J Korean Neurosurg Soc.
2018 Sep;61(5):608-617. 10.3340/jkns.2018.0118.
Prospective Multicenter Surveillance Study of Surgical Site Infection after Spinal Surgery in Korea : A Preliminary Study
- Affiliations
-
- 1Department of Neurosurgery, Gil Medical Center, Gachon University College of Medicine, Incheon, Korea. gtyee@gilhospital.com
- KMID: 2420069
- DOI: http://doi.org/10.3340/jkns.2018.0118
Abstract
OBJECTIVE
This study aimed to investigate the rates, types, and risk factors of surgical site infection (SSI) following spinal surgery using data from a Korean SSI surveillance system that included diagnoses made by surgeons.
METHODS
This was a prospective observational study of patients who underwent spinal surgeries at 42 hospitals in South Korea from January 2017 to December 2017. The procedures included spinal fusion, laminectomy, discectomy, and corpectomy. Univariate and multivariate logistic regression analyses were performed.
RESULTS
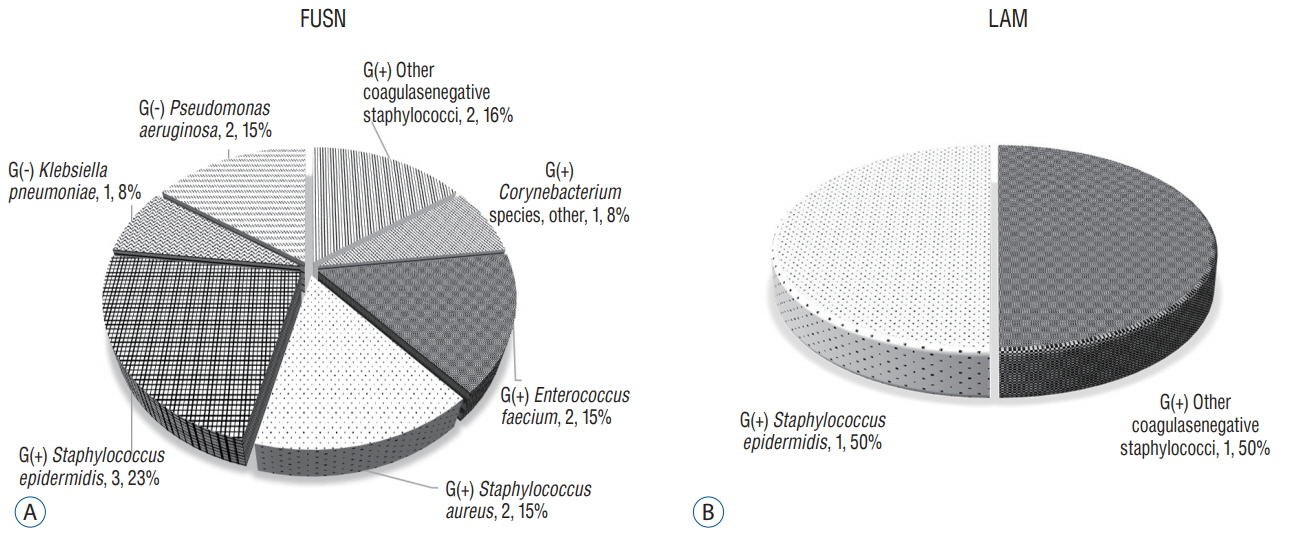
Of the 3080 cases included, 30 showed infection, and the overall SSI rate was 1.0% (an incidence of 1.2% in spinal fusion and 0.6% in laminectomy). Deep incisional infections were the most common type of SSIs (46.7%). Gram-positive bacteria caused 80% of the infections, and coagulase-negative staphylococci, including Staphylococcus epidermidis, accounted for 58% of the gram-positive bacteria. A longer preoperative hospital stay was significantly associated with the incidence of SSI after both spinal fusion and laminectomy (p=0.013, p < 0.001). A combined operation also was associated with SSI after laminectomy (p=0.032).
CONCLUSION
An SSI surveillance system is important for the accurate analysis of SSI. The incidence of SSI after spinal surgery assessed by a national surveillance system was 1.0%. Additional data collection will be needed in future studies to analyze SSI in spinal surgery.
Keyword
MeSH Terms
Figure
Reference
-
References
1. American Society of Anesthesiologists. ASA Physical Status Classification System. Available at : https://www.asahq.org/resources/clinical-information/asa-physical-status-classification-system.2. Blam OG, Vaccaro AR, Vanichkachorn JS, Albert TJ, Hilibrand AS, Minnich JM, et al. Risk factors for surgical site infection in the patient with spinal injury. Spine (Phila Pa 1976). 28:1475–1480. 2003.
Article3. Centers for Disease Control and Prevention (CDC). National Healthcare Safety Network (NHSN): Surgical site infection (SSI) event. Available at : http://www.cdc.gov/nhsn/pdfs/pscmanual/9pscssicurrent.pdf.4. Centers for Disease Control and Prevention (CDC). National Healthcare Safety Network (NHSN): Surveillance Definitions for Specific Types of Infections. Available at : https://www.cdc.gov/nhsn/pdfs/pscmanual/17pscnosinfdef_current.pdf.5. Shaw FE, Kohl KS, Lee LM, Thacker SB; Centers for Disease Control and Prevention (CDC). Public health then and now: Celebrating 50 years of MMWR at CDC. Introduction. MMWR Suppl. 60:2–6. 2011.6. Dixon RE; Centers for Disease Control and Prevention (CDC). Control of health-care-associated infections, 1961-2011. MMWR Suppl. 60:58–63. 2011.7. Emori TG, Gaynes RP. An overview of nosocomial infections, including the role of the microbiology laboratory. Clin Microbiol Rev. 6:428–442. 1993.
Article8. Fang A, Hu SS, Endres N, Bradford DS. Risk factors for infection after spinal surgery. Spine (Phila Pa 1976). 30:1460–1465. 2005.
Article9. Favre B, Hugonnet S, Correa L, Sax H, Rohner P, Pittet D. Nosocomial bacteremia: clinical significance of a single blood culture positive for coagulase-negative staphylococci. Infect Control Hosp Epidemiol. 26:697–702. 2005.
Article10. Gaynes RP, Culver DH, Horan TC, Edwards JR, Richards C, Tolson JS. Surgical site infection (SSI) rates in the United States, 1992-1998: the National Nosocomial Infections Surveillance System basic SSI risk index. Clin Infect Dis 33 Suppl. 2:S69–S77. 2001.
Article11. Haley RW, Culver DH, White JW, Morgan WM, Emori TG, Munn VP, et al. The efficacy of infection surveillance and control programs in preventing nosocomial infections in US hospitals. Am J Epidemiol. 121:182–205. 1985.
Article12. Jeong SJ, Choi SW, Youm JY, Kim HW, Ha HG, Yi JS. Microbiology and epidemiology of infectious spinal disease. J Korean Neurosurg Soc. 56:21–27. 2014.
Article13. John Jr JF, Davidson R, Low DE. Staphylococcus epidermidis and other coagulase-negative staphylococci. Available at : http://www.antimicrobe.org/new/b234.asp#t11.14. Klein JD, Hey LA, Yu CS, Klein BB, Coufal FJ, Young EP, et al. Perioperative nutrition and postoperative complications in patients undergoing spinal surgery. Spine (Phila Pa 1976). 21:2676–2682. 1996.
Article15. Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR; The Hospital Infection Control Practices Advisory Committee. Guideline for prevention of surgical site infection, 1999. Am J Infect Control. 27:97–134. 1999.
Article16. Marculescu CE, Berbari EF, Cockerill FR 3rd, Osmon DR. Unusual aerobic and anaerobic bacteria associated with prosthetic joint infections. Clin Orthop Relat Res. 451:55–63. 2006.
Article17. Moazzez A, Kelso RL, Towfigh S, Sohn H, Berne TV, Mason RJ. Breast abscess bacteriologic features in the era of community-acquired methicillin-resistant Staphylococcus aureus epidemics. Arch Surg. 142:881–884. 2007.
Article18. Olsen MA, Mayfield J, Lauryssen C, Polish LB, Jones M, Vest J, et al. Risk factors for surgical site infection in spinal surgery. J Neurosurg. 98(2 Suppl):149–155. 2003.
Article19. Olsen MA, Nepple JJ, Riew KD, Lenke LG, Bridwell KH, Mayfield J, et al. Risk factors for surgical site infection following orthopaedic spinal operations. J Bone Joint Surg Am. 90:62–69. 2008.
Article20. Perry JW, Montgomerie JZ, Swank S, Gilmore DS, Maeder K. Wound infections following spinal fusion with posterior segmental spinal instrumentation. Clin Infect Dis. 24:558–561. 1997.
Article21. Picada R, Winter RB, Lonstein JE, Denis F, Pinto MR, Smith MD, et al. Postoperative deep wound infection in adults after posterior lumbosacral spine fusion with instrumentation: incidence and management. J Spinal Disord. 13:42–45. 2000.
Article22. Plowman R. The socioeconomic burden of hospital acquired infection. Euro Surveill. 5:49–50. 2000.
Article23. Watanabe M, Sakai D, Matsuyama D, Yamamoto Y, Sato M, Mochida J. Risk factors for surgical site infection following spine surgery: efficacy of intraoperative saline irrigation. J Neurosurg Spine. 12:540–546. 2010.
Article24. Wimmer C, Gluch H, Franzreb M, Ogon M. Predisposing factors for infection in spine surgery: a survey of 850 spinal procedures. J Spinal Disord. 11:124–128. 1998.25. Wu PC, Kuo HK, Li M, Lai IC, Fang PC, Lin SA, et al. Nosocomial postoperative endophthalmitis: a 14-year review. Graefes Arch Clin Exp Ophthalmol. 244:920–929. 2006.
Article26. Ziebuhr W, Hennig S, Eckart M, Kränzler H, Batzilla C, Kozitskaya S. Nosocomial infections by Staphylococcus epidermidis: how a commensal bacterium turns into a pathogen. Int J Antimicrob Agents 28 Suppl. 1:S14–S20. 2006.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Perspective of Nationwide Surveillance System for Surgical Site Infections
- Prospective Multicenter Surveillance Study of Surgical Site Infection after Intracranial Procedures in Korea : A Preliminary Study
- Surgical Site Infection Rates according to Patient Risk Index after Cardiovascular Surgery
- A preliminary study for the development of indices and the current state of surgical site infections (SSIs) in Korea: the Korean Surgical Site Infection Surveillance (KOSSIS) program
- Surgical Site Infection