J Periodontal Implant Sci.
2019 Jun;49(3):193-204. 10.5051/jpis.2019.49.3.193.
Decontamination methods to restore the biocompatibility of contaminated titanium surfaces
- Affiliations
-
- 1Department of Dentistry, Graduate School, The Catholic University of Korea, Seoul, Korea.
- 2Department of Periodontics, Seoul St Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. ko_y@catholic.ac.kr
- 3Department of Oral Microbiology and Immunology, Seoul National University School of Dentistry, Seoul, Korea.
- 4Dental Research Institute, Seoul National University School of Dentistry, Seoul, Korea.
- KMID: 2454089
- DOI: http://doi.org/10.5051/jpis.2019.49.3.193
Abstract
- PURPOSE
The reaction of cells to a titanium implant depends on the surface characteristics of the implant which are affected by decontamination. The aim of this study was to evaluate the cytocompatibility of titanium disks treated with various decontamination methods, using salivary bacterial contamination with dental pellicle formation as an in vitro model.
METHODS
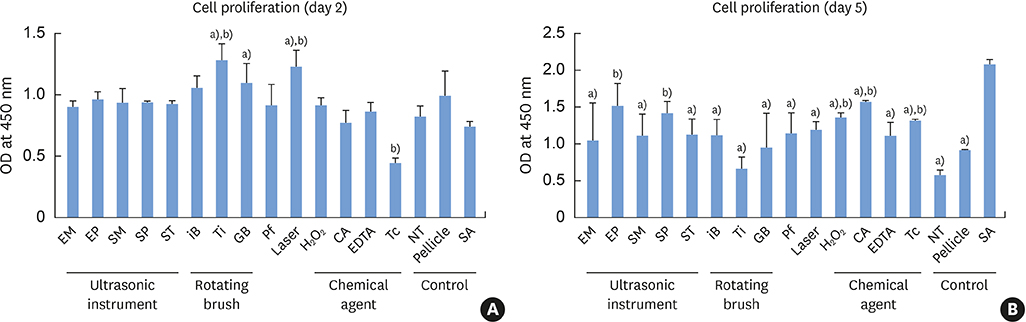
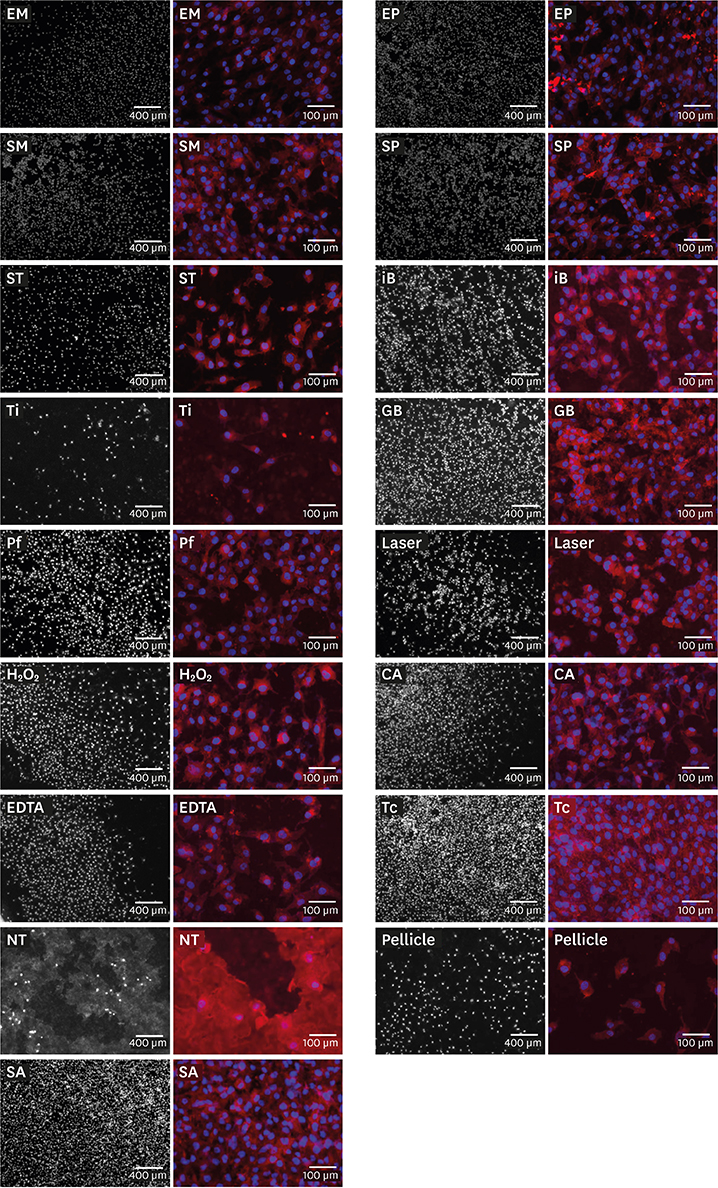
Sand-blasted and acid-etched (SA) titanium disks were used. Three control groups (pristine SA disks [SA group]; salivary pellicle-coated SA disks [pellicle group]; and biofilm-coated, untreated SA disks [NT group]) were not subjected to any decontamination treatments. Decontamination of the biofilm-coated disks was performed by 14 methods, including ultrasonic instruments, rotating instruments, an air-powder abrasive system, a laser, and chemical agents. MG63 cells were cultured in the presence of the treated disks. Cell proliferation assays were performed on days 2 and 5 of cell culture, and cell morphology was analyzed by immunofluorescence and scanning electron microscopy (SEM). A vascular endothelial growth factor (VEGF) assay was performed on day 5 of culture.
RESULTS
The cell proliferation assay revealed that all decontaminated disks, except for the 2 groups treated using a plastic tip, showed significantly less cell proliferation than the SA group. The immunofluorescence and SEM analyses revealed that most groups showed comparable cell density, with the exception of the NT group, in which the cell density was lower and bacterial residue was observed. Furthermore, the cells grown with tetracycline-treated titanium disks showed significantly lower VEGF production than those in the SA group.
CONCLUSIONS
None of the decontamination methods resulted in cytocompatibility similar to that of pristine SA titanium. However, many methods caused improvement in the biocompatibility of the titanium disks in comparison with the biofilm-coated, untreated titanium disks. This suggests that decontamination is indispensable for the treatment of peri-implantitis, even if the original biocompatibility cannot be restored.
MeSH Terms
-
Biocompatible Materials
Cell Count
Cell Culture Techniques
Cell Proliferation
Decontamination*
Dental Implants
Dental Pellicle
Fluorescent Antibody Technique
In Vitro Techniques
Methods*
Microscopy, Electron, Scanning
Peri-Implantitis
Plastics
Titanium*
Ultrasonics
Vascular Endothelial Growth Factor A
Biocompatible Materials
Dental Implants
Plastics
Titanium
Vascular Endothelial Growth Factor A
Figure
Reference
-
1. Zitzmann NU, Berglundh T. Definition and prevalence of peri-implant diseases. J Clin Periodontol. 2008; 35:286–291.
Article2. Louropoulou A, Slot DE, Van der Weijden F. Influence of mechanical instruments on the biocompatibility of titanium dental implants surfaces: a systematic review. Clin Oral Implants Res. 2015; 26:841–850.
Article3. Lindhe J, Meyle J. Group D of European Workshop on Periodontology. Peri-implant diseases: consensus report of the Sixth European Workshop on Periodontology. J Clin Periodontol. 2008; 35:282–285.
Article4. Unursaikhan O, Lee JS, Cha JK, Park JC, Jung UW, Kim CS, et al. Comparative evaluation of roughness of titanium surfaces treated by different hygiene instruments. J Periodontal Implant Sci. 2012; 42:88–94.
Article5. Schwarz F, Rothamel D, Sculean A, Georg T, Scherbaum W, Becker J. Effects of an Er:YAG laser and the Vector ultrasonic system on the biocompatibility of titanium implants in cultures of human osteoblast-like cells. Clin Oral Implants Res. 2003; 14:784–792.
Article6. Augthun M, Tinschert J, Huber A. In vitro studies on the effect of cleaning methods on different implant surfaces. J Periodontol. 1998; 69:857–864.
Article7. Ungvári K, Pelsöczi IK, Kormos B, Oszkó A, Rakonczay Z, Kemény L, et al. Effects on titanium implant surfaces of chemical agents used for the treatment of peri-implantitis. J Biomed Mater Res B Appl Biomater. 2010; 94:222–229.
Article8. Parham PL Jr, Cobb CM, French AA, Love JW, Drisko CL, Killoy WJ. Effects of an air-powder abrasive system on plasma-sprayed titanium implant surfaces: an in vitro evaluation. J Oral Implantol. 1989; 15:78–86.9. Kreisler M, Kohnen W, Christoffers AB, Götz H, Jansen B, Duschner H, et al. In vitro evaluation of the biocompatibility of contaminated implant surfaces treated with an Er : YAG laser and an air powder system. Clin Oral Implants Res. 2005; 16:36–43.
Article10. Yang SM, Park JB, Ko Y. Use of confocal microscopy for quantification of plastic remnants on rough titanium after instrumentation and evaluation of efficacy of removal. Int J Oral Maxillofac Implants. 2015; 30:519–525.
Article11. Park JB, Jeon Y, Ko Y. Effects of titanium brush on machined and sand-blasted/acid-etched titanium disc using confocal microscopy and contact profilometry. Clin Oral Implants Res. 2015; 26:130–136.
Article12. Wennerberg A, Albrektsson T. Effects of titanium surface topography on bone integration: a systematic review. Clin Oral Implants Res. 2009; 20:Suppl 4. 172–184.
Article13. Mann M, Parmar D, Walmsley AD, Lea SC. Effect of plastic-covered ultrasonic scalers on titanium implant surfaces. Clin Oral Implants Res. 2012; 23:76–82.
Article14. Renvert S, Lindahl C, Roos Jansåker AM, Persson GR. Treatment of peri-implantitis using an Er:YAG laser or an air-abrasive device: a randomized clinical trial. J Clin Periodontol. 2011; 38:65–73.
Article15. Louropoulou A, Slot DE, Weijden F. The effects of mechanical instruments on contaminated titanium dental implant surfaces: a systematic review. Clin Oral Implants Res. 2014; 25:1149–1160.
Article16. John G, Becker J, Schwarz F. Rotating titanium brush for plaque removal from rough titanium surfaces--an in vitro study. Clin Oral Implants Res. 2014; 25:838–842.
Article17. Schwarz F, Sculean A, Romanos G, Herten M, Horn N, Scherbaum W, et al. Influence of different treatment approaches on the removal of early plaque biofilms and the viability of SAOS2 osteoblasts grown on titanium implants. Clin Oral Investig. 2005; 9:111–117.
Article18. Schwarz F, Ferrari D, Popovski K, Hartig B, Becker J. Influence of different air-abrasive powders on cell viability at biologically contaminated titanium dental implants surfaces. J Biomed Mater Res B Appl Biomater. 2009; 88B:83–91.
Article19. Park JB, Lee SH, Kim N, Park S, Jin SH, Choi BK, et al. Instrumentation with ultrasonic scalers facilitates cleaning of the sandblasted and acid-etched titanium implants. J Oral Implantol. 2015; 41:419–428.
Article20. Schmidt KE, Auschill TM, Heumann C, Frankenberger R, Eick S, Sculean A, et al. Influence of different instrumentation modalities on the surface characteristics and biofilm formation on dental implant neck, in vitro . Clin Oral Implants Res. 2017; 28:483–490.
Article21. Lincks J, Boyan BD, Blanchard CR, Lohmann CH, Liu Y, Cochran DL, et al. Response of MG63 osteoblast-like cells to titanium and titanium alloy is dependent on surface roughness and composition. Biomaterials. 1998; 19:2219–2232.
Article22. Bordji K, Jouzeau JY, Mainard D, Payan E, Netter P, Rie KT, et al. Cytocompatibility of Ti-6Al-4V and Ti-5Al-2.5Fe alloys according to three surface treatments, using human fibroblasts and osteoblasts. Biomaterials. 1996; 17:929–940.
Article23. Park JW, Kim YJ, Jang JH. Enhanced osteoblast response to hydrophilic strontium and/or phosphate ions-incorporated titanium oxide surfaces. Clin Oral Implants Res. 2010; 21:398–408.
Article24. Donley TG, Gillette WB. Titanium endosseous implant-soft tissue interface: a literature review. J Periodontol. 1991; 62:153–160.
Article25. Lindhe J, Lang NP, Berglundh T, Giannobile WV, Sanz M. Clinical periodontology and implant dentistry. Ames: John Wiley & Sons;2015.26. Tilakaratne A, Soory M. Anti-inflammatory actions of adjunctive tetracyclines and other agents in periodontitis and associated comorbidities. Open Dent J. 2014; 8:109–124.
Article27. Perret LJ, Tait CP. Non-antibiotic properties of tetracyclines and their clinical application in dermatology. Australas J Dermatol. 2014; 55:111–118.
Article28. Lee S, Jilani SM, Nikolova GV, Carpizo D, Iruela-Arispe ML. Processing of VEGF-A by matrix metalloproteinases regulates bioavailability and vascular patterning in tumors. J Cell Biol. 2005; 169:681–691.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Endotoxin Assay of Contaminated Titanium Implants following Various Techniques of Detoxification
- The effect of saliva decontamination procedures on dentin bond strength after universal adhesive curing
- The Effectiveness Of Decontamination Methods In Dental Instruments
- The Effects of a Er:YAG Laser on Machined, Sand-Blasted and Acid-Etched, and Resorbable Blast Media Titanium Surfaces Using Confocal Microscopy and Scanning Electron Microscopy
- Comparative evaluation of roughness of titanium surfaces treated by different hygiene instruments