Nutr Res Pract.
2019 Jun;13(3):214-221. 10.4162/nrp.2019.13.3.214.
A prospective study on changes in body composition and fat percentage during the first year of cancer treatment in children
- Affiliations
-
- 1Department of Pediatrics, Seoul National University Bundang Hospital, Seoul National University College of Medicine, 82 Gumi-ro 173 Beon-gil, Bundang-gu, Seongnam, Gyeonggi 13620, Korea. choihs1786@snubh.org
- KMID: 2453285
- DOI: http://doi.org/10.4162/nrp.2019.13.3.214
Abstract
- BACKGROUND
S/OBJECTIVES: Cancer treatment may lead to significant body composition changes and affect growth and disease outcomes in pediatric cancer patients. This prospective study aimed to evaluate short- and long-term body compositions changes focused on body fat during the first year of cancer treatment in children.
SUBJECTS/METHODS
A prospective study was conducted in 30 pediatric cancer patients (19 hematologic malignancies and 11 solid tumors) and 30 age- and sex-matched healthy controls. Anthropometric measurements and body composition analysis using whole body dual energy X-ray absorptiometry were performed at baseline and 1, 6, and 12 month(s) of cancer treatment. Kruskal-Wallis tests, Wilcoxon paired t tests, and generalized estimation equation (GEE) were applied for statistical analysis.
RESULTS
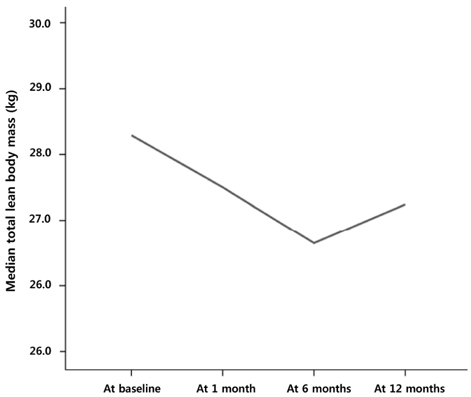
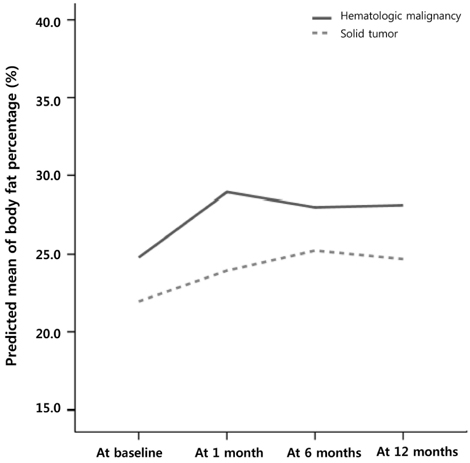
At baseline, no differences in weight, height, body mass index, abdominal circumferences, body fat, and fat-free mass were observed between 30 controls and 30 pediatric cancer patients. Total fat mass (P < 0.001) and body fat percentage (P = 0.002) increased significantly during the first month, but no changes were observed from 1 to 12 months; however, no changes in the total mass were observed during the first year of cancer treatment. Meanwhile, the total fat-free mass decreased during the first month (P = 0.008) and recovered between 6 and 12 months of follow-up (P < 0.001). According to GEE analysis, there was a significant upward trend in body fat percentage during the first year, especially the first month, of cancer treatment in children with hematologic malignancies, but not in those with solid tumors.
CONCLUSIONS
Our results indicate that cancer treatment is related to significant body composition changes and rapid body fat gain, particularly during the first month after initiating cancer treatment, in children with hematologic malignancies. Therefore, individualized dietary strategies to prevent excessive fat gain are needed in pediatric cancer patients for better outcomes.
MeSH Terms
Figure
Reference
-
1. Collins L, Nayiager T, Doring N, Kennedy C, Webber C, Halton J, Walker S, Sala A, Barr RD. Nutritional status at diagnosis in children with cancer I. An assessment by dietary recall--compared with body mass index and body composition measured by dual energy X-ray absorptiometry. J Pediatr Hematol Oncol. 2010; 32:e299–e303.
Article2. Brinksma A, Roodbol PF, Sulkers E, de Bont ES, Burgerhof JG, Tamminga RY, Jager-Wittenaar H, Tissing WJ. Finding the right balance: an evaluation of the adequacy of energy and protein intake in childhood cancer patients. Clin Nutr. 2015; 34:284–290.
Article3. Iniesta RR, Paciarotti I, Brougham MF, McKenzie JM, Wilson DC. Effects of pediatric cancer and its treatment on nutritional status: a systematic review. Nutr Rev. 2015; 73:276–295.
Article4. Sala A, Rossi E, Antillon F, Molina AL, de Maselli T, Bonilla M, Hernandez A, Ortiz R, Pacheco C, Nieves R, Navarrete M, Barrantes M, Pencharz P, Valsecchi MG, Barr R. Nutritional status at diagnosis is related to clinical outcomes in children and adolescents with cancer: a perspective from Central America. Eur J Cancer. 2012; 48:243–252.
Article5. Murphy AJ, White M, Davies PS. Body composition of children with cancer. Am J Clin Nutr. 2010; 92:55–60.
Article6. Brinksma A, Huizinga G, Sulkers E, Kamps W, Roodbol P, Tissing W. Malnutrition in childhood cancer patients: a review on its prevalence and possible causes. Crit Rev Oncol Hematol. 2012; 83:249–275.
Article7. Tan SY, Poh BK, Nadrah MH, Jannah NA, Rahman J, Ismail MN. Nutritional status and dietary intake of children with acute leukaemia during induction or consolidation chemotherapy. J Hum Nutr Diet. 2013; 26:Suppl 1. 23–33.
Article8. Butturini AM, Dorey FJ, Lange BJ, Henry DW, Gaynon PS, Fu C, Franklin J, Siegel SE, Seibel NL, Rogers PC, Sather H, Trigg M, Bleyer WA, Carroll WL. Obesity and outcome in pediatric acute lymphoblastic leukemia. J Clin Oncol. 2007; 25:2063–2069.
Article9. Di Sebastiano KM, Mourtzakis M. A critical evaluation of body composition modalities used to assess adipose and skeletal muscle tissue in cancer. Appl Physiol Nutr Metab. 2012; 37:811–821.
Article10. Murphy AJ, White M, Elliott SA, Lockwood L, Hallahan A, Davies PS. Body composition of children with cancer during treatment and in survivorship. Am J Clin Nutr. 2015; 102:891–896.
Article11. Halpern-Silveira D, Susin LR, Borges LR, Paiva SI, Assunção MC, Gonzalez MC. Body weight and fat-free mass changes in a cohort of patients receiving chemotherapy. Support Care Cancer. 2010; 18:617–625.
Article12. Sheean PM, Hoskins K, Stolley M. Body composition changes in females treated for breast cancer: a review of the evidence. Breast Cancer Res Treat. 2012; 135:663–680.
Article13. Tenardi RD, Frühwald MC, Jürgens H, Hertroijs D, Bauer J. Nutritional status of children and young adults with Ewing sarcoma or osteosarcoma at diagnosis and during multimodality therapy. Pediatr Blood Cancer. 2012; 59:621–626.
Article14. Fuemmeler BF, Pendzich MK, Clark K, Lovelady C, Rosoff P, Blatt J, Demark-Wahnefried W. Diet, physical activity, and body composition changes during the first year of treatment for childhood acute leukemia and lymphoma. J Pediatr Hematol Oncol. 2013; 35:437–443.
Article15. Brinksma A, Roodbol PF, Sulkers E, Kamps WA, de Bont ES, Boot AM, Burgerhof JG, Tamminga RY, Tissing WJ. Changes in nutritional status in childhood cancer patients: a prospective cohort study. Clin Nutr. 2015; 34:66–73.
Article16. Choi HS, Chang EJ, Lee EH, Yang HR. Changes in bone health during the first year of cancer treatment in children. J Clin Densitom. 2017; 20:25–31.
Article17. Harrington DM, Staiano AE, Broyles ST, Gupta AK, Katzmarzyk PT. Waist circumference measurement site does not affect relationships with visceral adiposity and cardiometabolic risk factors in children. Pediatr Obes. 2013; 8:199–206.
Article18. Kim JH, Yun S, Hwang SS, Shim JO, Chae HW, Lee YJ, Lee JH, Kim SC, Lim D, Yang SW, Oh K, Moon JS. Committee for the Development of Growth Standards for Korean Children and Adolescents. Committee for School Health and Public Health Statistics, the Korean Pediatric Society. Division of Health and Nutrition Survey, Korea Centers for Disease Control and Prevention. The 2017 Korean National Growth Charts for children and adolescents: development, improvement, and prospects. Korean J Pediatr. 2018; 61:135–149.
Article19. Ladas EJ, Sacks N, Meacham L, Henry D, Enriquez L, Lowry G, Hawkes R, Dadd G, Rogers P. A multidisciplinary review of nutrition considerations in the pediatric oncology population: a perspective from children's oncology group. Nutr Clin Pract. 2005; 20:377–393.
Article20. Jarfelt M, Lannering B, Bosaeus I, Johannsson G, Bjarnason R. Body composition in young adult survivors of childhood acute lymphoblastic leukaemia. Eur J Endocrinol. 2005; 153:81–89.
Article21. Barr R, Nayiager T, Gordon C, Marriott C, Athale U. Body composition and bone health in long-term survivors of acute lymphoblastic leukaemia in childhood and adolescence: the protocol for a cross-sectional cohort study. BMJ Open. 2015; 5:e006191.
Article22. Withycombe JS, Post-White JE, Meza JL, Hawks RG, Smith LM, Sacks N, Seibel NL. Weight patterns in children with higher risk ALL: a report from the Children's Oncology Group (COG) for CCG 1961. Pediatr Blood Cancer. 2009; 53:1249–1254.
Article23. Shin DW, Cho B, Kim SY, Jung JH, Park JH. Management of cancer survivors in clinical and public health perspectives: current status and future challenges in Korea. J Korean Med Sci. 2013; 28:651–657.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Body Composition Changes in Korean Children and Adolescents
- Body Composition of Children and Adolescents with Insulin-dependent Diabetes Mellitus
- Body composition by bioelectrical impedance analysis in children below 7 years old
- Body Composition by Bioelectrical Impedance Analysis in Obese Children
- The Association between Sleep Duration and Body Composition Variables in Korean Adults