Pediatr Gastroenterol Hepatol Nutr.
2019 Mar;22(2):193-200. 10.5223/pghn.2019.22.2.193.
Intestinal Spirochetosis: A Case Series and Review of the Literature
- Affiliations
-
- 1Kidz Health Castle, UZ Brussel, Vrije Universiteit Brussel, Brussels, Belgium. Yvan.Vandenplas@uzbrussel.be
- 2Department of Pathology, UZ Brussel, Vrije Universiteit Brussel, Brussels, Belgium.
- KMID: 2440594
- DOI: http://doi.org/10.5223/pghn.2019.22.2.193
Abstract
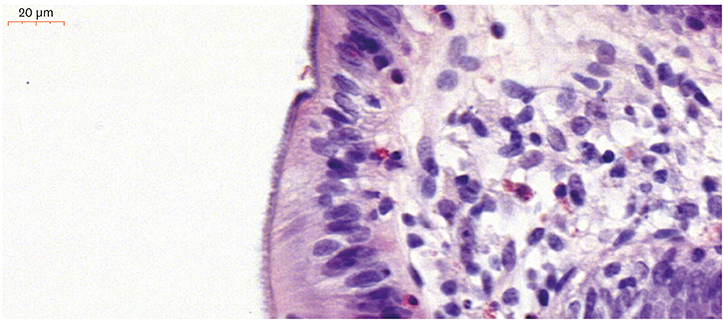
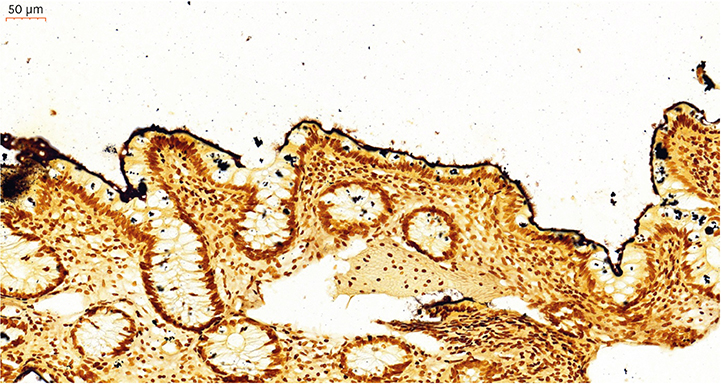
- A clinical suspicion of intestinal spirochetosis is required when patients have long lasting complaints of abdominal pain, diarrhea, rectal bleeding, weight loss, and nausea. An endoscopy with biopsies needs to be performed to confirm the diagnosis of intestinal spirochetosis. The diagnosis of intestinal spirochetosis is based on histological appearance. Intestinal spirochetosis can also be associated with other intestinal infections and juvenile polyps (JPs). JPs seem to be more frequent in patients with intestinal spirochetosis than in patients without intestinal spirochetosis. Intestinal spirochetosis in children should be treated with antibiotics. Metronidazole is the preferred option. In this article, we describe 4 cases of intestinal spirochetosis in a pediatric population and provide a review of the literature over the last 20 years. Intestinal spirochetosis is a rare infection that can cause a variety of severe symptom. It is diagnosed based on histological appearance.
Keyword
MeSH Terms
Figure
Reference
-
1. van Mook WN, Koek GH, van der Ven AJ, Ceelen TL, Bos RP. Human intestinal spirochaetosis: any clinical significance? Eur J Gastroenterol Hepatol. 2004; 16:83–87.2. Hovind-Hougen K, Birch-Andersen A, Henrik-Nielsen R, Orholm M, Pedersen JO, Teglbjaerg PS, et al. Intestinal spirochetosis: morphological characterization and cultivation of the spirochete Brachyspira aalborgi gen. nov., sp. nov. J Clin Microbiol. 1982; 16:1127–1136.
Article3. Lee JI, Hampson DJ. Genetic characterisation of intestinal spirochaetes and their association with disease. J Med Microbiol. 1994; 40:365–371.
Article4. Trott DJ, Stanton TB, Jensen NS, Hampson DJ. Phenotypic characteristics of Serpulina pilosicoli the agent of intestinal spirochaetosis. FEMS Microbiol Lett. 1996; 142:209–214.
Article5. Harland WA, Lee FD. Intestinal spirochaetosis. BMJ. 1967; 3:718–719.
Article6. Körner M, Gebbers JO. Clinical significance of human intestinal spirochetosis--a morphologic approach. Infection. 2003; 31:341–349.
Article7. Lee JI, Hampson DJ. Intestinal spirochaetes colonizing aborigines from communities in the remote north of Western Australia. Epidemiol Infect. 1992; 109:133–141.8. Walker MM, Talley NJ, Inganäs L, Engstrand L, Jones MP, Nyhlin H, et al. Colonic spirochetosis is associated with colonic eosinophilia and irritable bowel syndrome in a general population in Sweden. Hum Pathol. 2015; 46:277–283.
Article9. Ichimata S, Yoshizawa A, Kusakari M, Nakayama Y, Asaka S, Negishi T, et al. Human intestinal spirochetosis in Japanese patients aged less than 20 years: Histological analysis of colorectal biopsy and surgical specimens obtained from 479 patients. Pathol Int. 2017; 67:302–305.
Article10. Lindboe CF. The prevalence of human intestinal spirochetosis in Norway. Anim Health Res Rev. 2001; 2:117–119.
Article11. Tompkins DS, Foulkes SJ, Godwin PG, West AP. Isolation and characterisation of intestinal spirochaetes. J Clin Pathol. 1986; 39:535–541.
Article12. McMillan A, Lee FD. Sigmoidoscopic and microscopic appearance of the rectal mucosa in homosexual men. Gut. 1981; 22:1035–1041.
Article13. Helbling R, Osterheld MC, Vaudaux B, Jaton K, Nydegger A. Intestinal spirochetosis mimicking inflammatory bowel disease in children. BMC Pediatr. 2012; 12:163.
Article14. Carr NJ, Mahajan H, Tan KL, Sharma R. The histological features of intestinal spirochetosis in a series of 113 patients. Int J Surg Pathol. 2010; 18:144–148.
Article15. Ngwa T, Peng JL, Choi E, Tayarachakul S, Liangpunsakul S. Colonic spirochetosis in a 60-year-old immunocompetent patient: case report and review. J Investig Med High Impact Case Rep. 2016; 4:2324709616662671.16. Marthinsen L, Willén R, Carlén B, Lindberg E, Värendh G. Intestinal spirochetosis in eight pediatric patients from Southern Sweden. APMIS. 2002; 110:571–579.
Article17. Tsinganou E, Gebbers JO. Human intestinal spirochetosis--a review. Ger Med Sci. 2010; 8:Doc01.18. Koteish A, Kannangai R, Abraham SC, Torbenson M. Colonic spirochetosis in children and adults. Am J Clin Pathol. 2003; 120:828–832.
Article19. Carpentieri DF, Souza-Morones S, Gardetto JS, Ross HM, Downey K, Ingebo K, et al. Intestinal spirochetosis in children: five new cases and a 20-year review of the literature. Pediatr Dev Pathol. 2010; 13:471–475.
Article20. Peruzzi S, Gorrini C, Piccolo G, Calderaro A, Dettori G, Chezzi C. Human intestinal spirochaetosis in Parma: a focus on a selected population during 2002–2005. Acta Biomed. 2007; 78:128–132.21. Calderaro A, Gorrini C, Peruzzi S, Piccolo G, Dettori G, Chezzi C. Occurrence of human intestinal spirochetosis in comparison with infections by other enteropathogenic agents in an area of the Northern Italy. Diagn Microbiol Infect Dis. 2007; 59:157–163.
Article22. Omori S, Mabe K, Hatanaka K, Ono M, Matsumoto M, Takahashi M, et al. Human intestinal spirochetosis is significantly associated with sessile serrated adenomas/polyps. Pathol Res Pract. 2014; 210:440–443.
Article23. Calderaro A, Bommezzadri S, Gorrini C, Piccolo G, Peruzzi S, Villanacci V, et al. Infective colitis associated with human intestinal spirochetosis. J Gastroenterol Hepatol. 2007; 22:1772–1779.
Article24. Ogata S, Shimizu K, Nakanishi K. Human intestinal spirochetosis: right-side preference in the large intestine. Ann Diagn Pathol. 2015; 19:414–417.
Article25. Henrik-Nielsen R, Lundbeck FA, Teglbjaerg PS, Ginnerup P, Hovind-Hougen K. Intestinal spirochetosis of the vermiform appendix. Gastroenterology. 1985; 88:971–977.26. King NR, Fidda N, Gourley G. Colorectal spirochetosis in a child with rectal bleeding: case report and literature review. J Pediatr Gastroenterol Nutr. 2005; 41:673–675.
Article27. Ghosh JK, Goyal SK, Lamtha SC, Kaushik P, Behera MK, Abhilash VB, et al. Colonic spirochetosis in an immunocompetent child. Trop Gastroenterol. 2014; 35:266–269.
Article28. Nodit L, Parizhskaya M. Intestinal spirochetosis. Arch Pathol Lab Med. 2004; 128:823–824.
Article29. Heine RG, Ward PB, Mikosza AS, Bennett-Wood V, Robins-Browne RM, Hampson DJ. Brachyspira aalborgi infection in four Australian children. J Gastroenterol Hepatol. 2001; 16:872–875.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Coincident Occurrence of Intestinal Duplication Cyst and Type I and Type II Intestinal Atresias
- An Isolated Tubular Intestinal Loop in a Neonate with Type II Intestinal Atresia
- Hirschsprung's Disease Associated with Neonatal Intestinal Perforation
- Intestinal Obstruction Caused by Anisakiasis
- Time is Gut. Approaching Intestinal Leiomyositis: Case Presentation and Literature Review