Obstet Gynecol Sci.
2020 Jan;63(1):55-63. 10.5468/ogs.2020.63.1.55.
Potential predictors for chemotherapeutic response and prognosis in epithelial ovarian, fallopian tube and primary peritoneal cancer patients treated with platinum-based chemotherapy
- Affiliations
-
- 1Division of Gynecologic Oncology, Department of Obstetrics and Gynecology, Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand. psuprase@gmail.com
- KMID: 2467932
- DOI: http://doi.org/10.5468/ogs.2020.63.1.55
Abstract
OBJECTIVE
This study aimed to investigate the potential predictive factors for platinum resistance and poor prognosis in epithelial ovarian, fallopian tube, and primary peritoneal cancer treated with platinum-based chemotherapy.
METHODS
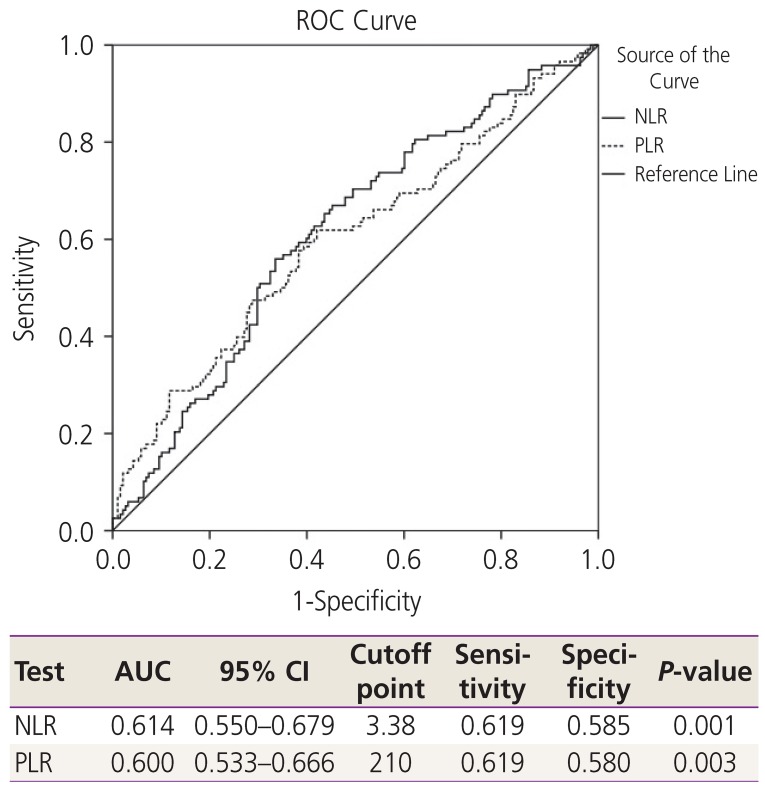
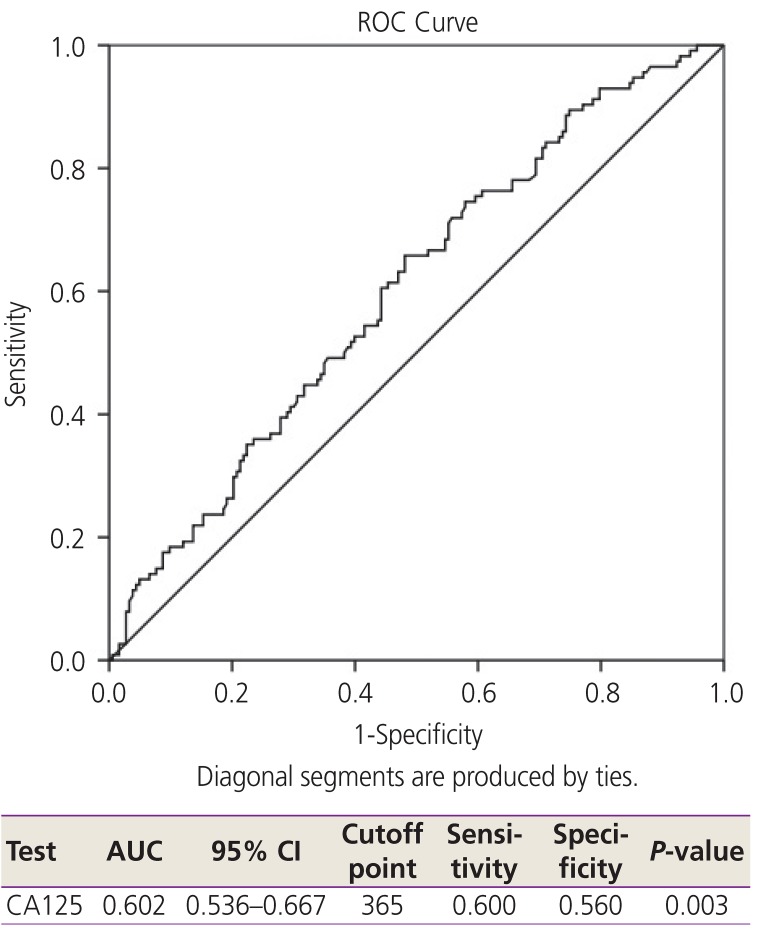
Medical records of 306 patients with the above mentioned cancers treated with platinum-based chemotherapy between 2007 and 2017 were retrospective reviewed. Clinical data, preoperative neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), platinum-free interval, and survival time were recorded. NLR, PLR, and cancer antigen 125 (CA125) levels were calculated for an optimal cutoff point using receiver operating characteristic curves. The clinicopathological variables were compared using univariate and multivariate analyses to identify independent predictive factors for platinum resistance and poor survival outcomes.
RESULTS
The optimal cutoff points for NLR, PLR, and CA125 were 3.38, 210, and 365 IU/L, respectively. Univariate analysis indicated that NLR >3.38, PLR >210, CA125 >365, advanced stage, suboptimal disease, serous type, and ascites were significant predictive factors for platinum resistance. However, only NLR >3.38 and advanced stage were independent predictive factors with an adjusted odds ratio of 1.880 and 3.333, respectively. Regarding factors associated with poor survival outcomes, only PLR >210 and advanced stage were independent factors, with a hazard ratio of 1.578 and 3.994, respectively.
CONCLUSION
High NLR and advanced stage were potential independent predictive factors for platinum resistance, whereas high PLR and advanced stage were potential independent predictive factors for poor survival outcomes.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Recent development of nanotechnology-based approaches for gynecologic cancer therapy
Gangaraju Gedda, Yoo-Jin Park, Myung-Geol Pang
Obstet Gynecol Sci. 2025;68(1):18-29. doi: 10.5468/ogs.24180.
Reference
-
1. International Agency for Research on Cancer. Estimated number of new cases in 2018, worldwide, females [Internet]. Lyon: International Agency for Research on Cancer;2018. cited 2019 Aug 1. Available from: http://gco.iarc.fr/today/online-analysis-table?v=2018&mode=cancer&mode_population=continents&population=900&populations=900&key=asr&sex=2&cancer=39&type=0&statistic=5&prevalence=0&population_group=0&ages_group%5B%5D=10&ages_group%5B%5D=15&nb_items=5&group_cancer=1&include_nmsc=1&include_nmsc_other=1.2. Jayson GC, Kohn EC, Kitchener HC, Ledermann JA. Ovarian cancer. Lancet. 2014; 384:1376–1388. PMID: 24767708.
Article3. Pignata S, C Cecere S, Du Bois A, Harter P, Heitz F. Treatment of recurrent ovarian cancer. Ann Oncol. 2017; 28:viii51–6. PMID: 29232464.
Article4. Ocana A, Nieto-Jiménez C, Pandiella A, Templeton AJ. Neutrophils in cancer: prognostic role and therapeutic strategies. Mol Cancer. 2017; 16:137–144. PMID: 28810877.
Article5. Badora-Rybicka A, Nowara E, Starzyczny-Słota D. Neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio before chemotherapy as potential prognostic factors in patients with newly diagnosed epithelial ovarian cancer. ESMO Open. 2016; 1:e000039. PMID: 27843595.
Article6. Miao Y, Li S, Yan Q, Li B, Feng Y. Prognostic significance of preoperative prognostic nutritional index in epithelial ovarian cancer patients treated with platinum-based chemotherapy. Oncol Res Treat. 2016; 39:712–719. PMID: 27855385.
Article7. Jansaka N, Suprasert P. Survival outcomes of recurrent epithelial ovarian cancer: experience from a Thailand northern tertiary care center. Asian Pac J Cancer Prev. 2014; 15:10837–10840. PMID: 25605186.
Article8. Moses K, Brandau S. Human neutrophils: their role in cancer and relation to myeloid-derived suppressor cells. Semin Immunol. 2016; 28:187–196. PMID: 27067179.
Article9. Miao Y, Yan Q, Li S, Li B, Feng Y. Neutrophil to lymphocyte ratio and platelet to lymphocyte ratio are predictive of chemotherapeutic response and prognosis in epithelial ovarian cancer patients treated with platinum-based chemotherapy. Cancer Biomark. 2016; 17:33–40. PMID: 27314290.
Article10. Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell. 2010; 140:883–899. PMID: 20303878.
Article11. Tian C, Song W, Tian X, Sun Y. Prognostic significance of platelet-to-lymphocyte ratio in patients with ovarian cancer: a meta-analysis. Eur J Clin Invest. 2018; 48:e12917. PMID: 29469190.
Article12. Huang QT, Zhou L, Zeng WJ, Ma QQ, Wang W, Zhong M, et al. Prognostic significance of neutrophil-to-lymphocyte ratio in ovarian cancer: a systematic review and meta-analysis of observational studies. Cell Physiol Biochem. 2017; 41:2411–2418. PMID: 28467978.
Article13. National Comprehensive Cancer Network (US). NCCN clinical practice guidelines in oncology. Fort Washington (PA): National Comprehensive Cancer Network;2019. cited 2019 Aug 1. Available from: https://www.nccn.org/professionals/physician_gls/pdf/ovarian.pdf.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two Cases of Primary Carcinoma of the Fallopian Tube
- A Case of Primary Malignant Mixed M llerian Tumor of the Fallopian Tube
- The 2020 Japan Society of Gynecologic Oncology guidelines for the treatment of ovarian cancer, fallopian tube cancer, and primary peritoneal cancer
- A Case of Primary Carcinoma of the Fallopian Tube
- The role of topotecan as second-line chemotherapy in patients with recurrent epithelial ovarian cancer