Yonsei Med J.
2019 Feb;60(2):174-181. 10.3349/ymj.2019.60.2.174.
Prognostic Value of Lymphovascular Invasion in Node-Negative Upper Urinary Tract Urothelial Carcinoma Patients Undergoing Radical Nephroureterectomy
- Affiliations
-
- 1Department of Urology, The Affiliated Hospital of Qingdao University, Qingdao, China. zhangguiming9@126.com
- KMID: 2431634
- DOI: http://doi.org/10.3349/ymj.2019.60.2.174
Abstract
- PURPOSE
This study aimed to evaluate the prognostic impact of lymphovascular invasion (LVI) in patients treated with radical nephroureterectomy (RNU) for upper urinary tract urothelial carcinoma (UTUC).
MATERIALS AND METHODS
We collected data from 180 patients who were treated with RNU from 2005 to 2013 at our institution. The Kaplan-Meier method with log-rank test and Cox proportional hazards regression models were used for univariate and multivariate analyses.
RESULTS
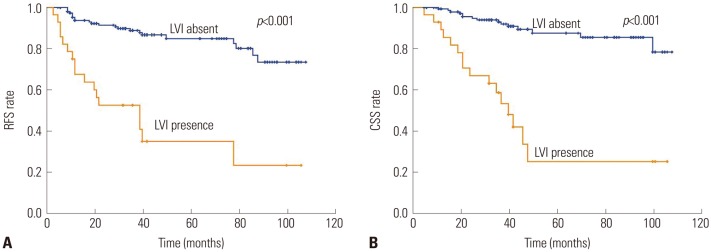
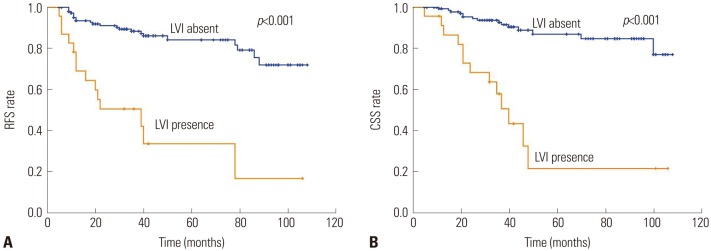
LVI was present in 28 patients (15.6%), which was associated with higher pathological tumor stage (p < 0.001), tumor necrosis (p=0.012), lymph node metastasis (p=0.017) and multifocality (p=0.012). On multivariate analysis, LVI was an independent prognostic factor of recurrence-free survival [RFS: hazard ratio (HR)=2.954; 95% confidence interval (CI)=1.539-5.671; p=0.001] and cancer-specific survival (CSS: HR=3.530; 95% CI=1.701-7.325; p=0.001) in all patients. In patients with node-negative UTUC, LVI was also a significant predictor of RFS (HR=3.732; 95% CI 1.866-7.464; p < 0.001) and CSS (HR=3.825; 95% CI=1.777-8.234; p=0.001).
CONCLUSION
LVI status was an independent predictor in patients with UTUC who underwent RNU. The estimate of LVI could help physicians identify high-risk patients and make a better medication regimen of adjuvant chemotherapy.
MeSH Terms
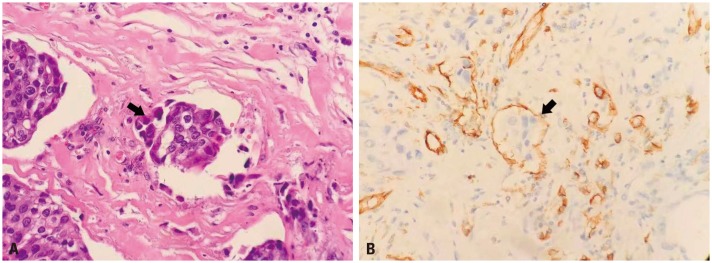
Figure
Reference
-
1. Rouprêt M, Babjuk M, Compérat E, Zigeuner R, Sylvester RJ, Burger M, et al. European Association of Urology Guidelines on Upper Urinary Tract Urothelial Carcinoma: 2017 update. Eur Urol. 2018; 73:111–122. PMID: 28867446.
Article2. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2017. CA Cancer J Clin. 2017; 67:7–30. PMID: 28055103.
Article3. Munoz JJ, Ellison LM. Upper tract urothelial neoplasms: incidence and survival during the last 2 decades. J Urol. 2000; 164:1523–1525. PMID: 11025695.
Article4. Xylinas E, Rink M, Margulis V, Karakiewicz P, Novara G, Shariat SF. Upper Tract Urothelial Carcinoma Collaboration (UTUCC). Multifocal carcinoma in situ of the upper tract is associated with high risk of bladder cancer recurrence. Eur Urol. 2012; 61:1069–1070. PMID: 22402109.
Article5. Margulis V, Shariat SF, Matin SF, Kamat AM, Zigeuner R, Kikuchi E, et al. Outcomes of radical nephroureterectomy: a series from the Upper Tract Urothelial Carcinoma Collaboration. Cancer. 2009; 115:1224–1233. PMID: 19156917.
Article6. Zhang XK, Zhang ZL, Yang P, Cai MY, Hu WM, Yun JP, et al. Tumor necrosis predicts poor clinical outcomes in patients with node-negative upper urinary tract urothelial carcinoma. Jpn J Clin Oncol. 2015; 45:1069–1075. PMID: 26355163.
Article7. Morizane S, Iwamoto H, Masago T, Yao A, Isoyama T, Sejima T, et al. Preoperative prognostic factors after radical nephroureterectomy in patients with upper urinary tract urothelial carcinoma. Int Urol Nephrol. 2013; 45:99–106. PMID: 23229166.
Article8. Verhoest G, Shariat SF, Chromecki TF, Raman JD, Margulis V, Novara G, et al. Predictive factors of recurrence and survival of upper tract urothelial carcinomas. World J Urol. 2011; 29:495–501. PMID: 21681525.
Article9. Sundar SS, Ganesan TS. Role of lymphangiogenesis in cancer. J Clin Oncol. 2007; 25:4298–4307. PMID: 17878481.
Article10. Mellouli M, Charfi S, Smaoui W, Kallel R, Khabir A, Bouacida M, et al. Prognostic role of lymphovascular invasion in patients with urothelial carcinoma of the upper urinary tract. Urol J. 2017; 14:5008–5012. PMID: 28853106.11. Lee HY, Li CC, Huang CN, Ke HL, Li WM, Liang PI, et al. Prognostic significance of lymphovascular invasion in upper urinary tract urothelial carcinoma is influenced by tumor location. Ann Surg Oncol. 2015; 22:1392–1400. PMID: 25239005.
Article12. Ku JH, Byun SS, Jeong H, Kwak C, Kim HH, Lee SE. Lymphovascular invasion as a prognostic factor in the upper urinary tract urothelial carcinoma: a systematic review and meta-analysis. Eur J Cancer. 2013; 49:2665–2680. PMID: 23721778.
Article13. Novara G, Matsumoto K, Kassouf W, Walton TJ, Fritsche HM, Bastian PJ, et al. Prognostic role of lymphovascular invasion in patients with urothelial carcinoma of the upper urinary tract: an international validation study. Eur Urol. 2010; 57:1064–1071. PMID: 20071073.
Article14. Kikuchi E, Margulis V, Karakiewicz PI, Roscigno M, Mikami S, Lotan Y, et al. Lymphovascular invasion predicts clinical outcomes in patients with node-negative upper tract urothelial carcinoma. J Clin Oncol. 2009; 27:612–618. PMID: 19075275.
Article15. Yoshida T, Kinoshita H, Shimada S, Sugi M, Matsuda T. Preoperative pyuria is a poor prognostic factor in patients with urothelial carcinoma of the upper urinary tract after surgery. Clin Genitourin Cancer. 2017; 15:e543–e550. PMID: 28110834.
Article16. Mathieu R, Klatte T, Margulis V, Karam JA, Rouprêt M, Seitz C, et al. Survivin is not an independent prognostic factor for patients with upper tract urothelial carcinoma: a multi-institutional study. Urol Oncol. 2015; 33:495.e15–495.e22.
Article17. Colin P, Ouzzane A, Yates DR, Audenet F, Pignot G, Arvin-Berod A, et al. Influence of positive surgical margin status after radical nephroureterectomy on upper urinary tract urothelial carcinoma survival. Ann Surg Oncol. 2012; 19:3613–3620. PMID: 22843187.
Article18. Raica M, Ribatti D. Targeting tumor lymphangiogenesis: an update. Curr Med Chem. 2010; 17:698–708. PMID: 20088760.
Article19. Yuan X, Zhu C, Wang M, Mo F, Du W, Ma X. Night shift work increases the risks of multiple primary cancers in women: a systematic review and meta-analysis of 61 articles. Cancer Epidemiol Biomarkers Prev. 2018; 27:25–40. PMID: 29311165.
Article20. Moch H, Cubilla AL, Humphrey PA, Reuter VE, Ulbright TM. The 2016 WHO Classification of Tumours of the Urinary System and Male Genital Organs-part A: renal, penile, and testicular tumours. Eur Urol. 2016; 70:93–105. PMID: 26935559.
Article21. Kahn HJ, Marks A. A new monoclonal antibody, D2-40, for detection of lymphatic invasion in primary tumors. Lab Invest. 2002; 82:1255–1257. PMID: 12218087.
Article22. Noma D, Inamura K, Matsuura Y, Hirata Y, Nakajima T, Yamazaki H, et al. Prognostic effect of lymphovascular invasion on TNM staging in stage I non-small-cell lung cancer. Clin Lung Cancer. 2018; 19:e109–e122. PMID: 29066222.
Article23. Ahmed Farag AF, Elbarmelgi MY, Azim HA, Abozeid AA, Mashhour AN. TNMF versus TNM in staging of colorectal cancer. Int J Surg. 2016; 27:147–150. PMID: 26836283.
Article24. Graziosi L, Marino E, Cavazzoni E, Donini A. Prognostic value of the seventh AJCC/UICC TNM classification of non-cardia gastric cancer. World J Surg Oncol. 2013; 11:103. PMID: 23687939.
Article25. Albers P, Siener R, Kliesch S, Weissbach L, Krege S, Sparwasser C, et al. Risk factors for relapse in clinical stage I nonseminomatous testicular germ cell tumors: results of the German Testicular Cancer Study Group Trial. J Clin Oncol. 2003; 21:1505–1512. PMID: 12697874.
Article26. Vassilakopoulou M, de la Motte Rouge T, Colin P, Ouzzane A, Khayat D, Dimopoulos MA, et al. Outcomes after adjuvant chemotherapy in the treatment of high-risk urothelial carcinoma of the upper urinary tract (UUT-UC): results from a large multicenter collaborative study. Cancer. 2011; 117:5500–5508. PMID: 21638278.27. Hellenthal NJ, Shariat SF, Margulis V, Karakiewicz PI, Roscigno M, Bolenz C, et al. Adjuvant chemotherapy for high risk upper tract urothelial carcinoma: results from the Upper Tract Urothelial Carcinoma Collaboration. J Urol. 2009; 182:900–906. PMID: 19616245.
Article28. Xylinas E, Necchi A. Young Academic Urologists Urothelial Carcinoma Group of the European Association of Urology. Re: effectiveness of adjuvant chemotherapy after radical nephroureterectomy for locally advanced and/or positive regional lymph node upper tract urothelial carcinoma. Eur Urol. 2017; 72:473–474. PMID: 28502719.
Article29. Shirotake S, Kikuchi E, Tanaka N, Matsumoto K, Miyazaki Y, Kobayashi H, et al. Impact of an adjuvant chemotherapeutic regimen on the clinical outcome in high risk patients with upper tract urothelial carcinoma: a Japanese multi-institution experience. J Urol. 2015; 193:1122–1128. PMID: 25444957.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Urothelial Tumors of the Upper Urinary Tract: Multiplicity and Prognostic Variables
- The Prognostic Significance of Blood and Lymphatic Vessels Invasion of Upper Urinary Tract Transitional Cell Carcinoma
- Identification of Significant Prognostic Tissue Markers Associated with Survival in Upper Urinary Tract Urothelial Carcinoma Patients Treated with Radical Nephroureterectomy: A Retrospective Immunohistochemical Analysis Using Tissue Microarray
- Impact of adjuvant chemotherapy in patients with upper tract urothelial carcinoma and lymphovascular invasion after radical nephroureterectomy
- Conditional Survival and Associated Prognostic Factors in Patients with Upper Tract Urothelial Carcinoma after Radical Nephroureterectomy: A Retrospective Study at a Single Institution