Obstet Gynecol Sci.
2017 Nov;60(6):558-564. 10.5468/ogs.2017.60.6.558.
Prognostic value of preoperative lymphocyte-monocyte ratio in elderly patients with advanced epithelial ovarian cancer
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Pusan National University School of Medicine, and Biomedical Research Institute and Pusan Cancer Center, Pusan National University Hospital, Busan, Korea. ghkim@pusan.ac.kr ldh0707@hanmail.net
- KMID: 2418357
- DOI: http://doi.org/10.5468/ogs.2017.60.6.558
Abstract
OBJECTIVE
To investigate the prognostic significance of preoperative lymphocyte-monocyte ratio (LMR) in elderly patients with advanced epithelial ovarian cancer (EOC) receiving primary cytoreductive surgery and adjuvant platinum-based chemotherapy.
METHODS
A total of 42 elderly patients (≥65 years) diagnosed with EOC who are receiving primary cytoreductive surgery and adjuvant platinum-based chemotherapy from 2009 to 2012 was included. LMR was calculated from complete blood cell count sampled before operation. Receiver operating characteristic (ROC) curves were used to calculate optimal cut-off values for LMR. Prognostic significance with respect to overall survival (OS) and progression-free survival (PFS) were determined using log-rank test and Cox regression analysis.
RESULTS
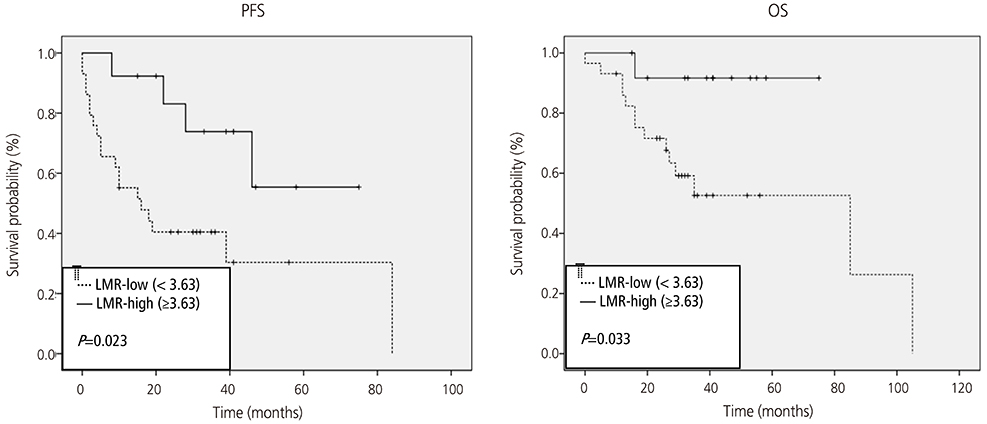
The optimized LMR cut-off value determined by ROC curve analysis was 3.63 for PFS and OS. The high LMR group (LMR ≥3.63) was found to be significantly more associated with optimal debulking (P=0.045) and platinum response (P=0.018) than the low LMR group. In addition, Kaplan-Meier analysis revealed the LMR-high group was significantly more associated with high PFS and OS rates (P=0.023 and P=0.033, respectively), and univariate analysis revealed that a high LMR, histology type, and optimal debulking and platinum responses were significantly associated with prolonged PFS and OS. However, subsequent Cox multivariate analysis showed only optimal debulking and platinum response were independent prognostic factors of PFS or OS.
CONCLUSION
This study suggests that LMR might be associated with treatment and survival outcomes in elderly patients with EOC receiving standard oncology treatment.
MeSH Terms
Figure
Reference
-
1. Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin. 2013; 63:11–30.2. Yancik R. Ovarian cancer. Age contrasts in incidence, histology, disease stage at diagnosis, and mortality. Cancer. 1993; 71:517–523.3. Cloven NG, Manetta A, Berman ML, Kohler MF, DiSaia PJ. Management of ovarian cancer in patients older than 80 years of age. Gynecol Oncol. 1999; 73:137–139.4. Uyar D, Frasure HE, Markman M, von Gruenigen VE. Treatment patterns by decade of life in elderly women (> or =70 years of age) with ovarian cancer. Gynecol Oncol. 2005; 98:403–408.5. Ries LA, Eisner MP, Kosary CL, Hankey BF, Miller BA, Clegg L, et al. SEER cancer statistics review, 1975??001 [Internet]. Bethesda (MD): National Cancer Institute;2014. cited 2017 Mar 1. Available from: http://www.seer.cancer.gov/csr/1975_2001/.6. Wang Y, Liu P, Xu Y, Zhang W, Tong L, Guo Z, et al. Preoperative neutrophil-to-lymphocyte ratio predicts response to first-line platinum-based chemotherapy and prognosis in serous ovarian cancer. Cancer Chemother Pharmacol. 2015; 75:255–262.7. Williams KA, Labidi-Galy SI, Terry KL, Vitonis AF, Welch WR, Goodman A, et al. Prognostic significance and predictors of the neutrophil-to-lymphocyte ratio in ovarian cancer. Gynecol Oncol. 2014; 132:542–550.8. Supoken A, Kleebkaow P, Chumworathayi B, Luanratanakorn S, Kietpeerakool C. Elevated preoperative platelet to lymphocyte ratio associated with decreased survival of women with ovarian clear cell carcinoma. Asian Pac J Cancer Prev. 2014; 15:10831–10836.9. Asher V, Lee J, Innamaa A, Bali A. Preoperative platelet lymphocyte ratio as an independent prognostic marker in ovarian cancer. Clin Transl Oncol. 2011; 13:499–503.10. Jiang R, Cai XY, Yang ZH, Yan Y, Zou X, Guo L, et al. Elevated peripheral blood lymphocyte-to-monocyte ratio predicts a favorable prognosis in the patients with metastatic nasopharyngeal carcinoma. Chin J Cancer. 2015; 34:237–246.11. Ni XJ, Zhang XL, Ou-Yang QW, Qian GW, Wang L, Chen S, et al. An elevated peripheral blood lymphocyte-to-monocyte ratio predicts favorable response and prognosis in locally advanced breast cancer following neoadjuvant chemotherapy. PLoS One. 2014; 9:e111886.12. Hu P, Shen H, Wang G, Zhang P, Liu Q, Du J. Prognostic significance of systemic inflammation-based lymphocyte- monocyte ratio in patients with lung cancer: based on a large cohort study. PLoS One. 2014; 9:e108062.13. Chen L, Zhang F, Sheng XG, Zhang SQ. Decreased pretreatment lymphocyte/monocyte ratio is associated with poor prognosis in stage Ib1-IIa cervical cancer patients who undergo radical surgery. Onco Targets Ther. 2015; 8:1355–1362.14. Winter WE 3rd, Maxwell GL, Tian C, Carlson JW, Ozols RF, Rose PG, et al. Prognostic factors for stage III epithelial ovarian cancer: a Gynecologic Oncology Group Study. J Clin Oncol. 2007; 25:3621–3627.15. Chan JK, Urban R, Cheung MK, Osann K, Shin JY, Husain A, et al. Ovarian cancer in younger vs older women: a population-based analysis. Br J Cancer. 2006; 95:1314–1320.16. Pectasides D, Fountzilas G, Aravantinos G, Bamias A, Kalofonos HP, Skarlos D, et al. Epithelial ovarian carcinoma in younger vs older women: is age an independent prognostic factor? The Hellenic Oncology Cooperative Group experience. Int J Gynecol Cancer. 2007; 17:1003–1010.17. Li YL, Gu KS, Pan YY, Jiao Y, Zhai ZM. Peripheral blood lymphocyte/monocyte ratio at the time of first relapse predicts outcome for patients with relapsed or primary refractory diffuse large B-cell lymphoma. BMC Cancer. 2014; 14:341.18. Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008; 454:436–444.19. Qi Q, Geng Y, Sun M, Wang P, Chen Z. Clinical implications of systemic inflammatory response markers as independent prognostic factors for advanced pancreatic cancer. Pancreatology. 2015; 15:145–150.20. Eo WK, Chang HJ, Kwon SH, Koh SB, Kim YO, Ji YI, et al. The lymphocyte-monocyte ratio predicts patient survival and aggressiveness of ovarian cancer. J Cancer. 2016; 7:289–296.21. Trillsch F, Woelber L, Eulenburg C, Braicu I, Lambrechts S, Chekerov R, et al. Treatment reality in elderly patients with advanced ovarian cancer: a prospective analysis of the OVCAD consortium. J Ovarian Res. 2013; 6:42.22. Alphs HH, Zahurak ML, Bristow RE, Díaz-Montes TP. Predictors of surgical outcome and survival among elderly women diagnosed with ovarian and primary peritoneal cancer. Gynecol Oncol. 2006; 103:1048–1053.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Platelet to lymphocyte ratio as a prognostic factor for epithelial ovarian cancer
- The Prognostic Significance of Serum CA 125 Levels in Patients with Advanced Serous Epithelial Ovarian Cancer
- The relationship between serum p53 autoantibodies and prognostic relevance of epithelial ovarian cancer
- Pretreatment neutrophil-to-lymphocyte ratio and its dynamic change during neoadjuvant chemotherapy as poor prognostic factors in advanced ovarian cancer
- Potential predictors for chemotherapeutic response and prognosis in epithelial ovarian, fallopian tube and primary peritoneal cancer patients treated with platinum-based chemotherapy