Ann Lab Med.
2018 Nov;38(6):503-511. 10.3343/alm.2018.38.6.503.
Complete Blood Count Reference Intervals and Patterns of Changes Across Pediatric, Adult, and Geriatric Ages in Korea
- Affiliations
-
- 1Department of Laboratory Medicine and Health Promotion Research Institute, Korea Association of Health Promotion, Seoul, Korea. cellonah@hanmail.net
- 2MEDIcheck LAB, Korea Association of Health Promotion, Cheongju, Korea.
- KMID: 2429114
- DOI: http://doi.org/10.3343/alm.2018.38.6.503
Abstract
- BACKGROUND
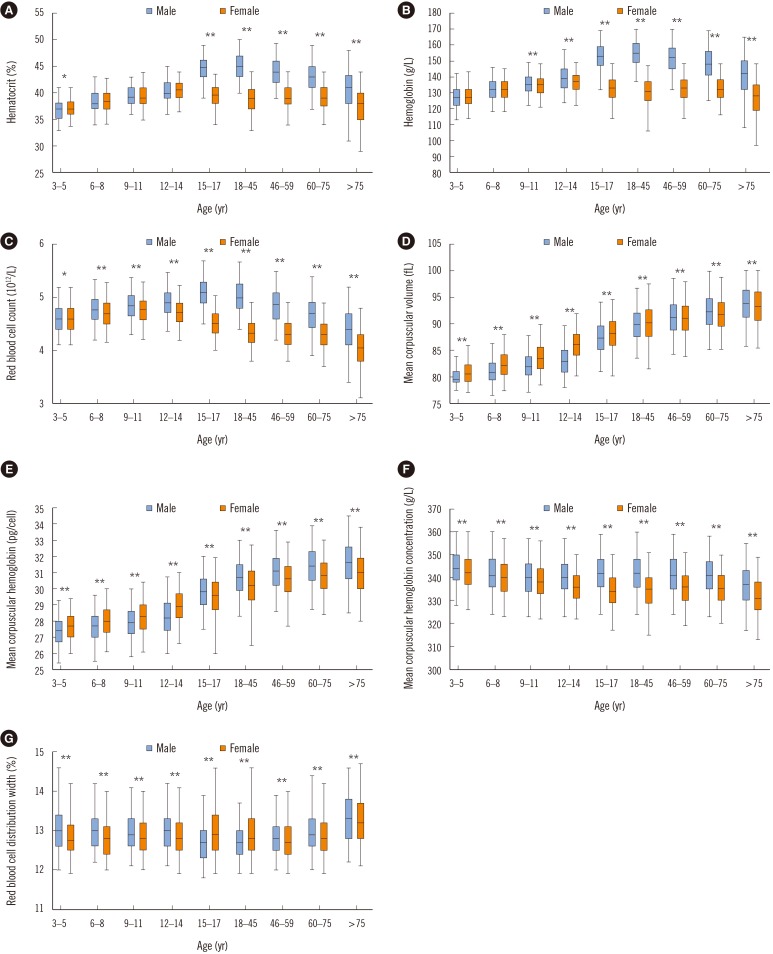
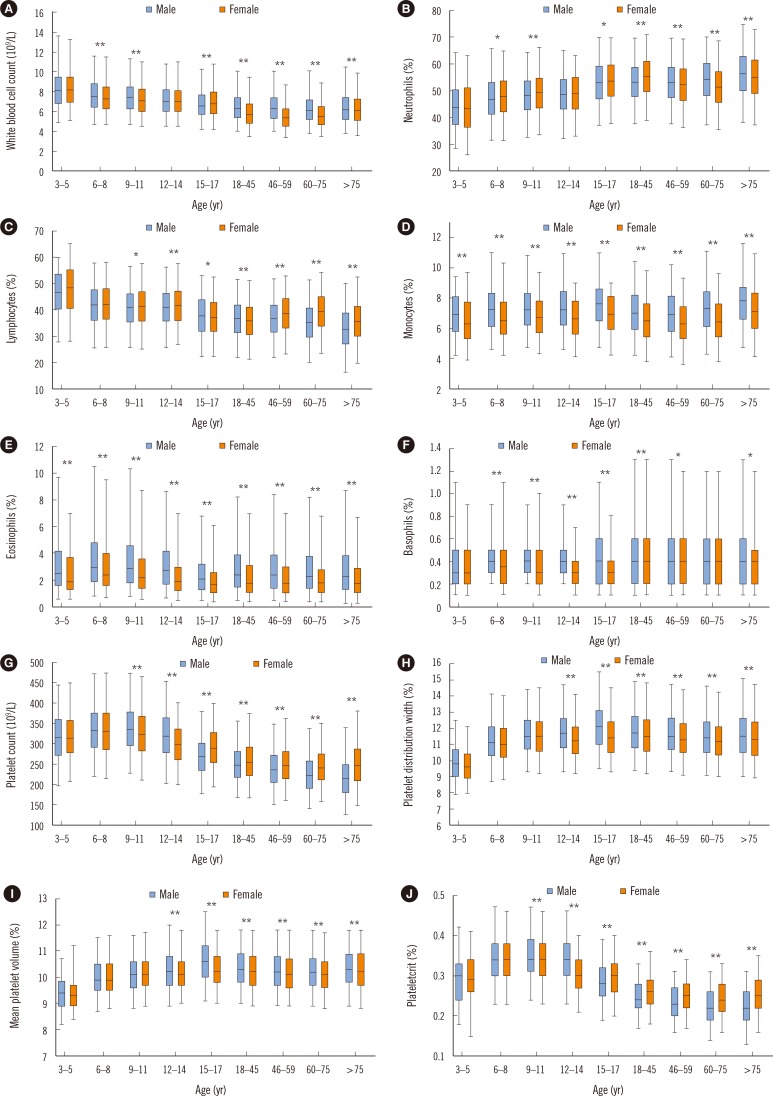
Sampling a healthy reference population to generate reference intervals (RIs) for complete blood count (CBC) parameters is not common for pediatric and geriatric ages. We established age- and sex-specific RIs for CBC parameters across pediatric, adult, and geriatric ages using secondary data, evaluating patterns of changes in CBC parameters.
METHODS
The reference population comprised 804,623 health examinees (66,611 aged 3-17 years; 564,280 aged 18-59 years; 173,732 aged 60-99 years), and, we excluded 22,766 examinees after outlier testing. The CBC parameters (red blood cell [RBC], white blood cell [WBC], and platelet parameters) from 781,857 examinees were studied. We determined statistically significant partitions of age and sex, and calculated RIs according to the CLSI C28-A3 guidelines.
RESULTS
RBC parameters increased with age until adulthood and decreased with age in males, but increased before puberty and then decreased with age in females. WBC and platelet counts were the highest in early childhood and decreased with age. Sex differences in each age group were noted: WBC count was higher in males than in females during adulthood, but platelet count was higher in females than in males from puberty onwards (P < 0.001). Neutrophil count was the lowest in early childhood and increased with age. Lymphocyte count decreased with age after peaking in early childhood. Eosinophil count was the highest in childhood and higher in males than in females. Monocyte count was higher in males than in females (P < 0.001).
CONCLUSIONS
We provide comprehensive age- and sex-specific RIs for CBC parameters, which show dynamic changes with both age and sex.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Establishment of Pediatric Reference Intervals for Routine Laboratory Tests in Korean Population: A Retrospective Multicenter Analysis
Ji Yeon Sung, Jong Do Seo, Dae-Hyun Ko, Min-Jeong Park, Sang Mee Hwang, Sohee Oh, Sail Chun, Moon-Woo Seong, Junghan Song, Sang Hoon Song, Sung Sup Park
Ann Lab Med. 2021;41(2):155-170. doi: 10.3343/alm.2021.41.2.155.
Reference
-
1. Friedberg RC, Souers R, Wagar EA, Stankovic AK, Valenstein PN. The origin of reference intervals. Arch Pathol Lab Med. 2007; 131:348–357. PMID: 17516737.2. Cheng CK, Chan J, Cembrowski GS, van Assendelft OW. Complete blood count reference interval diagrams derived from NHANES III: stratification by age, sex, and race. Lab Hematol. 2004; 10:42–53. PMID: 15070217.3. Adeli K, Raizman JE, Chen Y, Higgins V, Nieuwesteeg M, Abdelhaleem M, et al. Complex biological profile of hematologic markers across pediatric, adult, and geriatric ages: establishment of robust pediatric and adult reference intervals on the basis of the Canadian Health Measures Survey. Clin Chem. 2015; 61:1075–1086. PMID: 26044509.4. Ambayya A, Su AT, Osman NH, Nik-Samsudin NR, Khalid K, Chang KM, et al. Haematological reference intervals in a multiethnic population. PLoS One. 2014; 9:e91968. PMID: 24642526.5. Lee HR, Shin S, Yoon JH, Roh EY, Chang JY. Reference intervals of hematology and clinical chemistry analytes for 1-year-old Korean children. Ann Lab Med. 2016; 36:481–488. PMID: 27374715.6. Horowitz GL, Atlaie S, Boyd JC. Defining, establishing, and verifying reference intervals in the clinical laboratory; approved guideline. C28-A3c. Wayne, PA: Clinical and Laboratory Standards Institute;2010.7. Cho SM, Lee SG, Kim HS, Kim JH. Establishing pediatric reference intervals for 13 biochemical analytes derived from normal subjects in a pediatric endocrinology clinic in Korea. Clin Biochem. 2014; 47:268–271. PMID: 25241678.8. Bachman E, Travison TG, Basaria S, Davda MN, Guo W, Li M, et al. Testosterone induces erythrocytosis via increased erythropoietin and suppressed hepcidin: evidence for a new erythropoietin/hemoglobin set point. J Gerontol A Biol Sci Med Sci. 2014; 69:725–735. PMID: 24158761.9. Wakeman L, Al-Ismail S, Benton A, Beddall A, Gibbs A, Hartnell S, et al. Robust, routine haematology reference ranges for healthy adults. Int J Lab Hematol. 2007; 29:279–283. PMID: 17617078.10. Looker AC, Dallman PR, Carroll MD, Gunter EW, Johnson CL. Prevalence of iron deficiency in the United States. JAMA. 1997; 277:973–976. PMID: 9091669.11. Food and Agricultural Organization of the United Nations. WHO. World declaration and plan of action for nutrition: International Conference on Nutrition. Updated on Dec 1992. http://www.who.int/nutrition/publications/policies/icn_worlddeclaration_planofaction1992/en/.12. WHO. Iron deficiency anaemia: assessment, prevention and control: a guide for programme managers. Updated on Aug 2001. http://www.who.int/nutrition/publications/micronutrients/anaemia_iron_deficiency/WHO_NHD_01.3/en/.13. Ershler WB. Biological interactions of aging and anemia: a focus on cytokines. J Am Geriatr Soc. 2003; 51(S3):S18–S21. PMID: 12588568.14. Balducci L. Epidemiology of anemia in the elderly: information on diagnostic evaluation. J Am Geriatr Soc. 2003; 51(S3):S2–S9. PMID: 12588565.15. Verthelyi D. Sex hormones as immunomodulators in health and disease. Int Immunopharmacol. 2001; 1:983–993. PMID: 11407317.16. Roshan TM, Rosline H, Ahmed SA, Rapiaah M, Wan Zaidah A, Khattak MN. Hematological reference values of healthy Malaysian population. Int J Lab Hematol. 2009; 31:505–512. PMID: 18498389.17. Ishiguro A, Nakahata T, Matsubara K, Hayashi Y, Kato T, Suzuki Y, et al. Age-related changes in thrombopoietin in children: reference interval for serum thrombopoietin levels. Br J Haematol. 1999; 106:884–888. PMID: 10519988.18. Daly ME. Determinants of platelet count in humans. Haematologica. 2011; 96:10–13. PMID: 21193429.19. Kadikoylu G, Yavasoglu I, Bolaman Z, Senturk T. Platelet parameters in women with iron deficiency anemia. J Natl Med Assoc. 2006; 98:398–402. PMID: 16573304.20. Beguin Y. Erythropoietin and platelet production. Haematologica. 1999; 84:541–547. PMID: 10366799.21. Giles C. The platelet count and mean platelet volume. Br J Haematol. 1981; 48:31–37. PMID: 7248189.22. Buckley MF, James JW, Brown DE, Whyte GS, Dean MG, Chesterman CN, et al. A novel approach to the assessment of variations in the human platelet count. Thromb Haemost. 2000; 83:480–484. PMID: 10744157.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Establishing Reference Intervals for Complete Blood Cell Count in Healthy Korean Elderly Individuals
- Complete Blood Count Reference Values of Donated Cord Blood from Korean Neonates
- Influence of Waist Circumference Index of Metabolic Syndrome on the Establishment of Reference Intervals
- Establishment of Pediatric Reference Intervals for Routine Laboratory Tests in Korean Population: A Retrospective Multicenter Analysis
- Reference Intervals for Platelet Parameters in Korean Adults Using ADVIA 2120