Ann Pediatr Endocrinol Metab.
2019 Dec;24(4):243-247. 10.6065/apem.2019.24.4.243.
Application of body composition zones in boys with nonalcoholic fatty liver disease
- Affiliations
-
- 1Department of Pediatrics, Konkuk University Medical Center, Seoul, Korea. scchung@kuh.ac.kr
- 2Department of Pediatrics, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 3Konkuk University School of Medicine, Seoul, Korea.
- KMID: 2468726
- DOI: http://doi.org/10.6065/apem.2019.24.4.243
Abstract
- PURPOSE
Screening nonalcoholic fatty liver disease (NAFLD) by body mass index (BMI) as a single surrogate measure for obesity has limitations. We suggest considering body composition zones by drawing a body composition chart composed of body composition indices, including BMI and percent body fat (PBF), to visualize the risk of NAFLD in obese children and adolescents.
METHODS
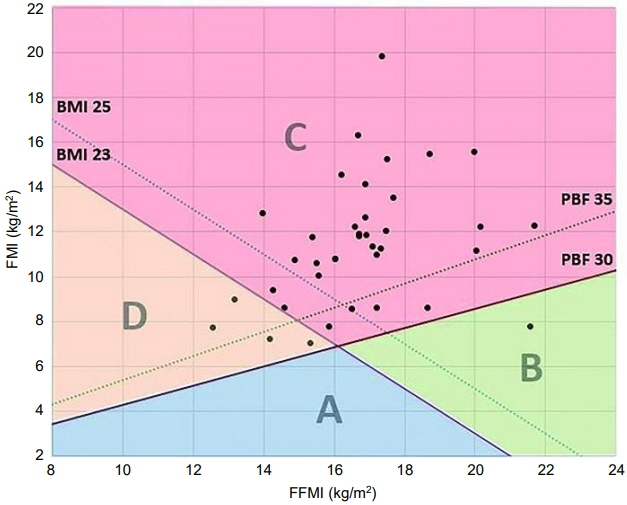
Thirty-eight boys diagnosed with NAFLD were selected retrospectively from patients who visited Konkuk University Medical Center from 2006 to 2015. They had gone through body composition analysis by bioelectrical impedance analysis (BIA), and biochemical analyses, including a liver function test (LFT) and lipid panel, were performed. Fat-free mass index (FFMI) and fat mass index (FMI) were calculated from body composition analysis and height. We plotted FFMI and FMI of patients on a body composition chart and classified the patients into zones A to D. In addition, we analyzed the correlations between LFT, lipid panel, and body composition indices.
RESULTS
Thirty-three of 38 boys (86.8%) were located in zone C, corresponding to high BMI and PBF. Four boys (10.5%) were located in zone D, which correlates with sarcopenic obesity. One boy located in zone B was a muscular adolescent. Alanine aminotransferase level was positively correlated with PBF, FMI, and BMI z-score.
CONCLUSION
Body composition zones on a body composition chart might be useful in risk assessment in obesity-related diseases such as NAFLD. Zones on a body composition chart could have practical applications, especially in sarcopenic obese children and adolescents.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Loomba R, Sirlin CB, Schwimmer JB, Lavine JE. Advances in pediatric nonalcoholic fatty liver disease. Hepatology. 2009; 50:1282–93.
Article2. Matthiessen J, Velsing Groth M, Fagt S, Biltoft-Jensen A, Stockmarr A, Andersen JS, et al. Prevalence and trends in overweight and obesity among children and adolescents in Denmark. Scand J Public Health. 2008; 36:153–60.
Article3. Chan C. Childhood obesity and adverse health effects in Hong Kong. Obes Rev. 2008; 9 Suppl 1:87–90.
Article4. Heymsfield SB, Gallagher D, Mayer L, Beetsch J, Pietrobelli A. Scaling of human body composition to stature: new insights into body mass index. Am J Clin Nutr. 2007; 86:82–91.
Article5. Okorodudu DO, Jumean MF, Montori VM, Romero-Corral A, Somers VK, Erwin PJ, et al. Diagnostic performance of body mass index to identify obesity as defined by body adiposity: a systematic review and meta-analysis. Int J Obes (Lond). 2010; 34:791–9.
Article6. Lim HS, Park YH, Suh K, Yoo MH, Park HK, Kim HJ, et al. Association between Sarcopenia, Sarcopenic Obesity, and Chronic Disease in Korean Elderly. J Bone Metab. 2018; 25:187–93.
Article7. Stenholm S, Harris TB, Rantanen T, Visser M, Kritchevsky SB, Ferrucci L. Sarcopenic obesity: definition, cause and consequences. Curr Opin Clin Nutr Metab Care. 2008; 11:693–700.
Article8. Chalasani N, Younossi Z, Lavine JE, Diehl AM, Brunt EM, Cusi K, et al. The diagnosis and management of non-alcoholic fatty liver disease: practice Guideline by the American Association for the Study of Liver Diseases, American College of Gastroenterology, and the American Gastroenterological Association. Hepatology. 2012; 55:2005–23.
Article9. Lee SY, Gallagher D. Assessment methods in human body composition. Curr Opin Clin Nutr Metab Care. 2008; 11:566–72.
Article10. Hattori K, Tatsumi N, Tanaka S. Assessment of body composition by using a new chart method. Am J Hum Biol. 1997; 9:573–8.
Article11. Park H, Park K, Kim MH, Kim GS, Chung S. Gender differences in relationship between fat-free mass index and fat mass index among Korean children using body composition chart. Yonsei Med J. 2011; 52:948–52.
Article12. Lee SH, Cho MH, Kim YH, Chung S. Two cases of successful type 2 diabetes control with lifestyle modification in children and adolescents. J Obes Metab Syndr. 2017; 26:71–5.
Article13. Park HW, Kim YH, Cho M, Kwak BO, Kim KS, Chung S. Adolescent build plotting on body composition chart and the type of diabetes mellitus. J Korean Med Sci. 2012; 27:1385–90.
Article14. Kim YH, Song MK, Chung S. Body composition analysis in newly diagnosed diabetic adolescent girls. J Korean Soc Pediatr Endocrinol. 2011; 16:172–7.
Article15. Park HW, Yoo HY, Kim CH, Kim H, Kwak BO, Kim KS, et al. Reference values of body composition indices: the Korean National Health and Nutrition Examination Surveys. Yonsei Med J. 2015; 56:95–102.
Article16. Huang JS, Barlow SE, Quiros-Tejeira RE, Scheimann A, Skelton J, Suskind D, et al. Childhood obesity for pediatric gastroenterologists. J Pediatr Gastroenterol Nutr. 2013; 56:99–109.
Article17. Steene-Johannessen J, Anderssen SA, Kolle E, Andersen LB. Low muscle fitness is associated with metabolic risk in youth. Med Sci Sports Exerc. 2009; 41:1361–7.
Article18. Benson AC, Torode ME, Singh MA. Muscular strength and cardiorespiratory fitness is associated with higher insulin sensitivity in children and adolescents. Int J Pediatr Obes. 2006; 1:222–31.
Article19. McCarthy HD, Samani-Radia D, Jebb SA, Prentice AM. Skeletal muscle mass reference curves for children and adolescents. Pediatr Obes. 2014; 9:249–59.
Article20. Schwimmer JB, Dunn W, Norman GJ, Pardee PE, Middleton MS, Kerkar N, et al. SAFETY study: alanine aminotransferase cutoff values are set too high for reliable detection of pediatric chronic liver disease. Gastroenterology. 2010; 138:1357–64. , 1364.e1-2.
Article21. Molleston JP, Schwimmer JB, Yates KP, Murray KF, Cummings OW, Lavine JE, et al. Histological abnormalities in children with nonalcoholic fatty liver disease and normal or mildly elevated alanine aminotransferase levels. J Pediatr. 2014; 164:707–13. e3.
Article22. Styne DM, Arslanian SA, Connor EL, Farooqi IS, Murad MH, Silverstein JH, et al. Pediatric obesity-assessment, treatment, and prevention: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2017; 102:709–57.
Article23. Lim JS, Hwang JS, Lee JA, Kim DH, Park KD, Jeong JS, et al. Cross-calibration of multi-frequency bioelectrical impedance analysis with eight-point tactile electrodes and dual-energy X-ray absorptiometry for assessment of body composition in healthy children aged 6-18 years. Pediatr Int. 2009; 51:263–8.24. Yu OK, Rhee YK, Park TS, Cha YS. Comparisons of obesity assessments in over-weight elementary students using anthropometry, BIA, CT and DEXA. Nutr Res Pract. 2010; 4:128–35.
Article25. Williams DP, Going SB, Lohman TG, Harsha DW, Srinivasan SR, Webber LS, et al. Body fatness and risk for elevated blood pressure, total cholesterol, and serum lipoprotein ratios in children and adolescents. Am J Public Health. 1992; 82:358–63.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Noninvasive serum biomarkers for liver steatosis in nonalcoholic fatty liver disease: Current and future developments
- Lean or Non-obese Nonalcoholic Fatty Liver Disease Patients: Are They Really Lean?
- Nonalcoholic fatty liver disease: pathogenesis and treatment
- Prevalence of the Nonalcoholic Fatty Liver Disease in Obese Children
- The Impact of Body Composition on the Prognosis of Nonalcoholic Fatty Liver Disease