Tuberc Respir Dis.
2017 Oct;80(4):377-384. 10.4046/trd.2017.0041.
Short-term Evaluation of a Comprehensive Education Program Including Inhaler Training and Disease Management on Chronic Obstructive Pulmonary Disease
- Affiliations
-
- 1Department of Internal Medicine, Konkuk University School of Medicine, Seoul, Korea.
- 2Department of Pulmonary and Critical Care Medicine, Ajou University School of Medicine, Suwon, Korea. jhpamc@hanmail.net
- 3Department of Clinical Pharmacology, Konkuk University School of Medicine, Seoul, Korea.
- 4Office of Biostatistics, Department of Humanities and Social Medicine, Ajou University School of Medicine, Suwon, Korea.
- 5Division of Pulmonary, Allergy and Critical Care Medicine, Department of Internal Medicine, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 6Division of Pulmonology, Department of Internal Medicine, Hanyang University Guri Hospital, Hanyang University College of Medicine, Guri, Korea.
- 7Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, Seoul National University College of Medicine, Seoul, Korea.
- 8Department of Pulmonary and Critical Care Medicine, Hallym University Kangdong Sacred Heart Hospital, Seoul, Korea.
- 9Department of Internal Medicine, Wonju Severance Christian Hospital, Wonju, Korea.
- 10Department of Internal Medicine, Inje University Seoul Paik Hospital, Seoul, Korea.
- KMID: 2420580
- DOI: http://doi.org/10.4046/trd.2017.0041
Abstract
- BACKGROUND
Proper education regarding inhaler usage and optimal management of chronic obstructive pulmonary disease (COPD) is essential for effectively treating patients with COPD. This study was conducted to evaluate the effects of a comprehensive education program including inhaler training and COPD management.
METHODS
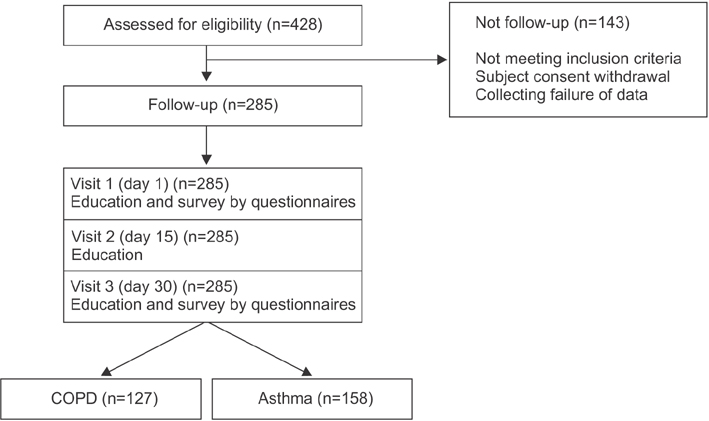
We enlisted 127 patients with COPD on an outpatient basis at 43 private clinics in Korea. The patients were educated on inhaler usage and disease management for three visits across 2 weeks. Physicians and patients were administered a COPD assessment test (CAT) and questionnaires about the correct usage of inhalers and management of COPD before commencement of this program and after their third visit.
RESULTS
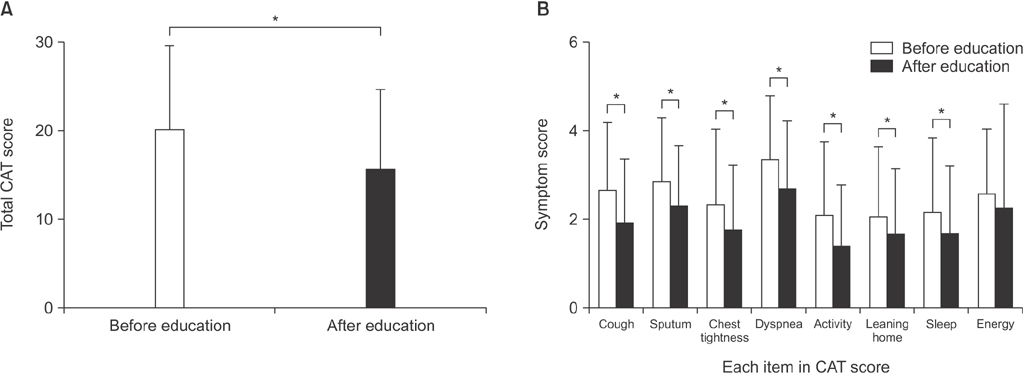
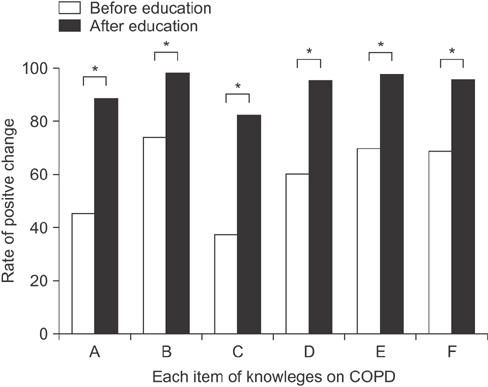
The outcomes of 127 COPD patients were analyzed. CAT scores (19.6±12.5 vs. 15.1±12.3) improved significantly after this program (p<0.05). Patients with improved CAT scores of 4 points or more had a better understanding of COPD management and the correct technique for using inhalers than those who did not have improved CAT scores (p<0.05).
CONCLUSION
A comprehensive education program including inhaler training and COPD management at a primary care setting improved CAT scores and led to patients' better understanding of COPD management.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Pharmacotherapy for chronic obstructive pulmonary disease
In Ae Kim, Yong Bum Park, Kwang Ha Yoo
J Korean Med Assoc. 2018;61(9):545-551. doi: 10.5124/jkma.2018.61.9.545.
Reference
-
1. Rabe KF, Hurd S, Anzueto A, Barnes PJ, Buist SA, Calverley P, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2007; 176:532–555.2. Yoo KH, Kim YS, Sheen SS, Park JH, Hwang YI, Kim SH, et al. Prevalence of chronic obstructive pulmonary disease in Korea: the fourth Korean National Health and Nutrition Examination Survey, 2008. Respirology. 2011; 16:659–665.3. Kim SA, Lee JH, Kim EK, Kim TH, Kim WJ, Lee JH, et al. Outcome of inhaler withdrawal in patients receiving triple therapy for COPD. Tuberc Respir Dis. 2016; 79:22–30.4. Zwerink M, Brusse-Keizer M, van der Valk PD, Zielhuis GA, Monninkhof EM, van der Palen J, et al. Self management for patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2014; (3):CD002990.5. Aydemir Y. Assessment of the factors affecting the failure to use inhaler devices before and after training. Respir Med. 2015; 109:451–458.6. Jarvis S, Ind PW, Shiner RJ. Inhaled therapy in elderly COPD patients; time for re-evaluation? Age Ageing. 2007; 36:213–218.7. VanderSchaaf K, Olson KL, Billups S, Hartsfield CL, Rice M. Self-reported inhaler use in patients with chronic obstructive pulmonary disease. Respir Med. 2010; 104:99–106.8. Pothirat C, Chaiwong W, Phetsuk N, Pisalthanapuna S, Chetsadaphan N, Choomuang W. Evaluating inhaler use technique in COPD patients. Int J Chron Obstruct Pulmon Dis. 2015; 10:1291–1298.9. George J, Kong DC, Thoman R, Stewart K. Factors associated with medication nonadherence in patients with COPD. Chest. 2005; 128:3198–3204.10. Vestbo J, Anderson JA, Calverley PM, Celli B, Ferguson GT, Jenkins C, et al. Adherence to inhaled therapy, mortality and hospital admission in COPD. Thorax. 2009; 64:939–943.11. Bryant J, McDonald VM, Boyes A, Sanson-Fisher R, Paul C, Melville J. Improving medication adherence in chronic obstructive pulmonary disease: a systematic review. Respir Res. 2013; 14:109.12. Lee JY, Yoo KH, Kim DK, Kim SH, Kim TE, Kim TH, et al. Effects of educational interventions for chronic airway disease on primary care. J Korean Med Sci. 2016; 31:1069–1074.13. Bhatt SP, Kim YI, Wells JM, Bailey WC, Ramsdell JW, Foreman MG, et al. FEV1/FEV6 to diagnose airflow obstruction. Comparisons with computed tomography and morbidity indices. Ann Am Thorac Soc. 2014; 11:335–341.14. Vandevoorde J, Verbanck S, Schuermans D, Kartounian J, Vincken W. FEV1/FEV6 and FEV6 as an alternative for FEV1/FVC and FVC in the spirometric detection of airway obstruction and restriction. Chest. 2005; 127:1560–1564.15. Gupta N, Pinto LM, Morogan A, Bourbeau J. The COPD assessment test: a systematic review. Eur Respir J. 2014; 44:873–884.16. Roggeri A, Micheletto C, Roggeri DP. Inhalation errors due to device switch in patients with chronic obstructive pulmonary disease and asthma: critical health and economic issues. Int J Chron Obstruct Pulmon Dis. 2016; 11:597–602.17. Tommelein E, Mehuys E, Van Hees T, Adriaens E, Van Bortel L, Christiaens T, et al. Effectiveness of pharmaceutical care for patients with chronic obstructive pulmonary disease (PHARMACOP): a randomized controlled trial. Br J Clin Pharmacol. 2014; 77:756–766.18. Vanfleteren LE, Spruit MA, Groenen M, Gaffron S, van Empel VP, Bruijnzeel PL, et al. Clusters of comorbidities based on validated objective measurements and systemic inflammation in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2013; 187:728–735.19. George J, Kong DC, Stewart K. Adherence to disease management programs in patients with COPD. Int J Chron Obstruct Pulmon Dis. 2007; 2:253–262.20. Wedzicha JA, Seemungal TA. COPD exacerbations: defining their cause and prevention. Lancet. 2007; 370:786–796.21. Bourbeau J, Ford G, Zackon H, Pinsky N, Lee J, Ruberto G. Impact on patients' health status following early identification of a COPD exacerbation. Eur Respir J. 2007; 30:907–913.22. Donaldson GC, Seemungal TA, Bhowmik A, Wedzicha JA. Relationship between exacerbation frequency and lung function decline in chronic obstructive pulmonary disease. Thorax. 2002; 57:847–852.23. Langsetmo L, Platt RW, Ernst P, Bourbeau J. Underreporting exacerbation of chronic obstructive pulmonary disease in a longitudinal cohort. Am J Respir Crit Care Med. 2008; 177:396–401.24. Seemungal TA, Donaldson GC, Bhowmik A, Jeffries DJ, Wedzicha JA. Time course and recovery of exacerbations in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2000; 161:1608–1613.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Continued Innovation in Respiratory Care: The Importance of Inhaler Devices
- Inhalation medications in chronic airway disease
- Inhaler Competency and Medication Adherence in Older Adults and Adults with Obstructive Lung Disease
- The Effect of Repeated Education using a Computerized Scoring System for the Proper Use of Inhalation Medicine
- Pulmonary Rehabilitation in Chronic Obstructive Pulmonary Disease