heneghan C, Aronson JK, Spencer E, Holman B, Mahtani KR, Perera R, et al. Oral hormone pregnancy tests and the risks of congenital malformations: a systematic review and meta-analysis. F1000Res. 2018; 7:1725.
Article15. Bérard A, Azoulay L, Koren G, Blais L, Perreault S, Oraichi D. Isotretinoin, pregnancies, abortions and birth defects: a population-based perspective. Br J Clin Pharmacol. 2007; 63:196–205.
Article16. Cheetham TC, Wagner RA, Chiu G, Day JM, Yoshinaga MA, Wong L. A risk management program aimed at preventing fetal exposure to isotretinoin: retrospective cohort study. J Am Acad Dermatol. 2006; 55:442–8.
Article17. Garcia-Bournissen F, Tsur L, Goldstein LH, Staroselsky A, Avner M, Asrar F, et al. Fetal exposure to isotretinoin-an international problem. Reprod Toxicol. 2008; 25:124–8.
Article18. Henry D, Dormuth C, Winquist B, Carney G, Bugden S, Teare G, et al. Occurrence of pregnancy and pregnancy outcomes during isotretinoin therapy. CMAJ. 2016; 188:723–30.
Article19. Mitchell AA, Van Bennekom CM, Louik C. A pregnancy-prevention program in women of childbearing age receiving isotretinoin. N Engl J Med. 1995; 333:101–6.
Article20. Schaefer C, Meister R, Weber-Schoendorfer C. Isotretinoin exposure and pregnancy outcome: an observational study of the Berlin Institute for Clinical Teratology and Drug Risk Assessment in Pregnancy. Arch Gynecol Obstet. 2010; 281:221–7.
Article21. Zomerdijk IM, Ruiter R, Houweling LM, Herings RM, Sturkenboom MC, Straus SM, et al. Isotretinoin exposure during pregnancy: a population-based study in The Netherlands. BMJ Open. 2014; 4:e005602.
Article22. MacDonald SC, Cohen JM, Panchaud A, McElrath TF, Huybrechts KF, Hernández-Díaz S. Identifying pregnancies in insurance claims data: methods and application to retinoid teratogenic surveillance. Pharmacoepidemiol Drug Saf. 2019; 28:1211–21.
Article23. Tkachenko E, Singer S, Sharma P, Barbieri J, Mostaghimi A. US Food and Drug Administration reports of pregnancy and pregnancy-related adverse events associated with isotretinoin. JAMA Dermatol. 2019; 155:1175–9.
Article24. Kim NR, Yoon SR, Choi JS, Ahn HK, Lee SY, Hong DS, et al. Isotretinoin exposure in pregnant women in Korea. Obstet Gynecol Sci. 2108; 61:649–54.
Article25. Layton AM, Cunliffe WJ. Guidelines for optimal use of isotretinoin in acne. J Am Acad Dermatol. 1992; 27(6 Pt 2):S2–7.
Article26. Amichai B, Shemer A, Grunwald MH. Low-dose isotretinoin in the treatment of acne vulgaris. J Am Acad Dermatol. 2006; 54:644–6.
Article27. Hermes B, Praetel C, Henz BM. Medium dose isotretinoin for the treatment of acne. J Eur Acad Dermatol Venereol. 1998; 11:117–21.
Article28. Seukeran DC, Cunliffe WJ. Acne vulgaris in the elderly: the response to low-dose isotretinoin. Br J Dermatol. 1998; 139:99–101.
Article29. Abdelmaksoud A, Vojvodic A, Ayhan E, Dönmezdil S, Jovicevic TV, Vojvodic P, et al. Depression, isotretinoin, and folic acid: a practical review. Dermatol Ther. 2019; 32:e13104.
Article30. Kim HJ, Lee SM, Lee JS, Lee SY, Chung EH, Cho MK, et al. Homocysteine, folic acid, and vitamin B12 levels in patients on isotretinoin therapy for acne vulgaris: a meta-analysis. J Cosmet Dermatol. 2020; 19:736–45.
Article31. Kriangkrai R, Chareonvit S, Iseki S, Limwongse V. Pretreatment effect of folic acid on 13-cis-RA-induced cellular damage of developing midfacial processes in cultured rat embryos. Open Dent J. 2017; 11:200–12.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prenatal Maternal Risk Factors Contributing to Atopic Dermatitis: A Systematic Review and Meta-Analysis of Cohort Studies
- An Introduction of the Systematic Review and Meta-Analysis
- Systematic Review and Meta-analysis in Digestive Cancer Research
- Critical Appraisal of Systematic Review/Meta-analysis
- Introduction to systematic review and meta-analysis