J Korean Soc Radiol.
2019 Nov;80(6):1214-1228. 10.3348/jksr.2019.80.6.1214.
Correlation between Carotid Arterial Calcium Score and Silent Cerebrovascular Lesions in Obstructive Sleep Apnea Patients: by Using Upper Airway CT and Brain MRI
- Affiliations
-
- 1Department of Radiology, Dong-A University College of Medicine, Busan, Korea. medcarrot@dau.ac.kr
- 2Department of Otorhinolaryngology-Head and Neck Surgery, Dong-A University College of Medicine, Busan, Korea.
- 3Department of Neurology, Dong-A University College of Medicine, Busan, Korea.
- 4Department of Oral and Maxillofacial Surgery, Dong-A University College of Medicine, Busan, Korea.
- 5Department of Neurosurgery, Dong-A University College of Medicine, Busan, Korea.
- KMID: 2464918
- DOI: http://doi.org/10.3348/jksr.2019.80.6.1214
Abstract
- PURPOSE
To investigate the relationship between carotid arterial calcium score (CarACS) and silent cerebrovascular lesions in patients with obstructive sleep apnea (OSA).
MATERIALS AND METHODS
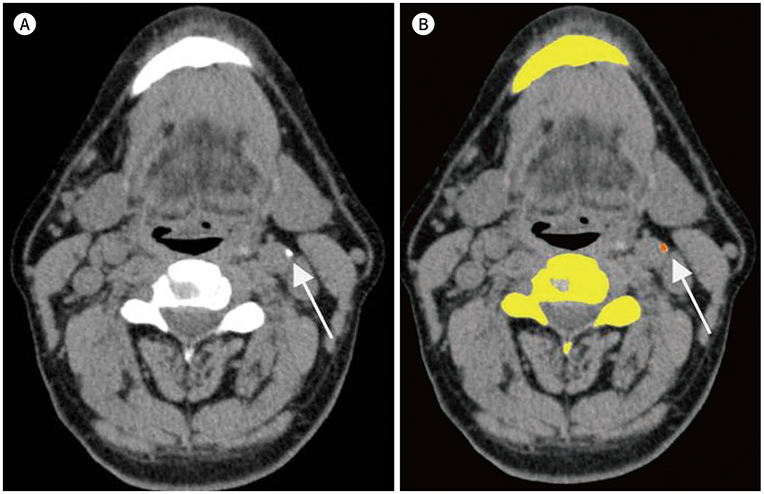
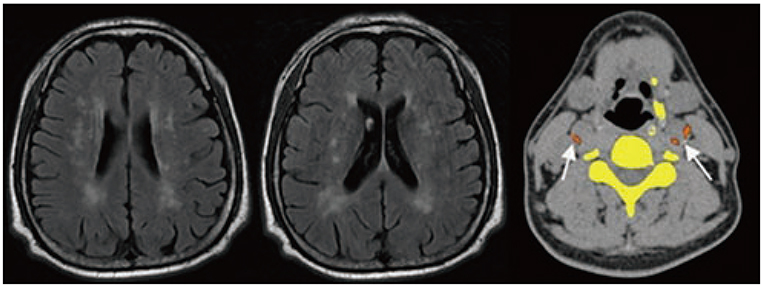
This study involved retrospective evaluation of 60 OSA patients who underwent both upper airway CT and brain MRI. Using polysomnography, several indicators, including apnea index (AI), were used to evaluate the relationship between OSA and silent cerebrovascular lesions. The CarACS was quantified on CT imaging using the modified Agatston method. Silent cerebrovascular lesions were evaluated on brain MRI by grading periventricular hyperintensity (PVH). Various clinical characteristics, including age, were analyzed in each patient.
RESULTS
The number of patients per PVH grade 0, 1, 2, 3, and 4 was 26 (43.3%), 14 (23.3%), 14 (23.3%), 4 (6.7%), and 2 (3.3%), respectively. The mean age, hypertension, smoking status, AI, and CarACS were significantly different among PVH groups (Ps < 0.05). In univariate analysis, the presence of carotid arterial calcification (β = 0.483, p < 0.01), CarACS (β = 0.482, p < 0.01), and age (β = 0.360, p < 0.01) showed a significant association with PVH grade. The mean AI and lowest O₂ saturation had statistically weak associations with PVH grade (β = 0.267, p < 0.01; β = −0.219, p < 0.14, respectively). In multivariate analysis, CarACS was the only factor affecting PVH grade (p < 0.04).
CONCLUSION
CarACS is associated with the severity of silent cerebrovascular lesions. Therefore, additional analysis of CarACS in OSA patients may provide more information on their cerebrovascular status.
MeSH Terms
Figure
Reference
-
1. Senaratna CV, Perret JL, Lodge CJ, Lowe AJ, Campbell BE, Matheson MC, et al. Prevalence of obstructive sleep apnea in the general population: a systematic review. Sleep Med Rev. 2017; 34:70–81.2. Dong R, Dong Z, Liu H, Shi F, Du J. Prevalence, risk factors, outcomes, and treatment of obstructive sleep apnea in patients with cerebrovascular disease: a systemic review. J Stroke Cerebrovasc Dis. 2018; 27:1471–1480.3. Gottlieb DJ, Yenokyan G, Newman AB, O'Connor GT, Punjabi NM, Quan SF, et al. Prospective study of obstructive sleep apnea and incident coronary heart disease and heart failure: the sleep heart health study. Circulation. 2010; 122:352–360.4. Beaudin AE, Waltz X, Hanly PJ, Poulin MJ. Impact of obstructive sleep apnoea and intermittent hypoxia on cardiovascular and cerebrovascular regulation. Exp Physiol. 2017; 102:743–763.5. Munoz R, Duran-Cantolla J, Martínez-Vila E, Gallego J, Rubio R, Aizpuru F, et al. Severe sleep apnea and risk of ischemic stroke in the elderly. Stroke. 2006; 37:2317–2321.6. Vermeer SE, Hollander M, Van Dijk EJ, Hofman A, Koudstaal PJ, Breteler MM. Rotterdam Scan Study. Silent brain infarcts and white matter lesions increase stroke risk in the general population: the Rotterdam Scan Study. Stroke. 2003; 34:1126–1129.7. Smith EE, Saposnik G, Biessels GJ, Doubal FN, Fornage M, Gorelick PB, et al. Prevention of stroke in patients with silent cerebrovascular disease: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2017; 48:e44–e71.8. Robbins J, Redline S, Ervin A, Walsleben JA, Ding J, Nieto FJ. Associations of sleep-disordered breathing and cerebral changes on MRI. J Clin Sleep Med. 2005; 1:159–165.9. Kim H, Yun CH, Thomas RJ, Lee SH, Seo HS, Cho ER, et al. Obstructive sleep apnea as a risk factor for cerebral white matter change in a middle-aged and older general population. Sleep. 2013; 36:709–715.10. Nishibayashi M, Miyamoto M, Miyamoto T, Suzuki K, Hirata K. Correlation between severity of obstructive sleep apnea and prevalence of silent cerebrovascular lesions. J Clin Sleep Med. 2008; 4:242–247.11. Chousangsuntorn K, Bhongmakapat T, Apirakkittikul N, Sungkarat W, Supakul N, Laothamatas J. Computed tomography characterization and comparison with polysomnography for obstructive sleep apnea evaluation. J Oral Maxillofac Surg. 2018; 76:854–872.12. Tsuda H, Almeida FR, Tsuda T, Moritsuchi Y, Lowe AA. Cephalometric calcified carotid artery atheromas in patients with obstructive sleep apnea. Sleep Breath. 2010; 14:365–370.13. Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990; 15:827–832.14. Mahabadi AA, Möhlenkamp S, Lehmann N, Kälsch H, Dykun I, Pundt N, et al. CAC score improves coronary and CV risk assessment above statin indication by ESC and AHA/ACC primary prevention guidelines. JACC Cardiovasc Imaging. 2017; 10:143–153.15. Denzel C, Lell M, Maak M, Höckl M, Balzer K, Müller KM, et al. Carotid artery calcium: accuracy of a calcium score by computed tomography-an in vitro study with comparison to sonography and histology. Eur J Vasc Endovasc Surg. 2004; 28:214–220.16. Miralles M, Merino J, Busto M, Perich X, Barranco C, Vidal-Barraquer F. Quantification and characterization of carotid calcium with multi-detector CT-angiography. Eur J Vasc Endovasc Surg. 2006; 32:561–567.17. Koh TK, Kang EJ, Bae WY, Kim SW, Kim CH, Koo SK, et al. Quantitative analysis of carotid arterial calcification using airway CT in obstructive sleep apnea. Auris Nasus Larynx. 2018; 12. 6. [Epub]. Available at. https://doi.org/10.1016/j.anl.2018.11.015.18. Bos D, Ikram MA, Elias-Smale SE, Krestin GP, Hofman A, Witteman JC, et al. Calcification in major vessel beds relates to vascular brain disease. Arterioscler Thromb Vasc Biol. 2011; 31:2331–2337.19. Fukuda H, Kobayashi S, Okada K, Tsunematsu T. Frontal white matter lesions and dementia in lacunar infarction. Stroke. 1990; 21:1143–1149.20. Fukuda H, Kitani M. Differences between treated and untreated hypertensive subjects in the extent of periventricular hyperintensities observed on brain MRI. Stroke. 1995; 26:1593–1597.21. Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991; 14:540–545.22. Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM, Mohsenin V. Obstructive sleep apnoea as a risk factor for stroke and death. N Engl J Med. 2005; 353:2034–2041.23. Lui MM, Sau-Man M. OSA and atherosclerosis. J Thorac Dis. 2012; 4:164–172.24. Davies CW, Crosby JH, Mullins RL, Traill ZC, Anslow P, Davies RJ, et al. Case control study of cerebrovascular damage defined by magnetic resonance imaging in patients with OSA and normal matched control subjects. Sleep. 2001; 24:715–720.25. Kiernan TE, Capampangan DJ, Hickey MG, Pearce LA, Aguilar MI. Sleep apnea and white matter disease in hypertensive patients: a case series. Neurologist. 2011; 17:289–291.26. Gunbatar H, Bulut MD, Ekin S, Sertogullarindan B, Bora A, Yavuz A, et al. A silent pre-stroke damage: obstructive sleep apnea syndrome. Int J Clin Exp Med. 2016; 9:3481–3488.27. Jennum P, Børgesen SE. Intracranial pressure and obstructive sleep apnea. Chest. 1989; 95:279–283.28. Klingelhöfer J, Hajak G, Sander D, Schulz-Varszegi M, Rüther E, Conrad B. Assessment of intracranial hemodynamics in sleep apnea syndrome. Stroke. 1992; 23:1427–1433.29. Patel SK, Hanly PJ, Smith EE, Chan W, Coutts SB. Nocturnal hypoxemia is associated with white matter hyperintensities in patients with a minor stroke or transient ischemic attack. J Clin Sleep Med. 2015; 11:1417–1424.30. Zuurbier LA, Vernooij MW, Luik AI, Kocevska D, Hofman A, Whitmore H, et al. Apnea-hypopnea index, nocturnal arousals, oxygen desaturation and structural brain changes: a population-based study. Neurobiol Sleep Circadian Rhythms. 2016; 1:1–7.31. De Leeuw FE, De Groot JC, Bots ML, Witteman JC, Oudkerk M, Hofman A. Carotid atherosclerosis and cerebral white matter lesions in a population based magnetic resonance imaging study. J Neurol. 2000; 247:291–296.32. Hougaku H, Matsumoto M, Handa N, Maeda H, Itoh T, Tsukamoto Y, et al. Asymptomatic carotid lesions and silent cerebral infarction. Stroke. 1994; 25:566–570.33. Shaalan WE, Cheng H, Gewertz B, McKinsey JF, Schwartz LB, Katz D, et al. Degree of carotid plaque calcification in relation to symptomatic outcome and plaque inflammation. J Vasc Surg. 2004; 40:262–269.34. Fanning NF, Walters TD, Fox AJ, Symons SP. Association between calcification of the cervical carotid artery bifurcation and white matter ischemia. AJNR Am J Neuroradiol. 2006; 27:378–383.35. De Weert TT, Cakir H, Rozie S, Cretier S, Meijering E, Dippel DW, et al. Intracranial internal carotid artery calcifications: association with vascular risk factors and ischemic cerebrovascular disease. AJNR Am J Neuroradiol. 2009; 30:177–184.36. Bos D, Van der Rijk MJ, Geeraedts TE, Hofman A, Krestin GP, Witteman JC, et al. Intracranial carotid artery atherosclerosis: prevalence and risk factors in the general population. Stroke. 2012; 43:1878–1884.37. Cohen SN, Friedlander AH, Jolly DA, Date L. Carotid calcification on panoramic radiographs: an important marker for vascular risk. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002; 94:510–514.38. Shamsuzzaman AS, Gersh BJ, Somers VK. Obstructive sleep apnea: implications for cardiac and vascular disease. JAMA. 2003; 290:1906–1914.39. Mohsenin V, Culebras A. Sleep-related breathing disorders and risk of stroke editorial comment: balancing sleep and breathing. Stroke. 2001; 32:1271–1278.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Upper airway studies in patients with obstructive sleep apnea syndrome
- Pathogenesis of Obstructive Sleep Apnea
- The Role of Endothelin-1 in Obstructive Sleep Apnea Syndrome and Pulmonary Hypertension
- Two Cases of Pediatric Obstructive Hypoventilation Managed with Upper Airway Surgery
- Upper airway myofunctional exercise: a systematic review