Cancer Res Treat.
2019 Oct;51(4):1324-1335. 10.4143/crt.2018.653.
The Feasibility of Spinal Stereotactic Radiosurgery for Spinal Metastasis with Epidural Cord Compression
- Affiliations
-
- 1Department of Radiation Oncology, Seoul National University College of Medicine, Seoul, Korea. jinho.kim.md@gmail.com
- 2Center for Precision Medicine, Seoul National University Hospital, Seoul, Korea.
- 3Department of Radiation Oncology, Graduate School of Medicine, Ewha Womans University, Seoul, Korea.
- 4Department of Radiation Oncology, Ewha Womans University College of Medicine, Seoul, Korea.
- 5Institute of Radiation Medicine, Seoul National University Medical Research Center, Seoul, Korea.
- 6Cancer Research Institute, Seoul National University, Seoul, Korea.
- KMID: 2460582
- DOI: http://doi.org/10.4143/crt.2018.653
Abstract
- PURPOSE
The purpose of this study was to investigate the effectiveness and safety of spinal stereotactic radiosurgery (SRS) in treating spinal metastasis with epidural spinal cord compression (ESCC).
MATERIALS AND METHODS
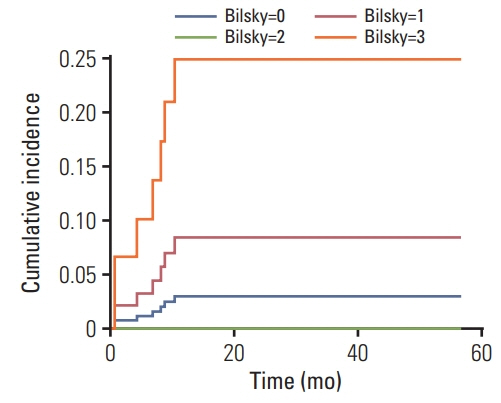
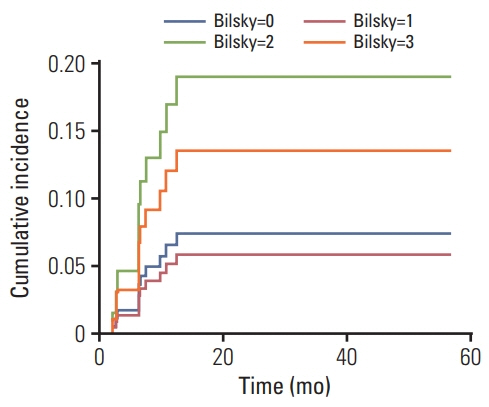
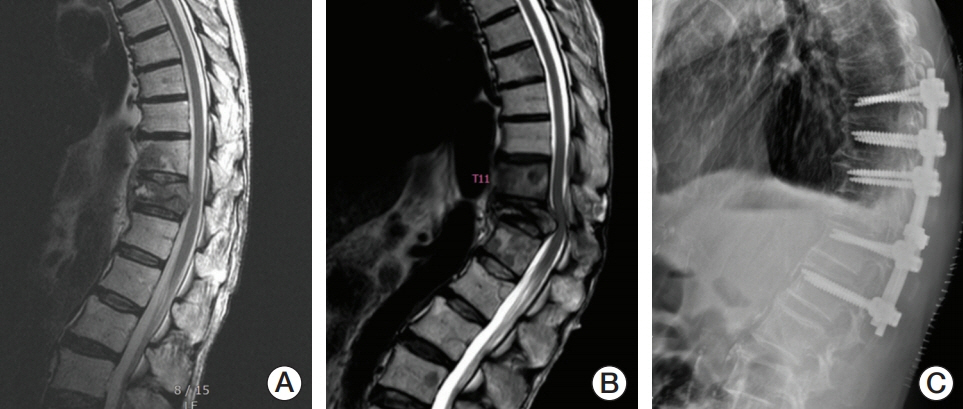
During 2013-2016, 149 regions of spinal metastasis in 105 patients treated with single-fraction (12-24 Gy) spinal SRS were reviewed. Cord compression of Bilsky grade 2 (with visible cerebrospinal fluid [CSF]) or 3 (no visible CSF) was defined as ESCC. Local progression (LP) and vertebral compression fracture (VCF) rates after SRS were evaluated using multivariate competing-risk regression analysis.
RESULTS
The 1-year cumulative incidences of LP for Bilsky grades 0 (n=80), 1 (n=39), 2 (n=21), and 3 (n=9) were 3.0%, 8.4%, 0%, and 24.9%, respectively. Bilsky grade 2 ESCC did not significantly increase the LP rate (no LP for grade 2). The 1-year cumulative incidences of VCF for Bilsky grades 0, 1, 2, and 3 were 6.6%, 5.2%, 17.1%, and 12.1%, respectively. ESCC may increase VCF risk (subhazard ratio [SHR] for grade 2, 5.368; p=0.035; SHR for grade 3, 2.215; p=0.460). Complete or partial pain response rates after SRS were 79%, 78%, 53%, and 63% for Bilsky grades 0, 1, 2, and 3, respectively (p=0.008). No neurotoxicity of grade ≥ 3 was observed.
CONCLUSION
Spinal SRS for spinal metastasis with Bilsky grade 2 ESCC did not increase the LP rate, was not associated with severe neurotoxicity, and showed moderate VCF and pain response rates. Bilsky grade 3 had a high LP rate.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Byrne TN. Spinal cord compression from epidural metastases. N Engl J Med. 1992; 327:614–9.
Article2. Patchell RA, Tibbs PA, Regine WF, Payne R, Saris S, Kryscio RJ, et al. Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: a randomised trial. Lancet. 2005; 366:643–8.
Article3. Pan H, Simpson DR, Mell LK, Mundt AJ, Lawson JD. A survey of stereotactic body radiotherapy use in the United States. Cancer. 2011; 117:4566–72.
Article4. Yu JI, Park HC, Ahn YC, Chung Y, Koom WS, Song SY. Variation in practice patterns of Korean radiation oncologists for spine metastasis between 2009 and 2014. Cancer Res Treat. 2016; 48:1102–9.
Article5. Yamada Y, Katsoulakis E, Laufer I, Lovelock M, Barzilai O, McLaughlin LA, et al. The impact of histology and delivered dose on local control of spinal metastases treated with stereotactic radiosurgery. Neurosurg Focus. 2017; 42:E6.
Article6. Cunha MV, Al-Omair A, Atenafu EG, Masucci GL, Letourneau D, Korol R, et al. Vertebral compression fracture (VCF) after spine stereotactic body radiation therapy (SBRT): analysis of predictive factors. Int J Radiat Oncol Biol Phys. 2012; 84:e343–9.
Article7. Kirkpatrick JP, van der Kogel AJ, Schultheiss TE. Radiation dose-volume effects in the spinal cord. Int J Radiat Oncol Biol Phys. 2010; 76(3 Suppl):S42–9.
Article8. Cox BW, Spratt DE, Lovelock M, Bilsky MH, Lis E, Ryu S, et al. International Spine Radiosurgery Consortium consensus guidelines for target volume definition in spinal stereotactic radiosurgery. Int J Radiat Oncol Biol Phys. 2012; 83:e597–605.
Article9. Bilsky MH, Laufer I, Fourney DR, Groff M, Schmidt MH, Varga PP, et al. Reliability analysis of the epidural spinal cord compression scale. J Neurosurg Spine. 2010; 13:324–8.
Article10. Fisher CG, DiPaola CP, Ryken TC, Bilsky MH, Shaffrey CI, Berven SH, et al. A novel classification system for spinal instability in neoplastic disease: an evidence-based approach and expert consensus from the Spine Oncology Study Group. Spine (Phila Pa 1976). 2010; 35:E1221–9.11. Cox JD, Stetz J, Pajak TF. Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int J Radiat Oncol Biol Phys. 1995; 31:1341–6.
Article12. Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999; 94:496–509.
Article13. Wang XS, Rhines LD, Shiu AS, Yang JN, Selek U, Gning I, et al. Stereotactic body radiation therapy for management of spinal metastases in patients without spinal cord compression: a phase 1-2 trial. Lancet Oncol. 2012; 13:395–402.
Article14. St Clair WH, Arnold SM, Sloan AE, Regine WF. Spinal cord and peripheral nerve injury: current management and investigations. Semin Radiat Oncol. 2003; 13:322–32.15. Laufer I, Rubin DG, Lis E, Cox BW, Stubblefield MD, Yamada Y, et al. The NOMS framework: approach to the treatment of spinal metastatic tumors. Oncologist. 2013; 18:744–51.
Article16. Suppli MH, Af Rosenschold PM, Pappot H, Dahl B, Morgen SS, Vogelius IR, et al. Stereotactic radiosurgery versus decompressive surgery followed by postoperative radiotherapy for metastatic spinal cord compression (STEREOCORD): Study protocol of a randomized non-inferiority trial. J Radiosurg SBRT. 2016; 4:S1–9.17. Pessina F, Navarria P, Riva M, Franceschini D, Nibali MC, Fornari M, et al. Long-term follow-up of patients with metastatic epidural spinal cord compression from breast cancer treated with surgery followed by radiotherapy. World Neurosurg. 2018; 110:e281–6.
Article18. Ghia AJ, Guha-Thakurta N, Hess K, Yang JN, Settle SH, Sharpe HJ, et al. Phase 1 study of spinal cord constraint relaxation with single session spine stereotactic radiosurgery in the primary management of patients with inoperable, previously unirradiated metastatic epidural spinal cord compression. Int Radiat Oncol Biol Phys. 2018; 102:1481–8.
Article19. Vellayappan BA, Kumar N, Chang EL, Sahgal A, Sloan AE, Lo SS. Novel multidisciplinary approaches in the management of metastatic epidural spinal cord compression. Future Oncol. 2018; 14:1665–8.
Article20. Park SJ, Lee CS, Chung SS. Surgical results of metastatic spinal cord compression (MSCC) from non-small cell lung cancer (NSCLC): analysis of functional outcome, survival time, and complication. Spine J. 2016; 16:322–8.
Article21. Husain ZA, Sahgal A, De Salles A, Funaro M, Glover J, Hayashi M, et al. Stereotactic body radiotherapy for de novo spinal metastases: systematic review. J Neurosurg Spine. 2017; 27:295–302.
Article22. Spratt DE, Beeler WH, de Moraes FY, Rhines LD, Gemmete JJ, Chaudhary N, et al. An integrated multidisciplinary algorithm for the management of spinal metastases: an International Spine Oncology Consortium report. Lancet Oncol. 2017; 18:e720–30.
Article23. Roodman GD. Mechanisms of bone metastasis. N Engl J Med. 2004; 350:1655–64.
Article24. Costelloe CM, Chuang HH, Madewell JE, Ueno NT. Cancer response criteria and bone metastases: RECIST 1.1, MDA and PERCIST. J Cancer. 2010; 1:80–92.
Article25. Virk MS, Han JE, Reiner AS, McLaughlin LA, Sciubba DM, Lis E, et al. Frequency of symptomatic vertebral body compression fractures requiring intervention following single-fraction stereotactic radiosurgery for spinal metastases. Neurosurg Focus. 2017; 42:E8.
Article26. Al-Omair A, Smith R, Kiehl TR, Lao L, Yu E, Massicotte EM, et al. Radiation-induced vertebral compression fracture following spine stereotactic radiosurgery: clinicopathological correlation. J Neurosurg Spine. 2013; 18:430–5.
Article27. Sahgal A, Atenafu EG, Chao S, Al-Omair A, Boehling N, Balagamwala EH, et al. Vertebral compression fracture after spine stereotactic body radiotherapy: a multi-institutional analysis with a focus on radiation dose and the spinal instability neoplastic score. J Clin Oncol. 2013; 31:3426–31.
Article28. Evans JD, Brown PD, Olivier KR. Stereotactic spinal radiosurgery and delayed vertebral fracture risk. Adv Radiat Oncol. 2019; 4:20–5.
Article29. Boyce-Fappiano D, Elibe E, Schultz L, Ryu S, Siddiqui MS, Chetty I, et al. Analysis of the factors contributing to vertebral compression fractures after spine stereotactic radiosurgery. Int J Radiat Oncol Biol Phys. 2017; 97:236–45.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Contemporary treatment with radiosurgery for spine metastasis and spinal cord compression in 2015
- Novalis Stereotactic Radiosurgery for Spinal Dural Arteriovenous Fistula
- The Role of Stereotactic Radiosurgery in Metastasis to the Spine
- Treatment of Spinal Epidural Metastasis
- Review of Stereotactic Radiosurgery for Intramedullary Spinal Lesions