Obstet Gynecol Sci.
2018 Mar;61(2):253-260. 10.5468/ogs.2018.61.2.253.
Serum visfatin levels in non-obese women with polycystic ovary syndrome and matched controls
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Healthcare System Gangnam Center, Seoul National University Hospital, Seoul, Korea.
- 2The Institute of Reproductive Medicine and Population, Medical Research Center, Seoul National University College of Medicine, Seoul, Korea. ymchoi@snu.ac.kr
- 3Department of Obstetrics and Gynecology, Seoul National University College of Medicine, Seoul, Korea.
- 4Department of Obstetrics and Gynecology, Maria Fertility Hospital, Seoul, Korea.
- 5Department of Obstetrics and Gynecology, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, Seoul, Korea.
- 6Department of Obstetrics and Gynecology, Graduate School of Medicine, Dongguk University, Seoul, Korea.
- KMID: 2420180
- DOI: http://doi.org/10.5468/ogs.2018.61.2.253
Abstract
OBJECTIVE
The purpose of the current study was to compare the circulating levels of visfatin between women with polycystic ovary syndrome (PCOS) and those without PCOS and to assess the correlations between visfatin levels and various parameters.
METHODS
This case-control study recruited 74 PCOS patients and 74 age- and body mass index (BMI)-matched controls. Serum visfatin levels were evaluated using the enzyme-linked immunosorbent assay. Women with PCOS were divided into 2 subgroups based on the presence of clinical or biochemical hyperandrogenism. The possible differences in serum visfatin levels between the hyperandrogenic and non-hyperandrogenic groups were also assessed.
RESULTS
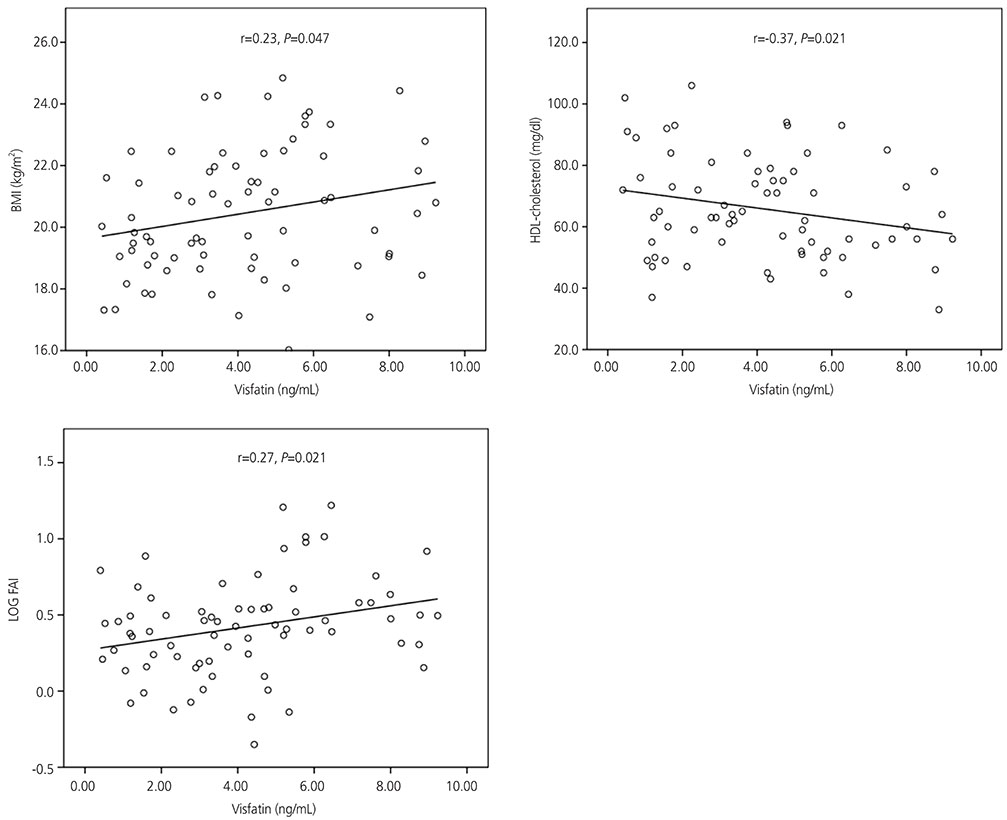
Visfatin levels in PCOS patients were similar to those in the controls. However, hyperandrogenic patients had significantly higher mean serum visfatin levels than those in non-hyperandrogenic patients (3.87 ng/mL; 95% confidence intervals [CIs], 3.09-4.85 in hyperandrogenic group vs. 2.69 ng/mL; 95% CIs, 2.06-3.52 in non-hyperandrogenic group; P=0.038). In women with PCOS, visfatin levels positively correlated with BMI (r=0.23; P=0.047) and the log free androgen index (FAI) (r=0.27; P=0.021) and negatively correlated with high-density lipoprotein (HDL) cholesterol levels (r=−0.37; P=0.025). Except for HDL cholesterol levels, these correlations were also observed in controls.
CONCLUSION
Visfatin levels in PCOS patients were similar to those in the controls. However, hyperandrogenic patients showed significantly higher serum visfatin levels than those of non-hyperandrogenic patients, and visfatin had a positive linear correlation with FAI in both PCOS patients and controls.
MeSH Terms
Figure
Cited by 1 articles
-
Gingival crevicular fluid levels of visfatin in patients with chronic periodontitis and polycystic ovary syndrome
Forouzan Saljoughi, Khadijeh Nasri, Mojtaba Bayani
Obstet Gynecol Sci. 2020;63(1):87-93. doi: 10.5468/ogs.2020.63.1.87.
Reference
-
1. Conway G, Dewailly D, Diamanti-Kandarakis E, Escobar-Morreale HF, Franks S, Gambineri A, et al. The polycystic ovary syndrome: a position statement from the European Society of Endocrinology. Eur J Endocrinol. 2014; 171:1–29.
Article2. Dumesic DA, Oberfield SE, Stener-Victorin E, Marshall JC, Laven JS, Legro RS. Scientific statement on the diagnostic criteria, epidemiology, pathophysiology, and molecular genetics of polycystic ovary syndrome. Endocr Rev. 2015; 36:487–525.
Article3. Berndt J, Klöting N, Kralisch S, Kovacs P, Fasshauer M, Schön MR, et al. Plasma visfatin concentrations and fat depot-specific mRNA expression in humans. Diabetes. 2005; 54:2911–2916.
Article4. Tan BK, Chen J, Digby JE, Keay SD, Kennedy CR, Randeva HS. Increased visfatin messenger ribonucleic acid and protein levels in adipose tissue and adipocytes in women with polycystic ovary syndrome: parallel increase in plasma visfatin. J Clin Endocrinol Metab. 2006; 91:5022–5028.
Article5. Cheng KH, Chu CS, Lee KT, Lin TH, Hsieh CC, Chiu CC, et al. Adipocytokines and proinflammatory mediators from abdominal and epicardial adipose tissue in patients with coronary artery disease. Int J Obes. 2008; 32:268–274.
Article6. Wang P, Xu TY, Guan YF, Su DF, Fan GR, Miao CY. Perivascular adipose tissue-derived visfatin is a vascular smooth muscle cell growth factor: role of nicotinamide mononucleotide. Cardiovasc Res. 2009; 81:370–380.
Article7. Zahorska-Markiewicz B, Olszanecka-Glinianowicz M, Janowska J, Kocełak P, Semik-Grabarczyk E, Holecki M, et al. Serum concentration of visfatin in obese women. Metabolism. 2007; 56:1131–1134.
Article8. Hug C, Lodish HF. Medicine. Visfatin: a new adipokine. Science. 2005; 307:366–367.
Article9. Dahl TB, Yndestad A, Skjelland M, Øie E, Dahl A, Michelsen A, et al. Increased expression of visfatin in macrophages of human unstable carotid and coronary atherosclerosis: possible role in inflammation and plaque destabilization. Circulation. 2007; 115:972–980.10. Moschen AR, Kaser A, Enrich B, Mosheimer B, Theurl M, Niederegger H, et al. Visfatin, an adipocytokine with proinflammatory and immunomodulating properties. J Immunol. 2007; 178:1748–1758.
Article11. Lee WJ, Wu CS, Lin H, Lee IT, Wu CM, Tseng JJ, et al. Visfatin-induced expression of inflammatory mediators in human endothelial cells through the NF-kappaB pathway. Int J Obes. 2009; 33:465–472.12. Kadoglou NP, Sailer N, Moumtzouoglou A, Kapelouzou A, Tsanikidis H, Vitta I, et al. Visfatin (nampt) and ghrelin as novel markers of carotid atherosclerosis in patients with type 2 diabetes. Exp Clin Endocrinol Diabetes. 2010; 118:75–80.
Article13. Romacho T, Sánchez-Ferrer CF, Peiró C. Visfatin/Nampt: an adipokine with cardiovascular impact. Mediators Inflamm. 2013; 2013:946427.
Article14. Curat CA, Wegner V, Sengenès C, Miranville A, Tonus C, Busse R, et al. Macrophages in human visceral adipose tissue: increased accumulation in obesity and a source of resistin and visfatin. Diabetologia. 2006; 49:744–747.
Article15. Diamanti-Kandarakis E, Paterakis T, Kandarakis HA. Indices of low-grade inflammation in polycystic ovary syndrome. Ann N Y Acad Sci. 2006; 1092:175–186.
Article16. Mannerås-Holm L, Leonhardt H, Kullberg J, Jennische E, Odén A, Holm G, et al. Adipose tissue has aberrant morphology and function in PCOS: enlarged adipocytes and low serum adiponectin, but not circulating sex steroids, are strongly associated with insulin resistance. J Clin Endocrinol Metab. 2011; 96:E304–E311.
Article17. Chan TF, Chen YL, Chen HH, Lee CH, Jong SB, Tsai EM. Increased plasma visfatin concentrations in women with polycystic ovary syndrome. Fertil Steril. 2007; 88:401–405.
Article18. Kowalska I, Straczkowski M, Nikolajuk A, Adamska A, Karczewska-Kupczewska M, Otziomek E, et al. Serum visfatin in relation to insulin resistance and markers of hyperandrogenism in lean and obese women with polycystic ovary syndrome. Hum Reprod. 2007; 22:1824–1829.
Article19. Panidis D, Farmakiotis D, Rousso D, Katsikis I, Delkos D, Piouka A, et al. Plasma visfatin levels in normal weight women with polycystic ovary syndrome. Eur J Intern Med. 2008; 19:406–412.
Article20. Ozkaya M, Cakal E, Ustun Y, Engin-Ustun Y. Effect of metformin on serum visfatin levels in patients with polycystic ovary syndrome. Fertil Steril. 2010; 93:880–884.
Article21. Plati E, Kouskouni E, Malamitsi-Puchner A, Boutsikou M, Kaparos G, Baka S. Visfatin and leptin levels in women with polycystic ovaries undergoing ovarian stimulation. Fertil Steril. 2010; 94:1451–1456.
Article22. Seow KM, Hwang JL, Wang PH, Ho LT, Juan CC. Expression of visfatin mRNA in peripheral blood mononuclear cells is not correlated with visfatin mRNA in omental adipose tissue in women with polycystic ovary syndrome. Hum Reprod. 2011; 26:2869–2873.
Article23. Pepene CE. Evidence for visfatin as an independent predictor of endothelial dysfunction in polycystic ovary syndrome. Clin Endocrinol (Oxf). 2012; 76:119–125.
Article24. Olszanecka-Glinianowicz M, Kocełak P, Nylec M, Chudek J, Zahorska-Markiewicz B. Circulating visfatin level and visfatin/insulin ratio in obese women with metabolic syndrome. Arch Med Sci. 2012; 8:214–218.25. Lajunen TK, Purhonen AK, Haapea M, Ruokonen A, Puukka K, Hartikainen AL, et al. Full-length visfatin levels are associated with inflammation in women with polycystic ovary syndrome. Eur J Clin Invest. 2012; 42:321–328.
Article26. Güdücü N, İşçi H, Görmüş U, Yiğiter AB, Dünder I. Serum visfatin levels in women with polycystic ovary syndrome. Gynecol Endocrinol. 2012; 28:619–623.
Article27. Farshchian F, Ramezani Tehrani F, Amirrasouli H, Rahimi Pour H, Hedayati M, Kazerouni F, et al. Visfatin and resistin serum levels in normal-weight and obese women with polycystic ovary syndrome. Int J Endocrinol Metab. 2014; 12:e15503.
Article28. Gümüş Ü, Güzel AI, Topcu HO, Timur H, Yılmaz N, Danışman N. Plasma visfatin levels in adolescents with polycystic ovary syndrome: a prospective case-control study. J Pediatr Adolesc Gynecol. 2015; 28:249–253.
Article29. Chae SJ, Kim JJ, Choi YM, Hwang KR, Jee BC, Ku SY, et al. Clinical and biochemical characteristics of polycystic ovary syndrome in Korean women. Hum Reprod. 2008; 23:1924–1931.
Article30. Kim JJ, Chae SJ, Choi YM, Hwang SS, Hwang KR, Kim SM, et al. Assessment of hirsutism among Korean women: results of a randomly selected sample of women seeking pre-employment physical check-up. Hum Reprod. 2011; 26:214–220.
Article31. Kim JJ, Choi YM, Kang JH, Hwang KR, Chae SJ, Kim SM, et al. Carotid intima-media thickness in mainly non-obese women with polycystic ovary syndrome and age-matched controls. Obstet Gynecol Sci. 2013; 56:249–255.
Article32. Rotterdam ESHRE/ASRM-Sponsored PCOS consensus workshop group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome (PCOS). Hum Reprod. 2004; 19:41–47.33. World Health Organization Western Pacific Region. International Association for the Study of Obesity. International Obesity Task Force. The Asia-Pacific perspective: redefining obesity and its treatment. Sydney: Health Communications Australia Pty Limited;2000.34. Yildiz BO, Bozdag G, Otegen U, Harmanci A, Boynukalin K, Vural Z, et al. Visfatin and retinol-binding protein 4 concentrations in lean, glucose-tolerant women with PCOS. Reprod Biomed Online. 2010; 20:150–155.
Article35. Tsouma I, Kouskouni E, Demeridou S, Boutsikou M, Hassiakos D, Chasiakou A, et al. Correlation of visfatin levels and lipoprotein lipid profiles in women with polycystic ovary syndrome undergoing ovarian stimulation. Gynecol Endocrinol. 2014; 30:516–519.
Article36. Gen R, Akbay E, Muslu N, Sezer K, Cayan F. Plasma visfatin level in lean women with PCOS: relation to proinflammatory markers and insulin resistance. Gynecol Endocrinol. 2009; 25:241–245.
Article37. Jongwutiwes T, Lertvikool S, Leelaphiwat S, Rattanasiri S, Jultanmas R, Weerakiet S. Serum visfatin in Asian women with polycystic ovary syndrome. Gynecol Endocrinol. 2009; 25:536–542.
Article38. Dıkmen E, Tarkun I, Cantürk Z, Cetınarslan B. Plasma visfatin level in women with polycystic ovary syndrome. Gynecol Endocrinol. 2011; 27:475–479.39. Nestler JE, Powers LP, Matt DW, Steingold KA, Plymate SR, Rittmaster RS, et al. A direct effect of hyperinsulinemia on serum sex hormone-binding globulin levels in obese women with the polycystic ovary syndrome. J Clin Endocrinol Metab. 1991; 72:83–89.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Gingival crevicular fluid levels of visfatin in patients with chronic periodontitis and polycystic ovary syndrome
- Studies on Fibrinolytic System Behavior in Women with Polycystic Ovary Syndrome
- Association of Serum Adiponectin Levels with Insulin Resistance in Women with Polycystic Ovary Syndrome
- The Effect of Metformin in Non-Obese Women with Polycystic Ovary Syndrome; Pilot Stud
- The Relationship between Plasma Visfatin Level, Obesity and Metabolic Syndrome in Women Without Diabetes