Yonsei Med J.
2019 Oct;60(10):960-968. 10.3349/ymj.2019.60.10.960.
Clinical Manifestations and Risk Factors of Anaphylaxis in Pollen-Food Allergy Syndrome
- Affiliations
-
- 1Department of Pediatrics, Hallym University Dongtan Sacred Heart Hospital, Hallym University College of Medicine, Hwaseong, Korea.
- 2Allergy and Clinical Immunology Research Center, Hallym University College of Medicine, Chuncheon, Korea. mdqueen@hallym.or.kr
- 3Department of Pediatrics, Eulji Hospital, Eulji University, Seoul, Korea.
- 4Department of Pediatrics, Korea University Anam Hospital, Korea University College of Medicine, Seoul, Korea. yoolina@korea.ac.kr
- 5Department of Otorhinolaryngology-Head and Neck Surgery, Hallym University Chuncheon Sacred Heart Hospital and Nano-Bio Regenerative Medical Institute, Hallym University College of Medicine, Chuncheon, Korea.
- 6Department of Pediatrics, Pediatric Allergy and Respiratory Center, Soonchunhyang University Seoul Hospital, Soonchunhyang University College of Medicine, Seoul, Korea.
- 7Department of Allergy and Clinical Immunology, Ajou University School of Medicine, Suwon, Korea.
- 8Lee & Hong ENT, Sleep and Cosmetic Center, Seongnam, Korea.
- 9Department of Pulmonology, Allergy and Critical Care Medicine, CHA Bundang Medical Center, CHA University, Seongnam, Korea.
- 10Department of Internal Medicine, Gyeongsang National University College of Medicine, Jinju, Korea.
- 11Department of Pediatrics, Gangneung Asan Hospital, University of Ulsan College of Medicine, Gangneung, Korea.
- 12Department of Otorhinolaryngology, Head and Neck Surgery, Dong-A University College of Medicine, Busan, Korea.
- 13Department of Internal Medicine, Soonchunhyang University Bucheon Hospital, Bucheon, Korea.
- 14Department of Pediatrics, Wonkwang University Sanbon Hospital, Wonkwang University College of Medicine, Gunpo, Korea.
- 15Department of Internal Medicine, Chonnam National University Hospital, Chonnam National University Medical School, Gwangju, Korea.
- 16Department of Internal Medicine, Jeju National University School of Medicine, Jeju, Korea.
- 17Department of Pediatrics, Inha University Hospital, Inha University College of Medicine, Incheon, Korea.
- 18Division of Pulmonology and Allergy, Department of Internal Medicine, Gil Medical Center, Gachon University College of Medicine, Incheon, Korea.
- 19Department of Otorhinolaryngology-Head and Neck Surgery, Chungnam National University College of Medicine, Daejeon, Korea.
- 20Department of Otorhinolaryngology-Head & Neck Surgery, Soonchunhyang University Gumi Hospital, Soonchunhyang University College of Medicine, Gumi, Korea.
- 21Department of Otorhinolaryngology-Head and Neck Surgery, Samsung Medical Center, School of Medicine, Sungkyunkwan University, Seoul, Korea.
- 22SCH Biomedical Informatics Research Unit, Soonchunhyang University Seoul Hospital, Seoul, Korea.
- 23Department of Pulmonology, Allergy and Critical Care Medicine, Hallym University Dongtan Sacred Heart Hospital, Hallym University College of Medicine, Hwaseong, Korea.
- KMID: 2459149
- DOI: http://doi.org/10.3349/ymj.2019.60.10.960
Abstract
- PURPOSE
Many studies have reported that pollen-food allergy syndrome (PFAS) can cause anaphylaxis. No comprehensive investigations into anaphylaxis in PFAS have been conducted, however. In this study, we investigated the clinical manifestations and risk factors for anaphylaxis in PFAS in Korean patients with pollinosis.
MATERIALS AND METHODS
Data were obtained from a nationwide cross-sectional study that previously reported on PFAS in Korean patients with pollinosis. Data from 273 patients with PFAS were collected, including demographics, list of culprit fruits and vegetables, and clinical manifestations of food allergy. We analyzed 27 anaphylaxis patients and compared them with patients with PFAS with oropharyngeal symptoms only (n=130).
RESULTS
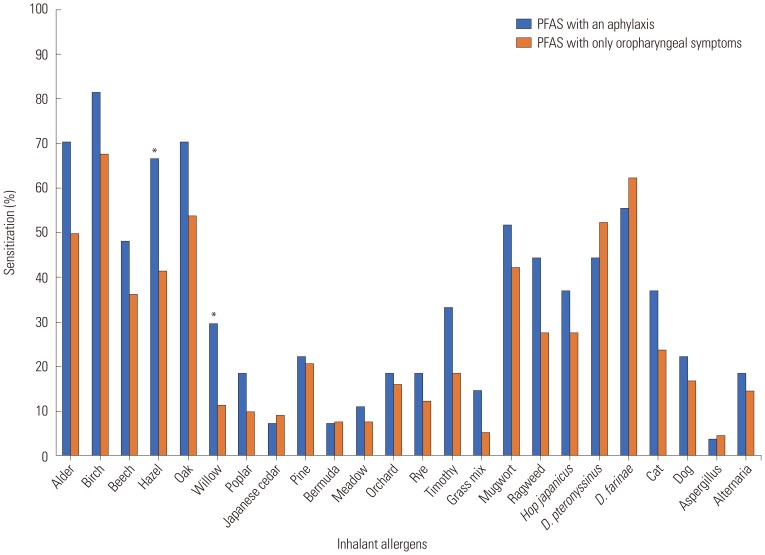
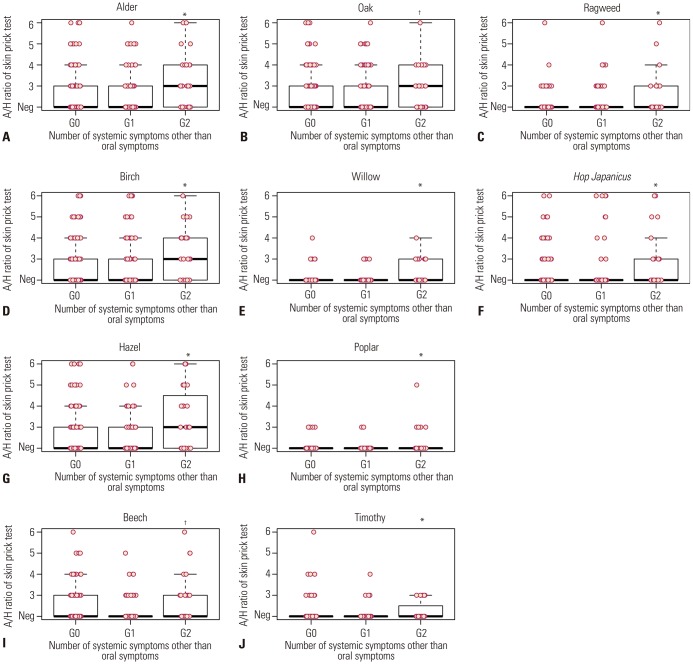
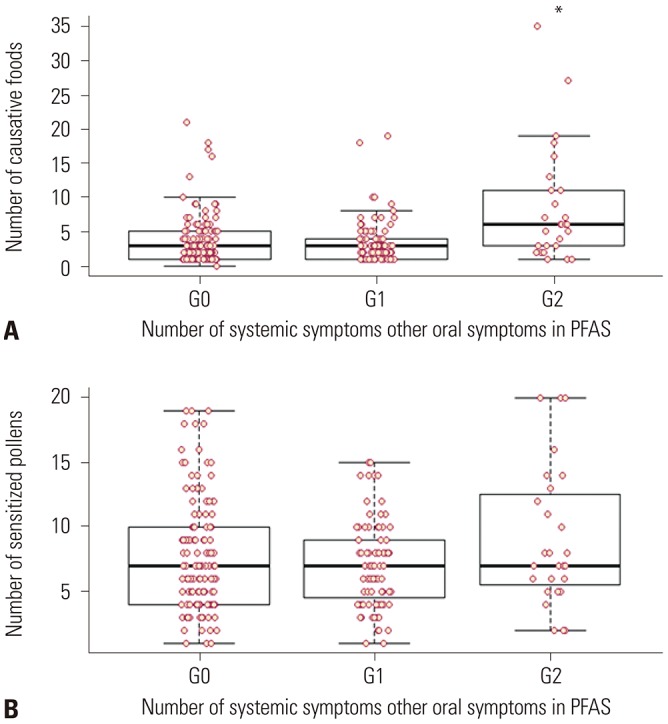
The most common cause of anaphylaxis in PFAS was peanut (33.3%), apple (22.2%), walnut (22.2%), pine nut (18.5%), peach (14.8%), and ginseng (14.8%). Anaphylaxis was significantly associated with the strength of sensitization to alder, hazel, willow, poplar, timothy, and ragweed (p<0.05, respectively). Multivariable analysis revealed that the presence of atopic dermatitis [odds ratio (OR), 3.58; 95% confidence interval (CI), 1.25-10.23; p=0.017]; sensitization to hazel (OR, 5.27; 95% CI, 1.79-15.53; p=0.003), timothy (OR, 11.8; 95% CI, 2.70-51.64; p=0.001), or ragweed (OR, 3.18; 95% CI, 1.03-9.87; p=0.045); and the number of culprit foods (OR, 1.25; 95% CI, 1.15-1.37; p<0.001) were related to the development of anaphylaxis in PFAS.
CONCLUSION
The most common culprit foods causing anaphylaxis in PFAS were peanut and apple. The presence of atopic dermatitis; sensitization to hazel, timothy, or ragweed; and a greater number of culprit foods were risk factors for anaphylaxis in PFAS.
MeSH Terms
Figure
Cited by 1 articles
-
Revised Pollen Calendar in Korea
Jung-Won Park
Allergy Asthma Immunol Res. 2020;12(2):171-172. doi: 10.4168/aair.2020.12.2.171.
Reference
-
1. Björkstén B, Clayton T, Ellwood P, Stewart A, Strachan D. ISAAC Phase III Study Group. Worldwide time trends for symptoms of rhinitis and conjunctivitis: Phase III of the International Study of Asthma and Allergies in Childhood. Pediatr Allergy Immunol. 2008; 19:110–124. PMID: 17651373.
Article2. Yura A, Kouda K, Iki M, Shimizu T. Trends of allergic symptoms in school children: large-scale long-term consecutive cross-sectional studies in Osaka Prefecture, Japan. Pediatr Allergy Immunol. 2011; 22:631–637. PMID: 21466587.
Article3. Kim SH, Park HS, Jang JY. Impact of meteorological variation on hospital visits of patients with tree pollen allergy. BMC Public Health. 2011; 11:890. PMID: 22115497.
Article4. Ma S, Sicherer SH, Nowak-Wegrzyn A. A survey on the management of pollen-food allergy syndrome in allergy practices. J Allergy Clin Immunol. 2003; 112:784–788. PMID: 14564362.
Article5. Lee SH, Ban GY, Jeong K, Shin YS, Park HS, Lee S, et al. A retrospective study of Korean adults with food allergy: differences in phenotypes and causes. Allergy Asthma Immunol Res. 2017; 9:534–539. PMID: 28913993.
Article6. Ortolani C, Pastorello EA, Farioli L, Ispano M, Pravettoni V, Berti C, et al. IgE-mediated allergy from vegetable allergens. Ann Allergy. 1993; 71:470–476. PMID: 8250353.7. Brown CE, Katelaris CH. The prevalence of the oral allergy syndrome and pollen-food syndrome in an atopic paediatric population in south-west Sydney. J Paediatr Child Health. 2014; 50:795–800. PMID: 24953857.
Article8. Flores E, Cervera L, Sanz ML, Diaz-Perales A, Fernández J. Plant food allergy in patients with pollinosis from the Mediterranean area. Int Arch Allergy Immunol. 2012; 159:346–354. PMID: 22832505.
Article9. Sicherer SH. Clinical implications of cross-reactive food allergens. J Allergy Clin Immunol. 2001; 108:881–890. PMID: 11742262.
Article10. Mari A, Ballmer-Weber BK, Vieths S. The oral allergy syndrome: improved diagnostic and treatment methods. Curr Opin Allergy Clin Immunol. 2005; 5:267–273. PMID: 15864087.
Article11. Osterballe M, Hansen TK, Mortz CG, Høst A, Bindslev-Jensen C. The prevalence of food hypersensitivity in an unselected population of children and adults. Pediatr Allergy Immunol. 2005; 16:567–573. PMID: 16238581.
Article12. Kong N, Kim S, Lee SC, Park KH, Lee JH, Park JW. Subcutaneous immunotherapy in patients with Fagales pollen-induced oral allergy syndrome. Yonsei Med J. 2019; 60:389–394. PMID: 30900426.
Article13. Kim JH, Kim SH, Park HW, Cho SH, Chang YS. Oral allergy syndrome in birch pollen-sensitized patients from a Korean University Hospital. J Korean Med Sci. 2018; 33:e218. PMID: 30093847.
Article14. Kim MA, Kim DK, Yang HJ, Yoo Y, Ahn Y, Park HS, et al. Pollenfood allergy syndrome in Korean pollinosis patients: a nationwide survey. Allergy Asthma Immunol Res. 2018; 10:648–661. PMID: 30306747.
Article15. Hofmann A, Burks AW. Pollen food syndrome: update on the allergens. Curr Allergy Asthma Rep. 2008; 8:413–417. PMID: 18682109.
Article16. Bousquet J, Heinzerling L, Bachert C, Papadopoulos NG, Bousquet PJ, Burney PG, et al. Practical guide to skin prick tests in allergy to aeroallergens. Allergy. 2012; 67:18–24. PMID: 22050279.17. Sampson HA, Muñoz-Furlong A, Campbell RL, Adkinson NF Jr, Bock SA, Branum A, et al. Second symposium on the definition and management of anaphylaxis: summary report--Second National Institute of Allergy and Infectious Disease/Food Allergy and Anaphylaxis Network symposium. J Allergy Clin Immunol. 2006; 117:391–397. PMID: 16461139.
Article18. Park HJ, Lim HS, Park KH, Lee JH, Park JW, Hong CS. Changes in allergen sensitization over the last 30 years in Korea respiratory allergic patients: a single-center. Allergy Asthma Immunol Res. 2014; 6:434–443. PMID: 25229001.
Article19. Maeda N, Inomata N, Morita A, Kirino M, Ikezawa Z. Correlation of oral allergy syndrome due to plant-derived foods with pollen sensitization in Japan. Ann Allergy Asthma Immunol. 2010; 104:205–210. PMID: 20377109.
Article20. Katelaris CH. Food allergy and oral allergy or pollen-food syndrome. Curr Opin Allergy Clin Immunol. 2010; 10:246–251. PMID: 20431372.
Article21. Fernández-Rivas M, Bolhaar S, González-Mancebo E, Asero R, van Leeuwen A, Bohle B, et al. Apple allergy across Europe: how allergen sensitization profiles determine the clinical expression of allergies to plant foods. J Allergy Clin Immunol. 2006; 118:481–488. PMID: 16890775.
Article22. Kim J, Hahm MI, Lee SY, Kim WK, Chae Y, Park YM, et al. Sensitization to aeroallergens in Korean children: a population-based study in 2010. J Korean Med Sci. 2011; 26:1165–1172. PMID: 21935271.
Article23. Wangorsch A, Jamin A, Lidholm J, Gräni N, Lang C, Ballmer-Weber B, et al. Identification and implication of an allergenic PR-10 protein from walnut in birch pollen associated walnut allergy. Mol Nutr Food Res. 2017; 61:DOI: 10.1002/mnfr.201600902.
Article24. Lim KH, Kang MK, Kim BK, Kim MH, Park HK, Lim JA, et al. A case of anaphylaxis after ingestion of freshginseng. Korean J Asthma Allergy Clin Immunol. 2010; 30:131–134.25. Kim M, Choi E, Yoon T. Korean ginseng makes oral allergy syndrome in birch-sensitized respiratory allergy patients. J Allergy Clin Immunol. 2008; 121:S187.
Article26. Stiefel G, Anagnostou K, Boyle RJ, Brathwaite N, Ewan P, Fox AT, et al. BSACI guideline for the diagnosis and management of peanut and tree nut allergy. Clin Exp Allergy. 2017; 47:719–739. PMID: 28836701.
Article27. Breiteneder H, Ebner C. Molecular and biochemical classification of plant-derived food allergens. J Allergy Clin Immunol. 2000; 106(1 Pt 1):27–36. PMID: 10887301.
Article28. Muluk NB, Cingi C. Oral allergy syndrome. Am J Rhinol Allergy. 2018; 32:27–30. PMID: 29336286.
Article29. Eriksson NE, Formgren H, Svenonius E. Food hypersensitivity in patients with pollen allergy. Allergy. 1982; 37:437–443. PMID: 7137538.
Article30. Lee S, Bashore C, Lohse CM, Bellolio MF, Chamberlain A, Yuki K, et al. Rate of recurrent anaphylaxis and associated risk factors among Olmsted County, Minnesota, residents: a population-based study. Ann Allergy Asthma Immunol. 2016; 117:655–660. PMID: 27979023.