J Adv Prosthodont.
2019 Feb;11(1):41-47. 10.4047/jap.2019.11.1.41.
Effects of different surface finishing protocols for zirconia on surface roughness and bacterial biofilm formation
- Affiliations
-
- 1Department of Prosthodontics, School of Dentistry, ITRD, Kyungpook National University, Daegu, Republic of Korea.
- 2Department of Microbiology and Immunology, School of Dentistry, Kyungpook National University, Daegu, Republic of Korea.
- 3Department of Periodontics and Endodontics, State University of New York at Buffalo, Buffalo, New York, United states of America.
- 4Department of Dentistry, Yonsei University Wonju College of Medicine, Wonju, Republic of Korea.
- 5Department of Prosthodontics, College of Dentistry, Yonsei University, Seoul, Republic of Korea. kwlee@yuhs.ac
- KMID: 2438930
- DOI: http://doi.org/10.4047/jap.2019.11.1.41
Abstract
- PURPOSE
Surface finishing of a zirconia restoration is essential after clinical adjustment. Herein, we investigated the effects of a surface finishing protocol for monolithic zirconia on final roughness and bacterial adherence.
MATERIALS AND METHODS
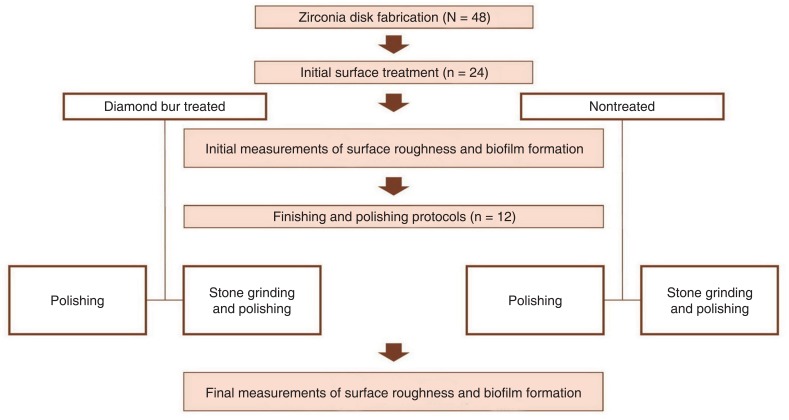
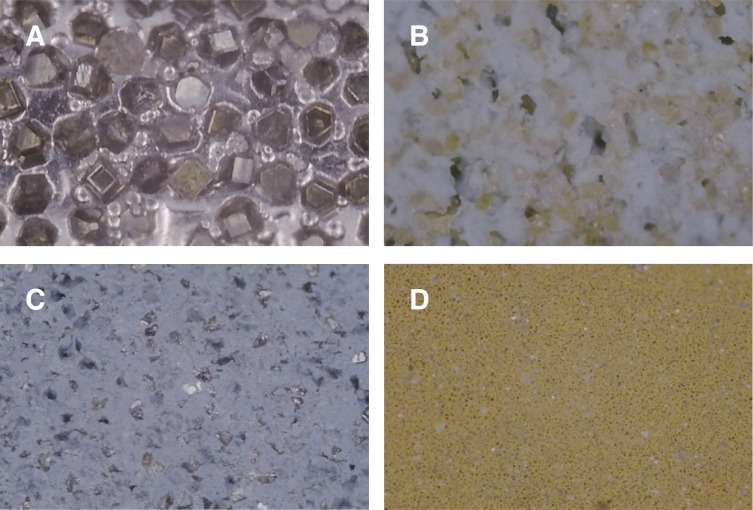
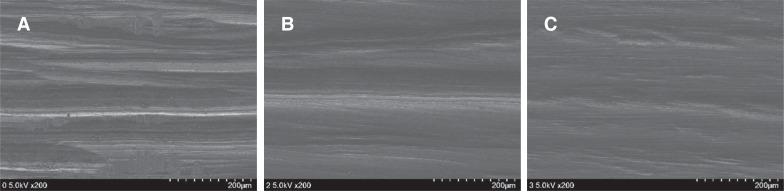
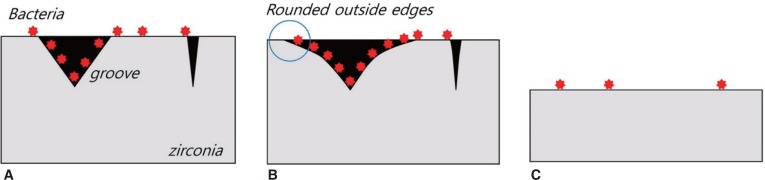
Forty-eight disk-shaped monolithic zirconia specimens were fabricated and divided into four groups (n = 12) based on initial surface treatment, finishing, and polishing protocols: diamond bur+polishing bur (DP group), diamond bur+stone grinding bur+polishing bur (DSP group), no diamond bur+polishing bur (NP group), and no diamond bur+stone grinding bur+polishing bur (NSP group). Initial and final surface roughness was measured with a profilometer, and shown using scanning electron microscope. Bacterial adhesion was evaluated by quantifying Streptococcus mutans in the biofilm. Kruskal-Wallis and Mann-Whitney U tests were used to compare results among groups, and two-way analysis of variance was used to evaluate the effects of grinding burs on final roughness (α=.05).
RESULTS
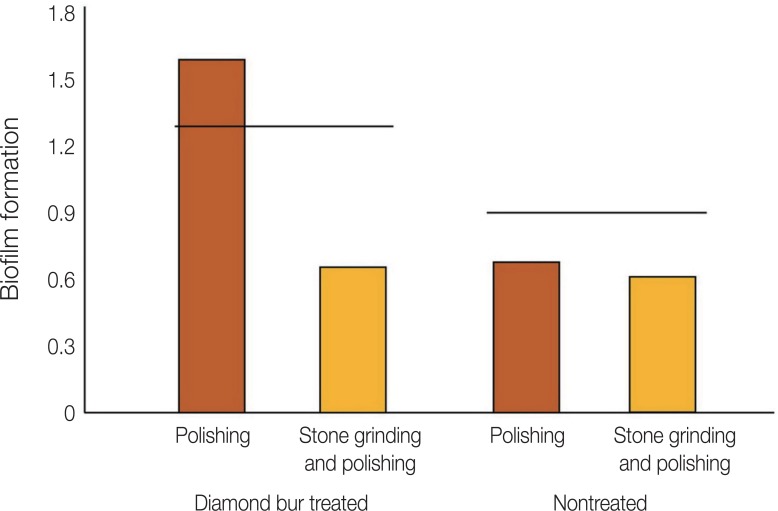
The DP group had the highest final Ra value, followed by the DSP, NP, and NSP groups. Use of the stone grinding bur as a coarse-finishing step significantly decreased final Ra values when a diamond bur was used (P < .001). Omission of the stone grinding bur increased biofilm formation on specimen surfaces. Combining a stone grinding bur with silicone polishing burs produced the smallest final biofilm values, regardless of the use of a diamond bur in initial surface treatment.
CONCLUSION
Coarse finishing of monolithic zirconia with a stone grinding bur significantly decreased final Ra values and bacterial biofilm formation when surfaces had been roughened by a diamond bur.
MeSH Terms
Figure
Reference
-
1. Caglar I, Ates SM, Yesil Duymus Z. The effect of various polishing systems on surface roughness and phase transformation of monolithic zirconia. J Adv Prosthodont. 2018; 10:132–137. PMID: 29713434.
Article2. Chavali R, Lin CP, Lawson NC. Evaluation of different polishing systems and speeds for dental zirconia. J Prosthodont. 2017; 26:410–418. PMID: 26618785.
Article3. Kim HK, Kim SH, Lee JB, Ha SR. Effects of surface treatments on the translucency, opalescence, and surface texture of dental monolithic zirconia ceramics. J Prosthet Dent. 2016; 115:773–779. PMID: 26809221.
Article4. Kim MJ, Oh SH, Kim JH, Ju SW, Seo DG, Jun SH, Ahn JS, Ryu JJ. Wear evaluation of the human enamel opposing different Y-TZP dental ceramics and other porcelains. J Dent. 2012; 40:979–988. PMID: 22892464.
Article5. Teughels W, Van Assche N, Sliepen I, Quirynen M. Effect of material characteristics and/or surface topography on biofilm development. Clin Oral Implants Res. 2006; 17(Suppl 2):68–81. PMID: 16968383.
Article6. Jones CS, Billington RW, Pearson GJ. The in vivo perception of roughness of restorations. Br Dent J. 2004; 196:42–45. PMID: 14966503.
Article7. Yuzugullu B, Celik C, Burak Ozcelik T, Erkut S, Yurdakul P, Ocal Y, Sener B. The effect of different polishing sequences on the adhesion of Streptococcus mutans to feldspathic Porcelain. J Adhes. 2016; 92:939–949.8. Bollen CM, Lambrechts P, Quirynen M. Comparison of surface roughness of oral hard materials to the threshold surface roughness for bacterial plaque retention: a review of the literature. Dent Mater. 1997; 13:258–269. PMID: 11696906.9. Lee BC, Jung GY, Kim DJ, Han JS. Initial bacterial adhesion on resin, titanium and zirconia in vitro. J Adv Prosthodont. 2011; 3:81–84. PMID: 21814616.10. Miyazaki T, Nakamura T, Matsumura H, Ban S, Kobayashi T. Current status of zirconia restoration. J Prosthodont Res. 2013; 57:236–261. PMID: 24140561.
Article11. Huh YH, Park CJ, Cho LR. Evaluation of various polishing systems and the phase transformation of monolithic zirconia. J Prosthet Dent. 2016; 116:440–449. PMID: 27061631.
Article12. Preis V, Grumser K, Schneider-Feyrer S, Behr M, Rosentritt M. The effectiveness of polishing kits: influence on surface roughness of zirconia. Int J Prosthodont. 2015; 28:149–151. PMID: 25822299.
Article13. Ho CM, Ding H, Chen X, Tsoi JK, Botelho MG. The effects of dry and wet grinding on the strength of dental zirconia. Ceram Int. 2018; 44:10451–10462.
Article14. Kosmac T, Oblak C, Jevnikar P, Funduk N, Marion L. Strength and reliability of surface treated Y-TZP dental ceramics. J Biomed Mater Res. 2000; 53:304–313. PMID: 10898871.15. Kosmac T, Oblak C, Jevnikar P, Funduk N, Marion L. The effect of surface grinding and sandblasting on flexural strength and reliability of Y-TZP zirconia ceramic. Dent Mater. 1999; 15:426–433. PMID: 10863444.16. Lee KR, Choe HC, Heo YR, Lee JJ, Son MK. Effect of different grinding burs on the physical properties of zirconia. J Adv Prosthodont. 2016; 8:137–143. PMID: 27141258.
Article17. Gilan I, Sivan A. Extracellular DNA plays an important structural role in the biofilm of the plastic degrading actinomycete Rhodo-coccus ruber. Adv Microbiol. 2013; 3:543–551.18. O'Toole GA. Microtiter dish biofilm formation assay. J Vis Exp. 2011; 47:2437.19. Han A, Tsoi JKH, Matinlinna JP, Chen Z. Influence of grit-Blasting and hydrofluoric acid etching treatment on surface characteristics and biofilm formation on zirconia. Coatings. 2017; 7:130.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of different finishing/polishing protocols and systems for monolithic zirconia on surface topography, phase transformation, and biofilm formation
- Surface Roughness and Microbial Adhesion After Finishing of Alkasite Restorative Material
- Comparison of biofilm on titanium and zirconia surfaces: in vivo study
- Effect of sintering programs and surface treatments on monolithic zirconia
- Investigation of effect of zirconia on osseointegration by surface treatments