Brain Tumor Res Treat.
2019 Apr;7(1):44-47. 10.14791/btrt.2019.7.e26.
A Case of Recurrent Supratentorial Extraventricular Anaplastic Ependymoma in Adult
- Affiliations
-
- 1Department of Neurosurgery, Daegu Fatima Hospital, Daegu, Korea. nshojun@naver.com
- KMID: 2444795
- DOI: http://doi.org/10.14791/btrt.2019.7.e26
Abstract
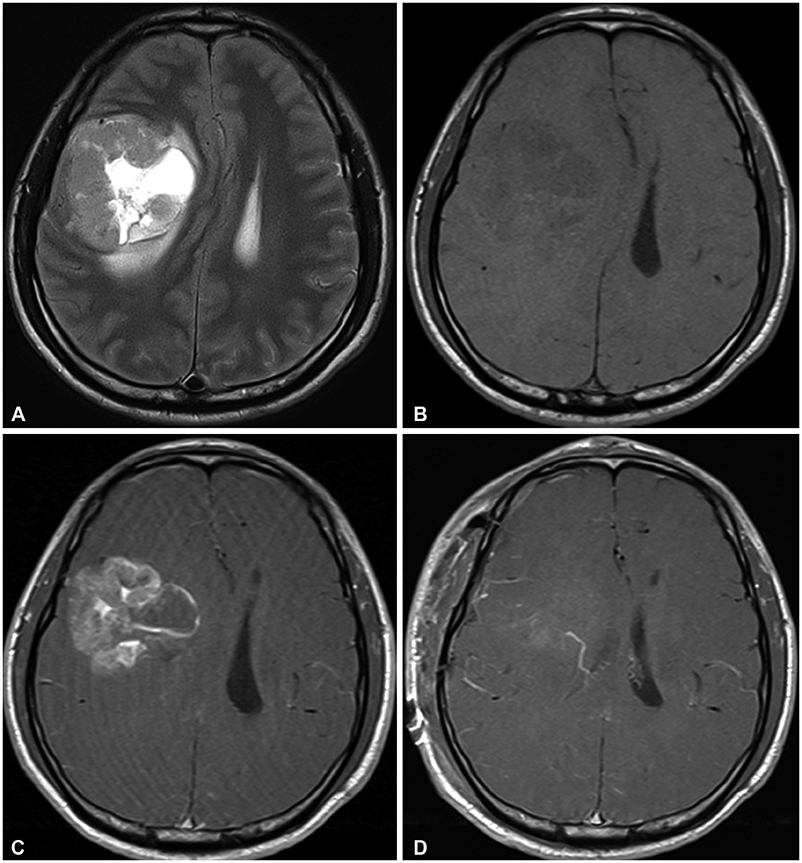
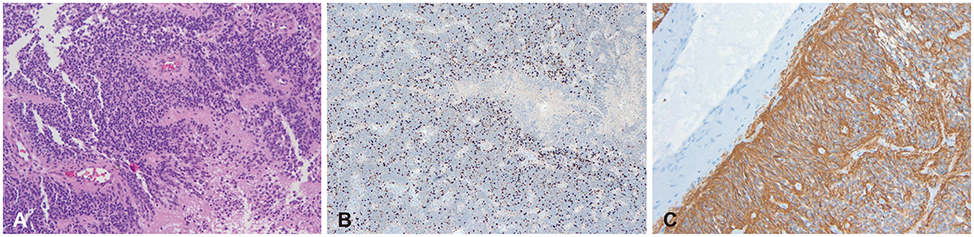
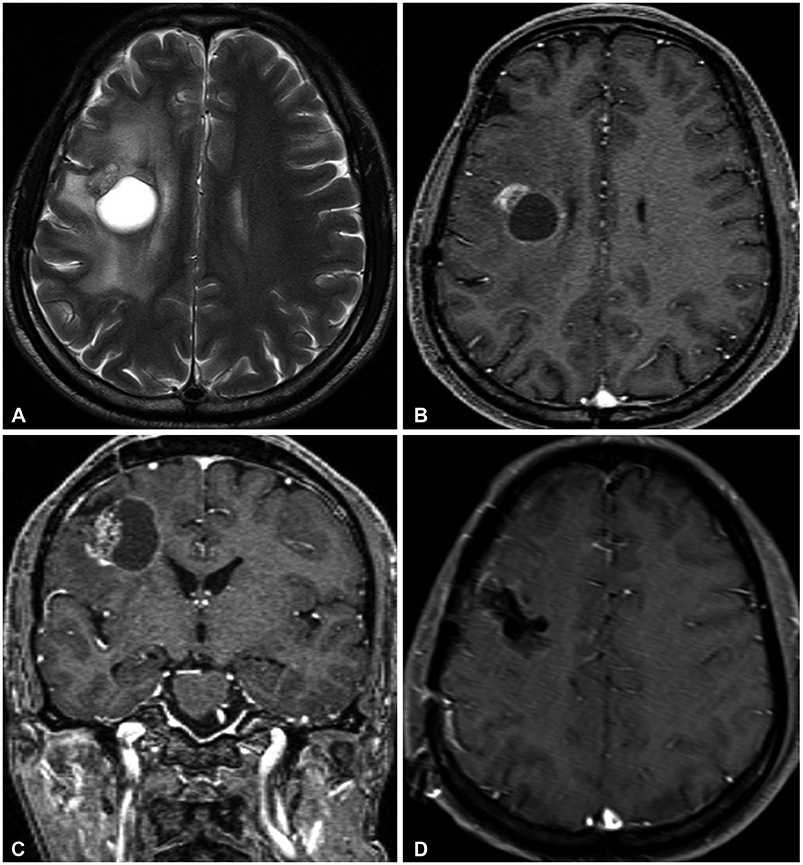
- Supratentorial extraventricular anaplastic ependymoma (SEAE) in adults is a relatively rare intracranial tumor. Because of the very low prevalence, only a few cases have been reported. According to a recent study, SEAE is associated with a poor prognosis and there is no definite consensus on optimal treatment. We report a case of an adult SEAE patient who had no recurrence until seven years after a gross total resection (GTR) followed by conventional radiotherapy. A 42-year-old male had a persistent mild headache, left facial palsy, dysarthria, and left hemiparesis. Preoperative neuroimaging revealed an anaplastic astrocytoma or supratentorial ependymoma in the right frontal lobe. A GTR was performed, followed by adjuvant radiotherapy. Histologic and immunohistochemical results revealed anaplastic ependymoma. After seven years of initial therapy, a regular follow-up MRI showed a 3-cm-sized partially cystic mass in the same area as the initial tumor. The patient underwent a craniotomy, and a GTR was performed. Histopathologic examination revealed recurrence of the SEAE. External radiotherapy was performed. The patient has been stable without any disease progression or complications for 12 months since the surgery for recurrent SEAE.
MeSH Terms
Figure
Reference
-
1. Chen L, Zou X, Wang Y, Mao Y, Zhou L. Central nervous system tumors: a single center pathology review of 34,140 cases over 60 years. BMC Clin Pathol. 2013; 13:14.
Article2. Reni M, Brandes AA, Vavassori V, et al. A multicenter study of the prognosis and treatment of adult brain ependymal tumors. Cancer. 2004; 100:1221–1229.
Article3. Miyazawa T, Hirose T, Nakanishi K, Uozumi Y, Tsuzuki N, Shima K. Supratentorial ectopic cortical ependymoma occurring with intratumoral hemorrhage. Brain Tumor Pathol. 2007; 24:35–40.
Article4. Roncaroli F, Consales A, Fioravanti A, Cenacchi G. Supratentorial cortical ependymoma: report of three cases. Neurosurgery. 2005; 57:E192.
Article5. Lavrador JP, Oliveira E, Teixeira JC, Lopes JP, Pimentel J, Carvalho MH. Adult supratentorial extraventricular anaplastic ependymoma: therapeutic approach and clinical review. Asian J Neurosurg. 2018; 13:105–109.
Article6. Byun J, Kim JH, Kim YH, Cho YH, Hong SH, Kim CJ. Supratentorial extraventricular ependymoma: retrospective analysis of 15 patients at a single institution. World Neurosurg. 2018; 118:e1–e9.
Article7. Vernet O, Farmer JP, Meagher-Villemure K, Montes JL. Supratentorial ectopic ependymoma. Can J Neurol Sci. 1995; 22:316–319.
Article8. Guyotat J, Signorelli F, Desme S, et al. Intracranial ependymomas in adult patients: analyses of prognostic factors. J Neurooncol. 2002; 60:255–268.9. Wang M, Zhang R, Liu X, et al. Supratentorial extraventricular ependymomas: a retrospective study focused on long-term outcomes and prognostic factors. Clin Neurol Neurosurg. 2018; 165:1–6.
Article10. Metellus P, Guyotat J, Chinot O, et al. Adult intracranial WHO grade II ependymomas: long-term outcome and prognostic factor analysis in a series of 114 patients. Neuro Oncol. 2010; 12:976–984.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Supratentorial Extraventricular Anaplastic Ependymoma Presenting with Repeated Intratumoral Hemorrhage
- Supratentorial Anaplastic Ependymoma Mimicking an Extra-Axial Tumor: A Case Report
- A Case of Supratentorial Intra-axial Ependymoma Showing Exophytic Growth
- Supratentorial Cortical Ependymoma in a 21-Month-Old Boy
- Correlation of Ki-67, p53 and bcl-2 Expression with Grade and Behavior of Ependymoma