Acute Crit Care.
2018 Nov;33(4):222-229. 10.4266/acc.2018.00136.
Oxygenation Index in the First 24 Hours after the Diagnosis of Acute Respiratory Distress Syndrome as a Surrogate Metric for Risk Stratification in Children
- Affiliations
-
- 1Department of Pediatrics, Yonsei University College of Medicine, Seoul, Korea. kwkim@yuhs.ac
- 2Department of Pediatrics, Hanyang University College of Medicine, Seoul, Korea.
- 3Sowha Children's Hospital, Seoul, Korea.
- KMID: 2441239
- DOI: http://doi.org/10.4266/acc.2018.00136
Abstract
- BACKGROUND
The diagnosis of pediatric acute respiratory distress syndrome (PARDS) is a pragmatic decision based on the degree of hypoxia at the time of onset. We aimed to determine whether reclassification using oxygenation metrics 24 hours after diagnosis could provide prognostic ability for outcomes in PARDS.
METHODS
Two hundred and eighty-eight pediatric patients admitted between January 1, 2010 and January 30, 2017, who met the inclusion criteria for PARDS were retrospectively analyzed. Reclassification based on data measured 24 hours after diagnosis was compared with the initial classification, and changes in pressure parameters and oxygenation were investigated for their prognostic value with respect to mortality.
RESULTS
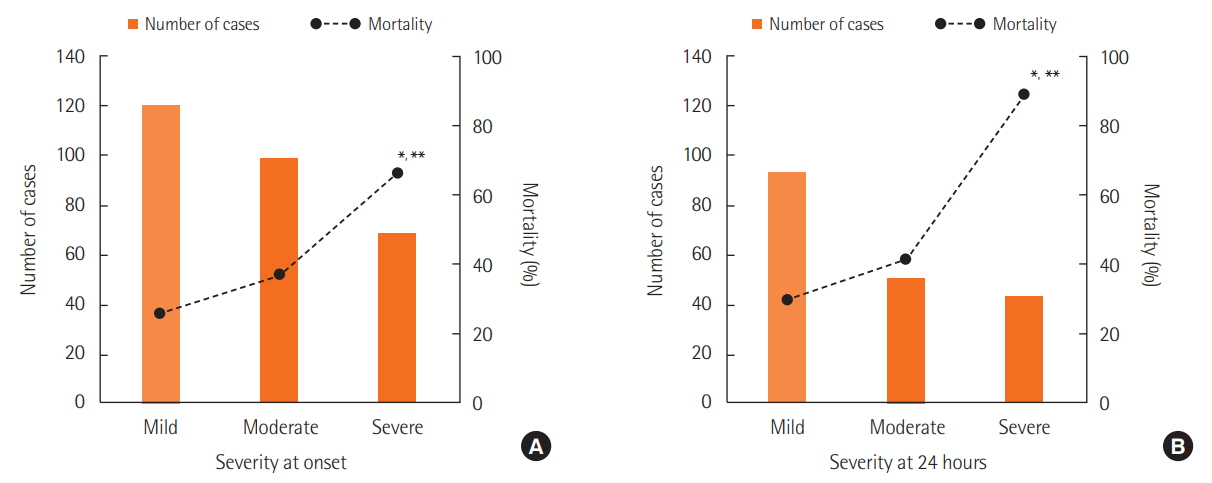
PARDS severity varied widely in the first 24 hours; 52.4% of patients showed an improvement, 35.4% showed no change, and 12.2% either showed progression of PARDS or died. Multivariate analysis revealed that mortality risk significantly increased for the severe group, based on classification using metrics collected 24 hours after diagnosis (adjusted odds ratio, 26.84; 95% confidence interval [CI], 3.43 to 209.89; P=0.002). Compared to changes in pressure variables (peak inspiratory pressure and driving pressure), changes in oxygenation (arterial partial pressure of oxygen to fraction of inspired oxygen) over the first 24 hours showed statistically better discriminative power for mortality (area under the receiver operating characteristic curve, 0.701; 95% CI, 0.636 to 0.766; P < 0.001).
CONCLUSIONS
Implementation of reclassification based on oxygenation metrics 24 hours after diagnosis effectively stratified outcomes in PARDS. Progress within the first 24 hours was significantly associated with outcomes in PARDS, and oxygenation response was the most discernable surrogate metric for mortality.
MeSH Terms
Figure
Reference
-
1. Pfenninger J, Gerber A, Tschäppeler H, Zimmermann A. Adult respiratory distress syndrome in children. J Pediatr. 1982; 101:352–7.
Article2. Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, et al. The American-European Consensus Conference on ARDS: definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med. 1994; 149(3 Pt 1):818–24.
Article3. ARDS Definition Task Force, Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, et al. Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012; 307:2526–33.4. Dahlem P, van Aalderen WM, Bos AP. Pediatric acute lung injury. Paediatr Respir Rev. 2007; 8:348–62.
Article5. Smith LS, Zimmerman JJ, Martin TR. Mechanisms of acute respiratory distress syndrome in children and adults: a review and suggestions for future research. Pediatr Crit Care Med. 2013; 14:631–43.6. Khemani RG, Smith LS, Zimmerman JJ, Erickson S; Pediatric Acute Lung Injury Consensus Conference Group. Pediatric acute respiratory distress syndrome: definition, incidence, and epidemiology: proceedings from the Pediatric Acute Lung Injury Consensus Conference. Pediatr Crit Care Med. 2015; 16(5 Suppl 1):S23–40.7. Schouten LR, Veltkamp F, Bos AP, van Woensel JB, Serpa Neto A, Schultz MJ, et al. Incidence and mortality of acute respiratory distress syndrome in children: a systematic review and meta-analysis. Crit Care Med. 2016; 44:819–29.8. López-Fernández Y, Azagra AM, de la Oliva P, Modesto V, Sánchez JI, Parrilla J, et al. Pediatric acute lung injury epidemiology and natural history study: incidence and outcome of the acute respiratory distress syndrome in children. Crit Care Med. 2012; 40:3238–45.9. Wong JJ, Jit M, Sultana R, Mok YH, Yeo JG, Koh JW, et al. Mortality in pediatric acute respiratory distress syndrome: a systematic review and meta-analysis. J Intensive Care Med. 2017; Jan. 1. [Epub]. https://doi.org/10.1177/0885066617705109.
Article10. Villar J, Pérez-Méndez L, López J, Belda J, Blanco J, Saralegui I, et al. An early PEEP/FIO2 trial identifies different degrees of lung injury in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2007; 176:795–804.11. Villar J, Pérez-Méndez L, Blanco J, Añón JM, Blanch L, Belda J, et al. A universal definition of ARDS: the PaO2/FiO2 ratio under a standard ventilatory setting: a prospective, multicenter alidation study. Intensive Care Med. 2013; 39:583–92.12. Trachsel D, McCrindle BW, Nakagawa S, Bohn D. Oxygenation index predicts outcome in children with acute hypoxemic respiratory failure. Am J Respir Crit Care Med. 2005; 172:206–11.
Article13. Yehya N, Servaes S, Thomas NJ. Characterizing degree of lung injury in pediatric acute respiratory distress syndrome. Crit Care Med. 2015; 43:937–46.
Article14. Parvathaneni K, Belani S, Leung D, Newth CJ, Khemani RG. Evaluating the performance of the pediatric acute lung injury consensus conference definition of acute respiratory distress syndrome. Pediatr Crit Care Med. 2017; 18:17–25.
Article15. Pediatric Acute Lung Injury Consensus Conference Group. Pediatric acute respiratory distress syndrome: consensus recommendations from the Pediatric Acute Lung Injury Consensus Conference. Pediatr Crit Care Med. 2015; 16:428–39.16. Khemani RG, Conti D, Alonzo TA, Bart RD 3rd, Newth CJ. Effect of tidal volume in children with acute hypoxemic respiratory failure. Intensive Care Med. 2009; 35:1428–37.
Article17. Amato MB, Meade MO, Slutsky AS, Brochard L, Costa EL, Schoenfeld DA, et al. Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med. 2015; 372:747–55.
Article18. Yehya N, Thomas NJ. Relevant outcomes in pediatric acute respiratory distress syndrome studies. Front Pediatr. 2016; 4:51.
Article19. Yehya N, Thomas NJ. Disassociating lung mechanics and oxygenation in pediatric acute respiratory distress syndrome. Crit Care Med. 2017; 45:1232–9.
Article20. Acute Respiratory Distress Syndrome Network, Brower RG, Matthay MA, Morris A, Schoenfeld D, Thompson BT, et al. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000; 342:1301–8.
Article21. de Jager P, Burgerhof JG, van Heerde M, Albers MJ, Markhorst DG, Kneyber MC. Tidal volume and mortality in mechanically ventilated children: a systematic review and meta-analysis of observational studies. Crit Care Med. 2014; 42:2461–72.22. Zimmerman JJ, Akhtar SR, Caldwell E, Rubenfeld GD. Incidence and outcomes of pediatric acute lung injury. Pediatrics. 2009; 124:87–95.
Article23. Bindl L, Dresbach K, Lentze MJ. Incidence of acute respiratory distress syndrome in German children and adolescents: a population-based study. Crit Care Med. 2005; 33:209–312.
Article24. De Luca D, Piastra M, Chidini G, Tissieres P, Calderini E, Essouri S, et al. The use of the Berlin definition for acute respiratory distress syndrome during infancy and early childhood: multicenter evaluation and expert consensus. Intensive Care Med. 2013; 39:2083–91.
Article25. Wong JJ, Phan HP, Phumeetham S, Ong JS, Chor YK, Qian S, et al. Risk stratification in pediatric acute respiratory distress syndrome: a multicenter observational study. Crit Care Med. 2017; 45:1820–8.26. Wong JJ, Loh TF, Testoni D, Yeo JG, Mok YH, Lee JH. Epidemiology of pediatric acute respiratory distress syndrome in Singapore: risk factors and predictive respiratory indices for mortality. Front Pediatr. 2014; 2:78.
Article27. Hu X, Qian S, Xu F, Huang B, Zhou D, Wang Y, et al. Incidence, management and mortality of acute hypoxemic respiratory failure and acute respiratory distress syndrome from a prospective study of Chinese paediatric intensive care network. Acta Paediatr. 2010; 99:715–21.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Successful use of extracorporeal membrane oxygenation for sudden aggravation of acute respiratory distress syndrome: A case report
- Treatment of acute respiratory failure: extracorporeal membrane oxygenation
- Clinical Manifestations and Diagnosis of Acute Respiratory Distress Syndrome
- Coagulopathy as a Prognostic Factor of Acute Lung Injury in Children
- Prone Position on Oxygenation in the Patient with Acute Respiratory Distress Syndrome after Decortication with Bilateral Empyectomy