J Pathol Transl Med.
2019 Mar;53(2):104-111. 10.4132/jptm.2018.11.10.
Intraoperative Frozen Cytology of Central Nervous System Neoplasms: An Ancillary Tool for Frozen Diagnosis
- Affiliations
-
- 1Department of Pathology, Gil Medical Center, Gachon University College of Medicine, Incheon, Korea. clara_nrk@gilhospital.com
- 2Department of Neurosurgery, Gil Medical Center, Gachon University College of Medicine, Incheon, Korea.
- 3Division of Medical Oncology, Department of Internal Medicine, Gil Medical Center, Gachon University College of Medicine, Incheon, Korea.
- 4Department of Radiology, Gil Medical Center, Gachon University College of Medicine, Incheon, Korea.
- 5Department of Radiation Oncology, Gil Medical Center, Gachon University College of Medicine, Incheon, Korea.
- KMID: 2465449
- DOI: http://doi.org/10.4132/jptm.2018.11.10
Abstract
- BACKGROUND
Pathologic diagnosis of central nervous system (CNS) neoplasms is made by comparing light microscopic, immunohistochemical, and molecular cytogenetic findings with clinicoradiologic observations. Intraoperative frozen cytology smears can improve the diagnostic accuracy for CNS neoplasms. Here, we evaluate the diagnostic value of cytology in frozen diagnoses of CNS neoplasms.
METHODS
Cases were selected from patients undergoing both frozen cytology and frozen sections. Diagnostic accuracy was evaluated.
RESULTS
Four hundred and fifty-four cases were included in this retrospective single-center review study covering a span of 10 years. Five discrepant cases (1.1%) were found after excluding 53 deferred cases (31 cases of tentative diagnosis, 22 cases of inadequate frozen sampling). A total of 346 cases of complete concordance and 50 cases of partial concordance were classified as not discordant cases in the present study. Diagnostic accuracy of intraoperative frozen diagnosis was 87.2%, and the accuracy was 98.8% after excluding deferred cases. Discrepancies between frozen and permanent diagnoses (n = 5, 1.1%) were found in cases of nonrepresentative sampling (n = 2) and misinterpretation (n = 3). High concordance was observed more frequently in meningeal tumors (97/98, 99%), metastatic brain tumors (51/52, 98.1%), pituitary adenomas (86/89, 96.6%), schwannomas (45/47, 95.8%), high-grade astrocytic tumors (47/58, 81%), low grade astrocytic tumors (10/13, 76.9%), non-neoplastic lesions (23/36, 63.9%), in decreasing frequency.
CONCLUSIONS
Using intraoperative cytology and frozen sections of CNS tumors is a highly accurate diagnostic ancillary method, providing subtyping of CNS neoplasms, especially in frequently encountered entities.
MeSH Terms
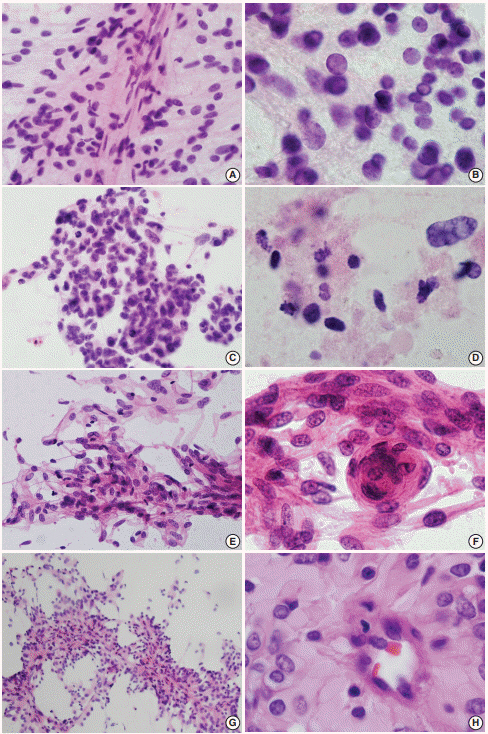
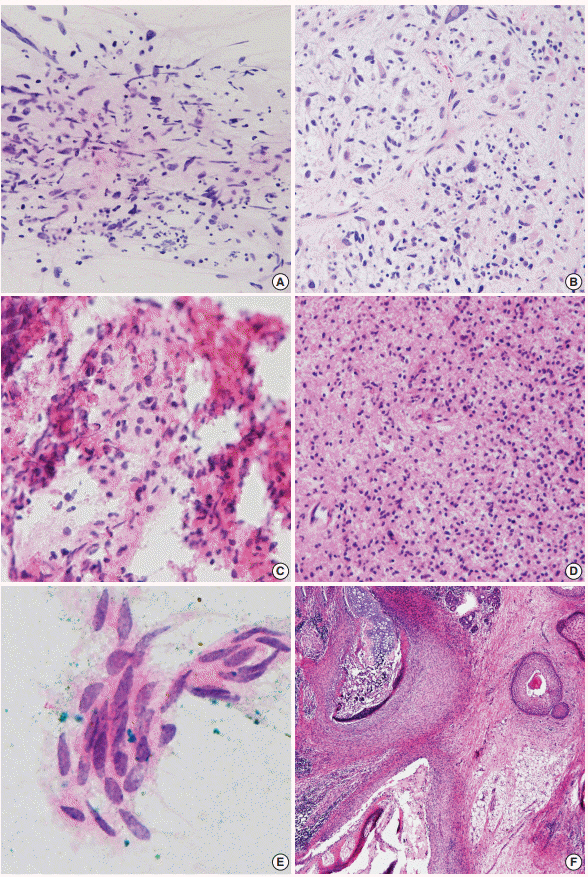
Figure
Cited by 1 articles
-
Intraoperative frozen cytology of intraosseous cystic meningioma in the sphenoid bone
Na Rae Kim, Gie-Taek Yie
J Pathol Transl Med. 2020;54(6):508-512. doi: 10.4132/jptm.2020.05.21.
Reference
-
1. Marshall LF, Adams H, Doyle D, Graham DI. The histological accuracy of the smear technique for neurosurgical biopsies. J Neurosurg. 1973; 39:82–8.
Article2. Eisenhardt L, Cushing H. Diagnosis of intracranial tumors by supravital technique. Am J Pathol. 1930; 6:541–52.3. Gal AA, Cagle PT. The 100-year anniversary of the description of the frozen section procedure. JAMA. 2005; 294:3135–7.
Article4. Cahill EM, Hidvegi DF. Crush preparations of lesions of the central nervous system: a useful adjunct to the frozen section. Acta Cytol. 1985; 29:279–85.5. Louis DN, Ohgaki H, Wiestler OD, Cavenee WK. WHO classification of tumours of the central nervous system. Lyon: IARC Press;2016. 4th.6. Louis DN, Ohgaki H, Wiestler OD, Cavenee WK. WHO classification of tumours of the central nervous system. Lyon: IARC Press;2007.7. Folkerth RD. Smears and frozen sections in the intraoperative diagnosis of central nervous system lesions. Neurosurg Clin N Am. 1994; 5:1–18.
Article8. Rushing EJ, Wesseling P. Towards an integrated morphological and molecular WHO diagnosis of central nervous system tumors: a paradigm shift. Curr Opin Neurol. 2015; 28:628–32.9. Inagawa H, Ishizawa K, Hirose T. Qualitative and quantitative analysis of cytologic assessment of astrocytoma, oligodendroglioma and oligoastrocytoma. Acta Cytol. 2007; 51:900–6.
Article10. Kang M, Kim NR, Chung DH, Yoo CJ. Crush cytologic findings of a cerebral granular cell astrocytoma. Acta Cytol. 2012; 56:571–5.
Article11. Shioyama T, Muragaki Y, Maruyama T, Komori T, Iseki H. Intraoperative flow cytometry analysis of glioma tissue for rapid determination of tumor presence and its histopathological grade: clinical article. J Neurosurg. 2013; 118:1232–8.12. Lampert PW, Davis RL. Delayed effects of radiation on the human central nervous system: “early” and “late” delayed reactions. Neurology. 1964; 14:912–7.
Article13. Lee S, Kim NR, Chung DH, Yee GT, Cho HY. Squash cytology of a dural-based high-grade chondrosarcoma may mimic that of glioblastoma in the central nervous system. Acta Cytol. 2015; 59:219–24.
Article14. Plesec TP, Prayson RA. Frozen section discrepancy in the evaluation of central nervous system tumors. Arch Pathol Lab Med. 2007; 131:1532–40.
Article15. Lee HS, Tihan T. The basics of intraoperative diagnosis in neuropathology. Surg Pathol Clin. 2015; 8:27–47.
Article16. Yamada SM, Murakami H, Tomita Y, et al. Glioblastoma multiforme versus pleomorphic xanthoastrocytoma with anaplastic features in the pathological diagnosis: a case report. Diagn Pathol. 2016; 11:65.
Article17. Seok JY, Kim NR, Cho HY, Chung DH, Yee GT, Kim EY. Crush cytology of microcystic meningioma with extensive sclerosis. Korean J Pathol. 2014; 48:77–80.
Article18. Jeong J, Kim NR, Lee SG. Crush cytology of a primary intraspinal rhabdoid papillary meningioma: a case report. Acta Cytol. 2013; 57:528–33.
Article19. Raisanen J, Hatanpaa KJ, Mickey BE, White CL 3rd. Atypical teratoid/rhabdoid tumor: cytology and differential diagnosis in adults. Diagn Cytopathol. 2004; 31:60–3.
Article20. Kobayashi S. Meningioma, neurilemmoma and astrocytoma specimens obtained with the squash method for cytodiagnosis: a cytologic and immunochemical study. Acta Cytol. 1993; 37:913–22.21. Kim NR, Suh YL. Primary intrasellar schwannoma: a case report. Korean J Pathol. 2002; 36:274–7.22. Plesec TP, Prayson RA. Frozen section discrepancy in the evaluation of nonneoplastic central nervous system samples. Ann Diagn Pathol. 2009; 13:359–66.
Article23. Can B, Akpolat I, Meydan D, Üner A, Kandemir B, Söylemezoğlu F. Fine-needle aspiration cytology of metastatic oligodendroglioma: case report and literature review. Acta Cytol. 2012; 56:97–103.
Article24. Hernández-Martínez SJ, De Leíja-Portilla JO, Medellín-Sánchez R. Cytologic features during intraoperative assessment of central neurocytoma: a report of three cases and review of the literature. Acta Cytol. 2013; 57:400–5.
Article25. Deb P, Manu V, Pradeep H, Bhatoe HS. Intraparenchymal clear cell ependymoma. J Cytol. 2011; 28:73–6.
Article26. Chaudhuri PM, Chaudhuri S, Chakrabarty D, et al. Squash cytology of tanycytic ependymoma: a report of two cases. Diagn Cytopathol. 2017; 45:270–3.
Article27. Wang M, He X, Chang Y, Sun G, Thabane L. A sensitivity and specificity comparison of fine needle aspiration cytology and core needle biopsy in evaluation of suspicious breast lesions: a systematic review and meta-analysis. Breast. 2017; 31:157–66.
Article28. Mahe E, Ara S, Bishara M, et al. Intraoperative pathology consultation: error, cause and impact. Can J Surg. 2013; 56:E13–8.
Article29. Monabati A, Kumar PV, Kamkarpour A. Intraoperative cytodiagnosis of metastatic brain tumors confused clinically with brain abscess: a report of three cases. Acta Cytol. 2000; 44:437–41.30. Chand P, Amit S, Gupta R, Agarwal A. Errors, limitations, and pitfalls in the diagnosis of central and peripheral nervous system lesions in intraoperative cytology and frozen sections. J Cytol. 2016; 33:93–7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Continuing Value of Ultrastructural Observation in Central Nervous System Neoplasms in Children
- Quality Assurance of Intraoperative Consultation Review Analysis of 2,392 frozen sections
- Intraoperative consultation for ovarian tumors
- The Role of Fine-Needle Aspiration Cytology and Frozen Section in the Operative Management of Thyroid Nodule
- Cytologic Features of Intracranial Germ Cell Tumors in Crush Preparation