Allergy Asthma Immunol Res.
2019 Sep;11(5):593-603. 10.4168/aair.2019.11.5.593.
Interactions Between Atopic Dermatitis and Staphylococcus aureus Infection: Clinical Implications
- Affiliations
-
- 1Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. kmaped@skku.edu
- 2Environmental Health Center for Atopic Diseases, Samsung Medical Center, Seoul, Korea.
- 3Department of Pediatrics, National Jewish Health, Denver, CO, USA. LeungD@njhealth.org
- KMID: 2452751
- DOI: http://doi.org/10.4168/aair.2019.11.5.593
Abstract
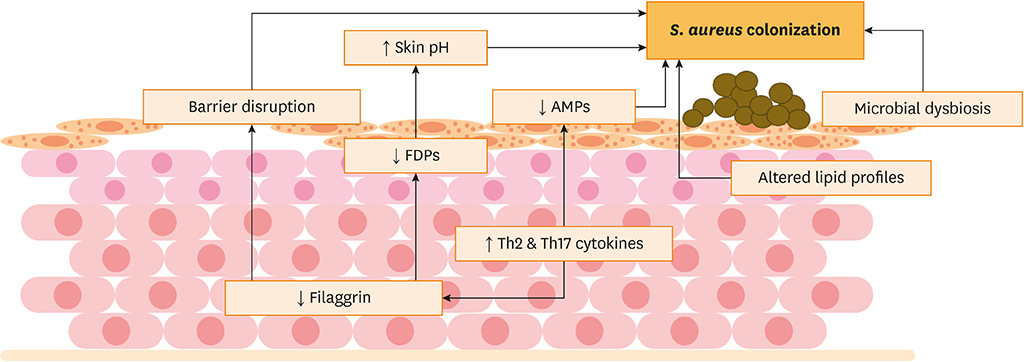
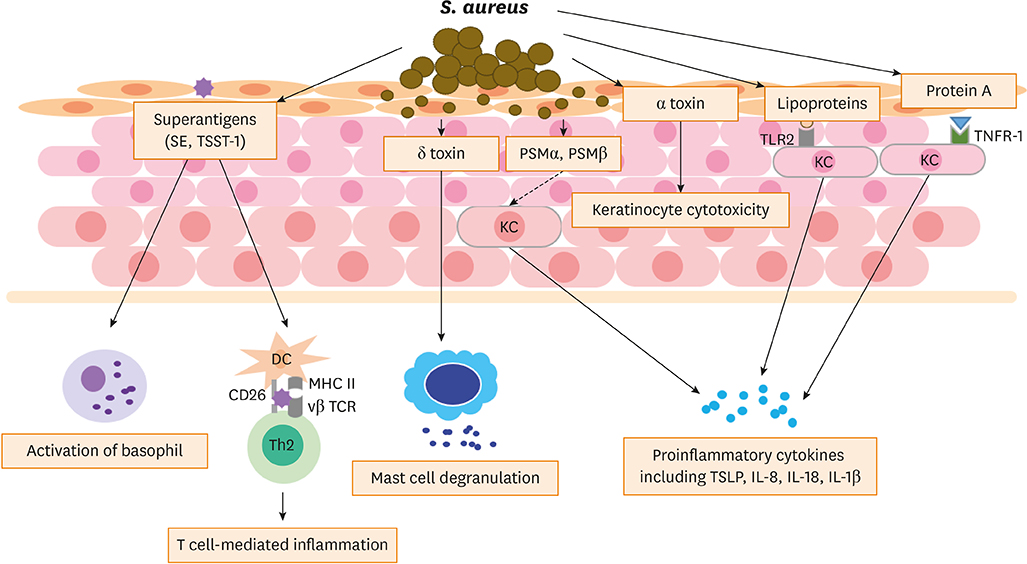
- Staphylococcus aureus commonly colonizes the skin of atopic dermatitis (AD) patients and contributes to the development and exacerbation of AD. Multiple factors are associated with colonization of AD skin by S. aureus, including the strength of S. aureus-corneocyte adhesion, deficiency of antimicrobial peptides, decreased levels of filaggrin and filaggrin degradation products, overexpressed Th2/Th17 cytokines, microbial dysbiosis and altered lipid profiles. S. aureus colonization on AD skin causes skin barrier dysfunction through virulence factors such as superantigens (toxins), enzymes and other proteins. Furthermore, colonization of AD skin by S. aureus exacerbates AD and may contribute to microbial dysbiosis, allergen sensitization, Th2/Th17 polarization, development of atopic march and food allergy in AD patients. Skin colonization of S. aureus, particularly methicillin-resistant S. aureus (MRSA), is one of the major challenges commonly encountered in the management of AD. Bleach bath, and topical or systemic antibiotics could be used to control S. aureus infection on AD skin. However, careful use of antibiotics is required to control the occurence of MRSA. Recently, various strategies, including microbiome transplant, monoclonal antibodies against virulent toxins, vaccines and recombinant phage endolysin, have been studied to control S. aureus infection on AD skin. Further advances in our understanding of S. aureus could provide us with ways to manage S. aureus colonization more effectively in AD patients.
Keyword
MeSH Terms
-
Anti-Bacterial Agents
Antibodies, Monoclonal
Bacteriophages
Baths
Colon
Cytokines
Dermatitis, Atopic*
Dysbiosis
Food Hypersensitivity
Humans
Methicillin Resistance
Methicillin-Resistant Staphylococcus aureus
Microbiota
Peptides
Skin
Staphylococcus aureus*
Staphylococcus*
Superantigens
Vaccines
Virulence Factors
Anti-Bacterial Agents
Antibodies, Monoclonal
Cytokines
Peptides
Superantigens
Vaccines
Virulence Factors
Figure
Reference
-
1. Leung DY. The microbiome and allergic diseases: a struggle between good and bad microbes. Ann Allergy Asthma Immunol. 2019; 122:231–232.2. Kim J, Kim BE, Leung DY. Pathophysiology of atopic dermatitis: clinical implications. Allergy Asthma Proc. 2019; 40:84–92.
Article3. Weidinger S, Novak N. Atopic dermatitis. Lancet. 2016; 387:1109–1122.
Article4. Kim BE, Leung DY. Significance of skin barrier dysfunction in atopic dermatitis. Allergy Asthma Immunol Res. 2018; 10:207–215.
Article5. Leung DY. Atopic dermatitis: more than a rash. Ann Allergy Asthma Immunol. 2018; 120:555–556.6. Leung DY. The effect of being African American on atopic dermatitis. Ann Allergy Asthma Immunol. 2019; 122:1.
Article7. Tham EH, Leung DY. Mechanisms by which atopic dermatitis predisposes to food allergy and the atopic march. Allergy Asthma Immunol Res. 2019; 11:4–15.
Article8. Leung DY, Guttman-Yassky E. Deciphering the complexities of atopic dermatitis: shifting paradigms in treatment approaches. J Allergy Clin Immunol. 2014; 134:769–779.
Article9. De Benedetto A, Agnihothri R, McGirt LY, Bankova LG, Beck LA. Atopic dermatitis: a disease caused by innate immune defects? J Invest Dermatol. 2009; 129:14–30.
Article10. Breuer K, HÄussler S, Kapp A, Werfel T. Staphylococcus aureus: colonizing features and influence of an antibacterial treatment in adults with atopic dermatitis. Br J Dermatol. 2002; 147:55–61.11. Kim BS, Kim JY, Lim HJ, Lee WJ, Lee SJ, Kim JM, et al. Colonizing features of Staphylococcus aureus in early childhood atopic dermatitis and in mothers: a cross-sectional comparative study done at four kindergartens in Daegu, South Korea. Ann Allergy Asthma Immunol. 2011; 106:323–329.12. Park HY, Kim CR, Huh IS, Jung MY, Seo EY, Park JH, et al. Staphylococcus aureus colonization in acute and chronic skin lesions of patients with atopic dermatitis. Ann Dermatol. 2013; 25:410–416.13. Shi B, Leung DY, Taylor PA, Li H. Methicillin-resistant Staphylococcus aureus colonization is associated with decreased skin commensal bacteria in atopic dermatitis. J Invest Dermatol. 2018; 138:1668–1671.14. Suh L, Coffin S, Leckerman KH, Gelfand JM, Honig PJ, Yan AC. Methicillin-resistant Staphylococcus aureus colonization in children with atopic dermatitis. Pediatr Dermatol. 2008; 25:528–534.15. Jagadeesan S, Kurien G, Divakaran MV, Sadanandan SM, Sobhanakumari K, Sarin A. Methicillin-resistant Staphylococcus aureus colonization and disease severity in atopic dermatitis: a cross-sectional study from South India. Indian J Dermatol Venereol Leprol. 2014; 80:229–234.16. Petry V, Lipnharski C, Bessa GR, Silveira VB, Weber MB, Bonamigo RR, et al. Prevalence of community-acquired methicillin-resistant Staphylococcus aureus and antibiotic resistance in patients with atopic dermatitis in Porto Alegre, Brazil. Int J Dermatol. 2014; 53:731–735.17. Jung MY, Chung JY, Lee HY, Park J, Lee DY, Yang JM. Antibiotic susceptibility of Staphylococcus aureus in atopic dermatitis: current prevalence of methicillin-resistant Staphylococcus aureus in Korea and treatment strategies. Ann Dermatol. 2015; 27:398–403.18. Park JM, Jo JH, Jin H, Ko HC, Kim MB, Kim JM, et al. Change in antimicrobial susceptibility of skin-colonizing Staphylococcus aureus in Korean patients with atopic dermatitis during ten-year period. Ann Dermatol. 2016; 28:470–478.19. Leung DY, Hanifin JM, Pariser DM, Barber KA, Langley RG, Schlievert PM, et al. Effects of pimecrolimus cream 1% in the treatment of patients with atopic dermatitis who demonstrate a clinical insensitivity to topical corticosteroids: a randomized, multicentre vehicle-controlled trial. Br J Dermatol. 2009; 161:435–443.
Article20. Williams MR, Gallo RL. Evidence that human skin microbiome dysbiosis promotes atopic dermatitis. J Invest Dermatol. 2017; 137:2460–2461.
Article21. Meylan P, Lang C, Mermoud S, Johannsen A, Norrenberg S, Hohl D, et al. Skin colonization by Staphylococcus aureus precedes the clinical diagnosis of atopic dermatitis in infancy. J Invest Dermatol. 2017; 137:2497–2504.22. Vu AT, Baba T, Chen X, Le TA, Kinoshita H, Xie Y, et al. Staphylococcus aureus membrane and diacylated lipopeptide induce thymic stromal lymphopoietin in keratinocytes through the Toll-like receptor 2-Toll-like receptor 6 pathway. J Allergy Clin Immunol. 2010; 126:985–993. 993.e1–993.e3.23. Byrd AL, Deming C, Cassidy SK, Harrison OJ, Ng WI, Conlan S, et al. Staphylococcus aureus and Staphylococcus epidermidis strain diversity underlying pediatric atopic dermatitis. Sci Transl Med. 2017; 9:eaal4651.24. Mayo B, Rachid CT, Alegría A, Leite AM, Peixoto RS, Delgado S. Impact of next generation sequencing techniques in food microbiology. Curr Genomics. 2014; 15:293–309.
Article25. Geoghegan JA, Irvine AD, Foster TJ. Staphylococcus aureus and atopic dermatitis: a complex and evolving relationship. Trends Microbiol. 2018; 26:484–497.26. Ong PY, Leung DY. Bacterial and viral infections in atopic dermatitis: a comprehensive review. Clin Rev Allergy Immunol. 2016; 51:329–337.
Article27. Nakatsuji T, Chen TH, Two AM, Chun KA, Narala S, Geha RS, et al. Staphylococcus aureus exploits epidermal barrier defects in atopic dermatitis to trigger cytokine expression. J Invest Dermatol. 2016; 136:2192–2200.28. Nakatsuji T, Chen TH, Narala S, Chun KA, Two AM, Yun T, et al. Antimicrobials from human skin commensal bacteria protect against Staphylococcus aureus and are deficient in atopic dermatitis. Sci Transl Med. 2017; 9:eaah4680.29. Kennedy EA, Connolly J, Hourihane JO, Fallon PG, McLean WH, Murray D, et al. Skin microbiome before development of atopic dermatitis: early colonization with commensal staphylococci at 2 months is associated with a lower risk of atopic dermatitis at 1 year. J Allergy Clin Immunol. 2017; 139:166–172.30. Berdyshev E, Goleva E, Bronova I, Dyjack N, Rios C, Jung J, et al. Lipid abnormalities in atopic skin are driven by type 2 cytokines. JCI Insight. 2018; 3:98006.
Article31. Goleva E, Berdyshev E, Leung DY. Epithelial barrier repair and prevention of allergy. J Clin Invest. 2019; 129:1463–1474.
Article32. Miller SJ, Aly R, Shinefeld HR, Elias PM. In vitro and in vivo antistaphylococcal activity of human stratum corneum lipids. Arch Dermatol. 1988; 124:209–215.33. Feuillie C, Vitry P, McAleer MA, Kezic S, Irvine AD, Geoghegan JA, et al. Adhesion of Staphylococcus aureus to corneocytes from atopic dermatitis patients is controlled by natural moisturizing factor levels. MBio. 2018; 9:e01184-18.
Article34. Howell MD, Boguniewicz M, Pastore S, Novak N, Bieber T, Girolomoni G, et al. Mechanism of HBD-3 deficiency in atopic dermatitis. Clin Immunol. 2006; 121:332–338.
Article35. Howell MD, Gallo RL, Boguniewicz M, Jones JF, Wong C, Streib JE, et al. Cytokine milieu of atopic dermatitis skin subverts the innate immune response to vaccinia virus. Immunity. 2006; 24:341–348.
Article36. Mallbris L, Carlén L, Wei T, Heilborn J, Nilsson MF, Granath F, et al. Injury downregulates the expression of the human cathelicidin protein hCAP18/LL-37 in atopic dermatitis. Exp Dermatol. 2010; 19:442–449.
Article37. Nakatsuji T, Gallo RL. The role of the skin microbiome in atopic dermatitis. Ann Allergy Asthma Immunol. 2019; 122:263–269.
Article38. Miajlovic H, Fallon PG, Irvine AD, Foster TJ. Effect of filaggrin breakdown products on growth of and protein expression by Staphylococcus aureus . J Allergy Clin Immunol. 2010; 126:1184–1190.e3.39. Brown SJ, McLean WH. One remarkable molecule: filaggrin. J Invest Dermatol. 2012; 132:751–762.
Article40. Jungersted JM, Hellgren LI, Jemec GB, Agner T. Lipids and skin barrier function--a clinical perspective. Contact Dermat. 2008; 58:255–262.41. Benenson S, Zimhony O, Dahan D, Solomon M, Raveh D, Schlesinger Y, et al. Atopic dermatitis--a risk factor for invasive Staphylococcus aureus infections: two cases and review. Am J Med. 2005; 118:1048–1051.42. Spaulding AR, Salgado-Pabón W, Kohler PL, Horswill AR, Leung DY, Schlievert PM. Staphylococcal and streptococcal superantigen exotoxins. Clin Microbiol Rev. 2013; 26:422–447.
Article43. Park KD, Pak SC, Park KK. The pathogenetic effect of natural and bacterial toxins on atopic dermatitis. Toxins (Basel). 2016; 9:E3.
Article44. Sonkoly E, Muller A, Lauerma AI, Pivarcsi A, Soto H, Kemeny L, et al. IL-31: a new link between T cells and pruritus in atopic skin inflammation. J Allergy Clin Immunol. 2006; 117:411–417.
Article45. Cornelissen C, Marquardt Y, Czaja K, Wenzel J, Frank J, Luscher-Firzlaff J, et al. IL-31 regulates differentiation and filaggrin expression in human organotypic skin models. J Allergy Clin Immunol. 2012; 129:426–433. 433.e1–433.e8.
Article46. Peschel A, Otto M. Phenol-soluble modulins and staphylococcal infection. Nat Rev Microbiol. 2013; 11:667–673.
Article47. Syed AK, Reed TJ, Clark KL, Boles BR, Kahlenberg JM. Staphlyococcus aureus phenol-soluble modulins stimulate the release of proinflammatory cytokines from keratinocytes and are required for induction of skin inflammation. Infect Immun. 2015; 83:3428–3437.48. Nakamura Y, Oscherwitz J, Cease KB, Chan SM, Muñoz-Planillo R, Hasegawa M, et al. Staphylococcus δ-toxin induces allergic skin disease by activating mast cells. Nature. 2013; 503:397–401.
Article49. Brauweiler AM, Goleva E, Leung DY. Th2 cytokines increase Staphylococcus aureus alpha toxin-induced keratinocyte death through the signal transducer and activator of transcription 6 (STAT6). J Invest Dermatol. 2014; 134:2114–2121.50. Claßen A, Kalali BN, Schnopp C, Andres C, Aguilar-Pimentel JA, Ring J, et al. TNF receptor I on human keratinocytes is a binding partner for staphylococcal protein A resulting in the activation of NF kappa B, AP-1, and downstream gene transcription. Exp Dermatol. 2011; 20:48–52.
Article51. Wang V, Keefer M, Ong PY. Antibiotic choice and methicillin-resistant Staphylococcus aureus rate in children hospitalized for atopic dermatitis. Ann Allergy Asthma Immunol. 2019; 122:314–317.52. Tauber M, Balica S, Hsu CY, Jean-Decoster C, Lauze C, Redoules D, et al. Staphylococcus aureus density on lesional and nonlesional skin is strongly associated with disease severity in atopic dermatitis. J Allergy Clin Immunol. 2016; 137:1272–1274.e3.53. Kong HH, Oh J, Deming C, Conlan S, Grice EA, Beatson MA, et al. Temporal shifts in the skin microbiome associated with disease flares and treatment in children with atopic dermatitis. Genome Res. 2012; 22:850–859.
Article54. Maintz L, Novak N. Modifications of the innate immune system in atopic dermatitis. J Innate Immun. 2011; 3:131–141.
Article55. Miedzobrodzki J, Kaszycki P, Bialecka A, Kasprowicz A. Proteolytic activity of Staphylococcus aureus strains isolated from the colonized skin of patients with acute-phase atopic dermatitis. Eur J Clin Microbiol Infect Dis. 2002; 21:269–276.56. Simpson EL, Villarreal M, Jepson B, Rafaels N, David G, Hanifin J, et al. Patients with atopic dermatitis colonized with Staphylococcus aureus have a distinct phenotype and endotype. J Invest Dermatol. 2018; 138:2224–2233.57. Fleury OM, McAleer MA, Feuillie C, Formosa-Dague C, Sansevere E, Bennett DE, et al. Clumping factor B promotes adherence of Staphylococcus aureus to corneocytes in atopic dermatitis. Infect Immun. 2017; 85:e00994-16.
Article58. Paller AS, Kong HH, Seed P, Naik S, Scharschmidt TC, Gallo RL, et al. The microbiome in patients with atopic dermatitis. J Allergy Clin Immunol. 2019; 143:26–35.
Article59. Clausen ML, Edslev SM, Andersen PS, Clemmensen K, Krogfelt KA, Agner T. Staphylococcus aureus colonization in atopic eczema and its association with filaggrin gene mutations. Br J Dermatol. 2017; 177:1394–1400.60. Yu J, Oh MH, Park JU, Myers AC, Dong C, Zhu Z, et al. Epicutaneous exposure to staphylococcal superantigen enterotoxin B enhances allergic lung inflammation via an IL-17A dependent mechanism. PLoS One. 2012; 7:e39032.
Article61. Jones AL, Curran-Everett D, Leung DY. Food allergy is associated with Staphylococcus aureus colonization in children with atopic dermatitis. J Allergy Clin Immunol. 2016; 137:1247–1248.e3.62. Leung DY, Calatroni A, Zaramela LS, LeBeau PK, Dyjack N, Brar K, et al. The nonlesional skin surface distinguishes atopic dermatitis with food allergy as a unique endotype. Sci Transl Med. 2019; 11:eaav2685.
Article63. Stevens DL, Bisno AL, Chambers HF, Dellinger EP, Goldstein EJ, Gorbach SL, et al. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America. Clin Infect Dis. 2014; 59:e10–e52.64. Clebak KT, Malone MA. Skin infections. Prim Care. 2018; 45:433–454.
Article65. Montravers P, Snauwaert A, Welsch C. Current guidelines and recommendations for the management of skin and soft tissue infections. Curr Opin Infect Dis. 2016; 29:131–138.
Article66. Eriksson S, van der Plas MJ, Mörgelin M, Sonesson A. Antibacterial and antibiofilm effects of sodium hypochlorite against Staphylococcus aureus isolates derived from patients with atopic dermatitis. Br J Dermatol. 2017; 177:513–521.67. Maarouf M, Shi VY. Bleach for atopic dermatitis. Dermatitis. 2018; 29:120–126.
Article68. Chopra R, Vakharia PP, Sacotte R, Silverberg JI. Efficacy of bleach baths in reducing severity of atopic dermatitis: a systematic review and meta-analysis. Ann Allergy Asthma Immunol. 2017; 119:435–440.
Article69. Raafat D, Otto M, Reppschläger K, Iqbal J, Holtfreter S. Fighting Staphylococcus aureus biofilms with monoclonal antibodies. Trends Microbiol. 2019; 27:303–322.70. Totté JE, van Doorn MB, Pasmans SG. Successful treatment of chronic Staphylococcus aureus-related dermatoses with the topical endolysin Staphefekt SA.100: a report of 3 cases. Case Rep Dermatol. 2017; 9:19–25.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The role of antiseptic agents in atopic dermatitis
- The association between Staphylococcus aureus colonization and food sensitization in children with atopic dermatitis
- Colonization of Staphylococcus aureus and sensitivity to antibiotics in children with atopic dermatitis
- The Effect of Skin-colonizing Staphylococcus aureus and Its Exotoxins on Childhood Atopic Dermatitis
- Correlation between serum 25-hydroxyvitamin D levels and methicillin - resistant Staphylococcus aureus skin colonization in atopic dermatitis