J Korean Neurosurg Soc.
2017 Sep;60(5):534-539. 10.3340/jkns.2016.1011.001.
Surgical Roles for Spinal Involvement of Hematological Malignancies
- Affiliations
-
- 1Department of Orthopaedic Surgery, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. boscoa@catholic.ac.kr
- KMID: 2457960
- DOI: http://doi.org/10.3340/jkns.2016.1011.001
Abstract
OBJECTIVE
Patients with hematological malignancies frequently encounter spine-related symptoms, which are caused by disease itself or process of treatment. However, there is still lack of knowledge on their epidemiology and clinical courses. The purpose of this article is to review clinical presentations and surgical results for spinal involvement of hematologic malignancies.
METHODS
From January 2011 to September 2014, 195 patients (98 males and 97 females) suffering from hematological malignancies combined with spinal problems were retrospectively analyzed for clinical and radiological characteristics and their clinical results.
RESULTS
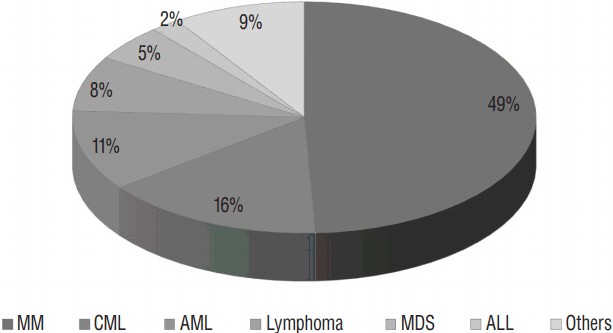
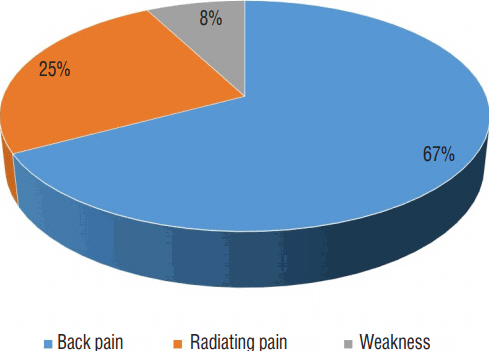
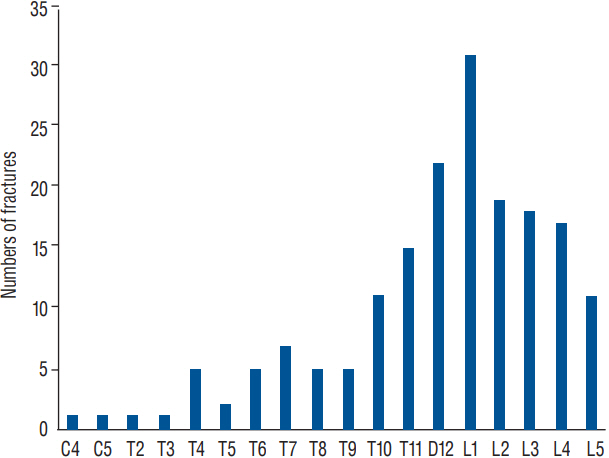
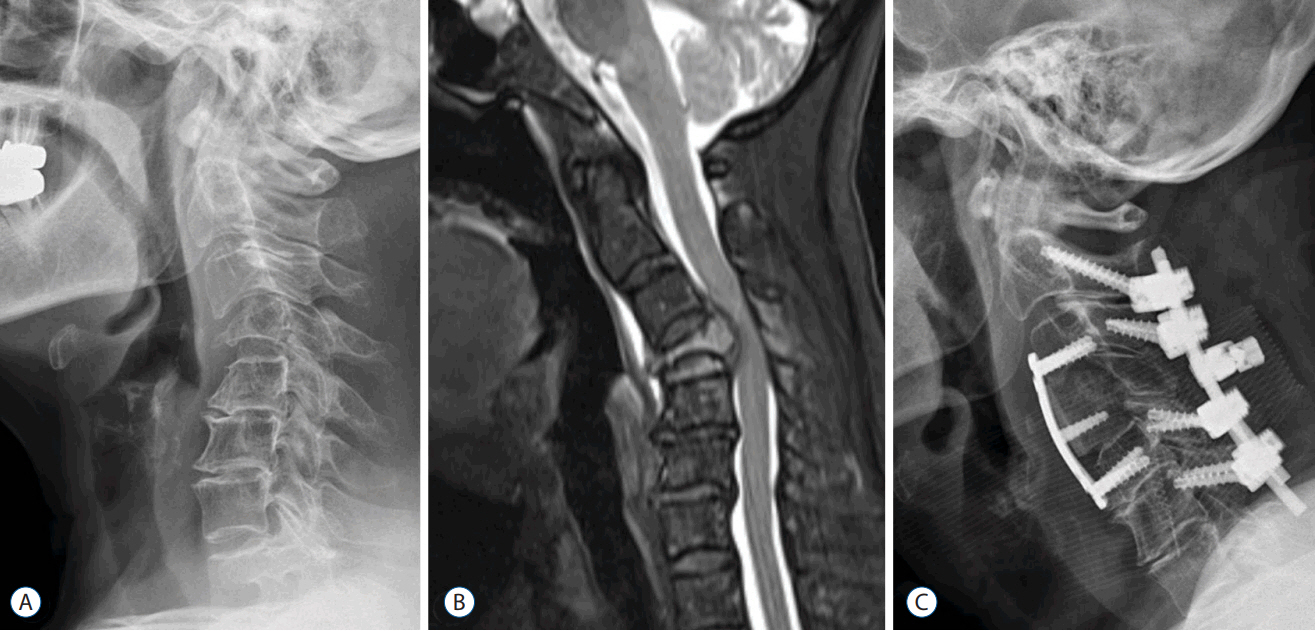
The most common diagnosis of hematological malignancy was multiple myeloma (96 patients, 49.7%), followed by chronic myeloid leukemia (30, 15.2%), acute myeloid leukemia (22, 11.2%), and lymphoma (15, 7.56%). The major presenting symptoms were mechanical axial pain (132, 67.7%) resulting from pathologic fractures, and followed by radiating pain (49, 25.1%). Progressive neurologic deficits were noted in 15 patients (7.7%), which revealed as cord compression by epidural mass or compressive myelopathy combined with pathologic fractures. Reconstructive surgery for neurologic compromise was done in 16 patients. Even though surgical intervention was useful for early paralysis (Frankel grade D or E), neurologic recovery was not satisfactory for the progressed paralysis (Frankel grade A or B).
CONCLUSION
Hematological malignancies may cause various spinal problems related to disease progression or consequences of treatments. Conservative and palliative treatments are mainstay for these lesions. However, timely surgical interventions should be considered for the cases of pathologic fractures with progressive neurologic compromise.
Keyword
MeSH Terms
-
Diagnosis
Disease Progression
Epidemiology
Fractures, Spontaneous
Hematologic Neoplasms*
Humans
Leukemia, Myelogenous, Chronic, BCR-ABL Positive
Leukemia, Myeloid, Acute
Lymphoma
Male
Multiple Myeloma
Neurologic Manifestations
Palliative Care
Paralysis
Retrospective Studies
Spinal Cord Compression
Spinal Cord Injuries
Spine
Figure
Cited by 1 articles
-
Unstable Pathologic Vertebral Fractures in Multiple Myeloma : Propensity Score Matched Cohort Study between Reconstructive Surgery with Adjuvant Radiotherapy and Radiotherapy Alone
Hyung-Youl Park, Young-Hoon Kim, Joo-Hyun Ahn, Kee-Yong Ha, Sang-Il Kim, Jae-Woong Jung
J Korean Neurosurg Soc. 2022;65(2):287-296. doi: 10.3340/jkns.2021.0199.
Reference
-
References
1. Bickels J, Dadia S, Lidar Z. Surgical management of metastatic bone disease. J Bone Joint Surg Am. 91:1503–1516. 2009.
Article2. Bladé J, Rosiñol L. Complications of multiple myeloma. Hematol Oncol Clin North Am. 21:1231–1246. xi2007.
Article3. Cavaletti G, Jakubowiak AJ. Peripheral neuropathy during bortezomib treatment of multiple myeloma: a review of recent studies. Leuk Lymphoma. 51:1178–1187. 2010.
Article4. Choi D, Crockard A, Bunger C, Harms J, Kawahara N, Mazel C, et al. Review of metastatic spine tumour classification and indications for surgery: the consensus statement of the Global Spine Tumour Study Group. Eur Spine J. 19:215–222. 2010.
Article5. Dürr HR, Müller PE, Hiller E, Maier M, Baur A, Jansson V, et al. Malignant lymphoma of bone. Arch Orthop Trauma Surg. 122:10–16. 2002.
Article6. Dürr HR, Wegener B, Krödel A, Müller PE, Jansson V, Refior HJ. Multiple myeloma: surgery of the spine: retrospective analysis of 27 patients. Spine (Phila Pa 1976). 27:320–324. discussion 325–326. 2002.7. Flouzat-Lachaniette CH, Allain J, Roudot-Thoraval F, Poignard A. Treatment of spinal epidural compression due to hematological malignancies: a single institution’s retrospective experience. Eur Spine J. 22:548–555. 2013.
Article8. Fourney DR, Frangou EM, Ryken TC, Dipaola CP, Shaffrey CI, Berven SH, et al. Spinal instability neoplastic score: an analysis of reliability and validity from the spine oncology study group. J Clin Oncol. 29:3072–3077. 2011.
Article9. Ha KY, Min CK, Seo JY, Kim YH, Ahn JH, Hyun NM, et al. Bone cement augmentation procedures for spinal pathologic fractures by multiple myeloma. J Korean Med Sci. 30:88–94. 2015.
Article10. Hage WD, Aboulafia AJ, Aboulafia DM. Incidence, location, and diagnostic evaluation of metastatic bone disease. Orthop Clin North Am. 31:515–528. vii2000.
Article11. Hameed A, Brady JJ, Dowling P, Clynes M, O’Gorman P. Bone disease in multiple myeloma: pathophysiology and management. Cancer Growth Metastasis. 7:33–42. 2014.
Article12. Kaloostian PE, Yurter A, Zadnik PL, Sciubba DM, Gokaslan ZL. Current paradigms for metastatic spinal disease: an evidence-based review. Ann Surg Oncol. 21:248–262. 2014.
Article13. Lal A, Tallman MS, Soble MB, Golubovich I, Peterson L. Hairy cell leukemia presenting as localized skeletal involvement. Leuk Lyhmphoma. 43:2207–2211. 2002.
Article14. Muta T, Osaki K, Yamano Y. Translocation t(9;22) (p23;q11) in atypical chronic myeloid leukemia (aCML) presenting osteolytic lesions. Int J Hematol. 76:344–348. 2002.
Article15. Niscola P, Arcuri E, Giovannini M, Scaramucci L, Romani C, Palombi F, et al. Pain syndromes in haematological malignancies: an overview. Hematol J. 5:293–303. 2004.
Article16. Popescu M, Popov V, Popescu G, Dobrea C, Sandu A, Grigorean VT, et al. Spinal involvement with spinal cord compression syndrome in hematological diseases. Rom J Morphol Embryol. 53:1069–1072. 2012.17. Recht L, Mrugala M. Neurologic complications of hematologic neoplasms. Neurol Clin. 21:87–105. 2003.
Article18. Rodriguez-Abreu D, Bordoni A, Zucca E. Epidemiology of hematological malignancies. Ann Oncol. 18(Suppl 1):i3–i8. 2007.
Article19. Tomita K, Kawahara N, Kobayashi T, Yoshida A, Murakami H, Akamaru T. Surgical strategy for spinal metastases. Spine (Phila Pa 1976). 26:298–306. 2001.
Article20. Utzschneider S, Schmidt H, Weber P, Schmidt GP, Jansson V, Durr HR. Surgical therapy of skeletal complications in multiple myeloma. Int Orthop. 35:1209–1213. 2011.
Article21. Zadnik PL, Goodwin CR, Karami KJ, Mehta AI, Amin AG, Groves ML, et al. Outcomes following surgical intervention for impending and gross instability caused by multiple myeloma in the spinal column. J Neurosurg Spine. 22:301–309. 2015.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgery for Pulmonary Fungal Infections Complicating Hematological Malignancies
- Multiple Primary Cancers With Hematologic Malignancies and Germline Predisposition: A Case Series
- Atypical Form of Multiple Spinal Tuberculosis
- A Case of Sweet's Panniculitis Associated with Spinal Metastasis from Prostate Cancer
- Pulmonary Resection for Invasive Pulmonary Aspergillosis in Hematological Malignancy Patients