J Clin Neurol.
2018 Apr;14(2):225-233. 10.3988/jcn.2018.14.2.225.
An 8-Week Low-Intensity Progressive Cycling Training Improves Motor Functions in Patients with Early-Stage Parkinson's Disease
- Affiliations
-
- 1Division of Movement Disorders, Department of Neurology, Chang Gung Memorial Hospital, Linkou, Taiwan.
- 2School of Physical Therapy and Graduate Institute of Rehabilitation Science, College of Medicine, Chang Gung University, Taoyuan City, Taiwan. yjchang@mail.cgu.edu.tw
- 3Neuroscience Research Center, Chang Gung Memorial Hospital, Linkou, Taiwan.
- 4Health Aging Research Center, Chang Gung University, Taoyuan City, Taiwan.
- KMID: 2407951
- DOI: http://doi.org/10.3988/jcn.2018.14.2.225
Abstract
- BACKGROUND AND PURPOSE
The effects of high-intensity cycling as an adjuvant therapy for early-stage Parkinson's disease (PD) were highlighted recently. However, patients experience difficulties in maintaining these cycling training programs. The present study investigated the efficacy of cycling at a mild-to-moderate intensity in early-stage PD.
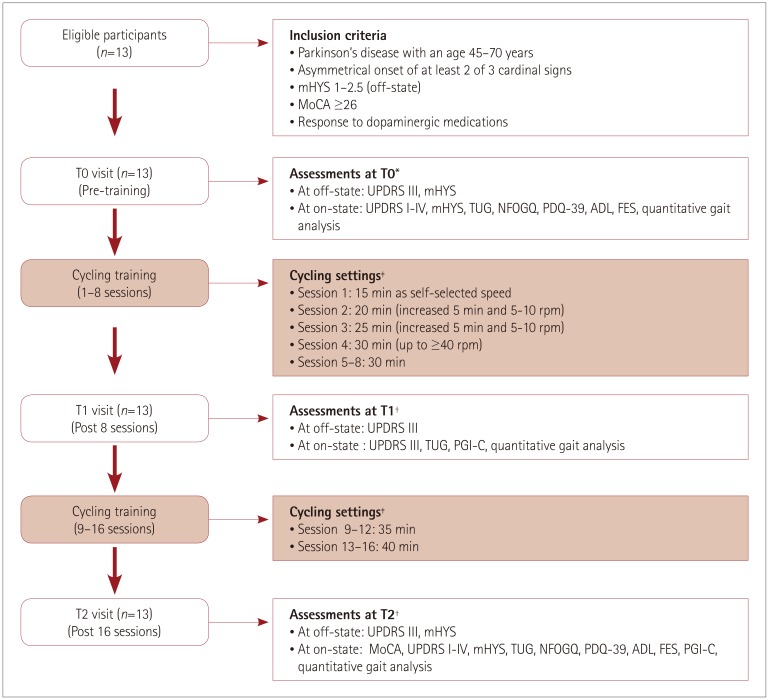
METHODS
Thirteen PD patients were enrolled for 16 serial cycling sessions over a 2-month period. Motor function was assessed using the Unified Parkinson's Disease Rating Scale part III (UPDRS III) and Timed Up and Go (TUG) test as primary outcomes. The Montreal Cognitive Assessment (MoCA), modified Hoehn and Yahr Stage (mHYS), total UPDRS, Falls Efficacy Scale, New Freezing of Gait Questionnaire, Schwab and England Activities of Daily Living, 39-item Parkinson's Disease Questionnaire, Patient Global Impression of Change, and gait performance were assessed as secondary outcomes.
RESULTS
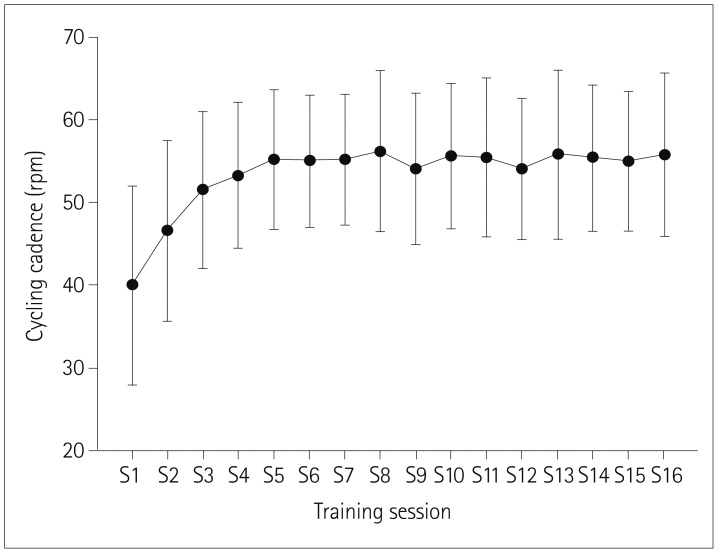
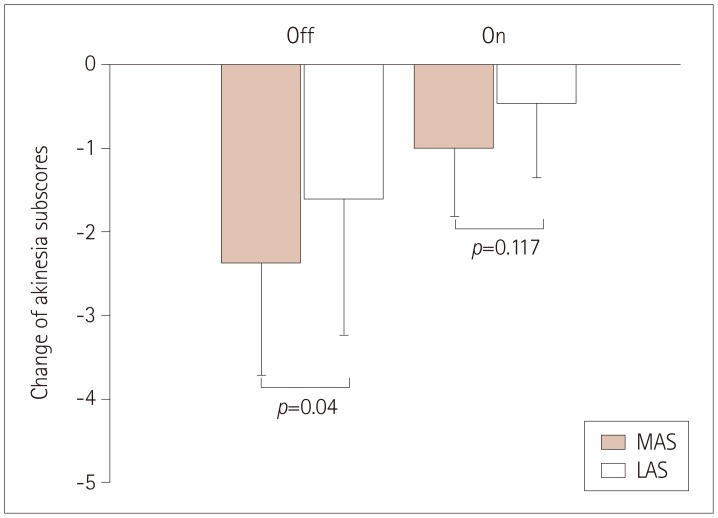
The age and the age at onset were 59.67±7.24 and 53.23±10.26 years (mean±SD), respectively. The cycling cadence was 53.27±8.92 revolutions per minute. The UPDRS III score improved significantly after 8 training sessions (p=0.011) and 16 training sessions (T2) (p=0.001) in the off-state, and at T2 (p=0.004) in the on-state compared to pretraining (T0). The TUG duration was significantly shorter at T2 than at T0 (p < 0.05). The findings of MoCA, total UPDRS, double limb support time, and mHYS (in both the off- and on-states) also improved significantly at T2.
CONCLUSIONS
Our pioneer study has demonstrated that a low-intensity progressive cycling exercise can improve motor function in PD, especially akinesia. The beneficial effects were similar to those of high-intensity rehabilitation programs.
Keyword
MeSH Terms
Figure
Reference
-
1. Wu T, Hallett M, Chan P. Motor automaticity in Parkinson's disease. Neurobiol Dis. 2015; 82:226–234. PMID: 26102020.
Article2. Marsden CD. The mysterious motor function of the basal ganglia: the Robert Wartenberg Lecture. Neurology. 1982; 32:514–539. PMID: 7200209.
Article3. Paillard T, Rolland Y, de Souto Barreto P. Protective effects of physical exercise in Alzheimer's disease and Parkinson's disease: a narrative review. J Clin Neurol. 2015; 11:212–219. PMID: 26174783.
Article4. Goldman JG, Weintraub D. Advances in the treatment of cognitive impairment in Parkinson's disease. Mov Disord. 2015; 30:1471–1489. PMID: 26297863.
Article5. Monteiro-Junior RS, Cevada T, Oliveira BR, Lattari E, Portugal EM, Carvalho A, et al. We need to move more: neurobiological hypotheses of physical exercise as a treatment for Parkinson's disease. Med Hypotheses. 2015; 85:537–541. PMID: 26209418.
Article6. Archer T, Fredriksson A, Johansson B. Exercise alleviates Parkinsonism: clinical and laboratory evidence. Acta Neurol Scand. 2011; 123:73–84. PMID: 21108623.
Article7. Foley TE, Fleshner M. Neuroplasticity of dopamine circuits after exercise: implications for central fatigue. Neuromolecular Med. 2008; 10:67–80. PMID: 18274707.
Article8. da Silva PG, Domingues DD, de Carvalho LA, Allodi S, Correa CL. Neurotrophic factors in Parkinson's disease are regulated by exercise: evidence-based practice. J Neurol Sci. 2016; 363:5–15. PMID: 27000212.
Article9. Rasmussen P, Brassard P, Adser H, Pedersen MV, Leick L, Hart E, et al. Evidence for a release of brain-derived neurotrophic factor from the brain during exercise. Exp Physiol. 2009; 94:1062–1069. PMID: 19666694.
Article10. Radak Z, Chung HY, Goto S. Exercise and hormesis: oxidative stress-related adaptation for successful aging. Biogerontology. 2005; 6:71–75. PMID: 15834665.
Article11. Bloomer RJ. Effect of exercise on oxidative stress biomarkers. Adv Clin Chem. 2008; 46:1–50. PMID: 19004186.12. Ridgel AL, Vitek JL, Alberts JL. Forced, not voluntary, exercise improves motor function in Parkinson's disease patients. Neurorehabil Neural Repair. 2009; 23:600–608. PMID: 19131578.
Article13. Alberts JL, Linder SM, Penko AL, Lowe MJ, Phillips M. It is not about the bike, it is about the pedaling: forced exercise and Parkinson's disease. Exerc Sport Sci Rev. 2011; 39:177–186. PMID: 21799425.14. Zoladz JA, Majerczak J, Zeligowska E, Mencel J, Jaskolski A, Jaskolska A, et al. Moderate-intensity interval training increases serum brain-derived neurotrophic factor level and decreases inflammation in Parkinson's disease patients. J Physiol Pharmacol. 2014; 65:441–448. PMID: 24930517.15. Ridgel AL, Phillips RS, Walter BL, Discenzo FM, Loparo KA. Dynamic high-cadence cycling improves motor symptoms in Parkinson's disease. Front Neurol. 2015; 6:194. PMID: 26388836.
Article16. Ridgel AL, Peacock CA, Fickes EJ, Kim CH. Active-assisted cycling improves tremor and bradykinesia in Parkinson's disease. Arch Phys Med Rehabil. 2012; 93:2049–2054. PMID: 22659536.
Article17. McGough EL, Robinson CA, Nelson MD, Houle R, Fraser G, Handley L, et al. A tandem cycling program: feasibility and physical performance outcomes in people with Parkinson disease. J Neurol Phys Ther. 2016; 40:223–229. PMID: 27576091.
Article18. Nadeau A, Lungu O, Duchesne C, Robillard MÈ, Bore A, Bobeuf F, et al. A 12-week cycling training regimen improves gait and executive functions concomitantly in people with Parkinson's disease. Front Hum Neurosci. 2017; 10:690. PMID: 28127282.
Article19. Duchesne C, Lungu O, Nadeau A, Robillard ME, Boré A, Bobeuf F, et al. Enhancing both motor and cognitive functioning in Parkinson's disease: aerobic exercise as a rehabilitative intervention. Brain Cogn. 2015; 99:68–77. PMID: 26263381.
Article20. Shulman LM, Katzel LI, Ivey FM, Sorkin JD, Favors K, Anderson KE, et al. Randomized clinical trial of 3 types of physical exercise for patients with Parkinson disease. JAMA Neurol. 2013; 70:183–190. PMID: 23128427.
Article21. Lauhoff P, Murphy N, Doherty C, Horgan NF. A controlled clinical trial investigating the effects of cycle ergometry training on exercise tolerance, balance and quality of life in patients with Parkinson's disease. Disabil Rehabil. 2013; 35:382–387. PMID: 22747197.
Article22. Nieman DC, Miller AR, Henson DA, Warren BJ, Gusewitch G, Johnson RL, et al. Effect of high-versus moderate-intensity exercise on lymphocyte subpopulations and proliferative response. Int J Sports Med. 1994; 15:199–206. PMID: 8063469.23. Pedersen BK, Bruunsgaard H. How physical exercise influences the establishment of infections. Sports Med. 1995; 19:393–400. PMID: 7676100.
Article24. Pyne DB. Regulation of neutrophil function during exercise. Sports Med. 1994; 17:245–258. PMID: 8009138.
Article25. Ronsen O, Pedersen BK, Øritsland TR, Bahr R, Kjeldsen-Kragh J. Leukocyte counts and lymphocyte responsiveness associated with repeated bouts of strenuous endurance exercise. J Appl Physiol. 2001; 91:425–434. PMID: 11408460.
Article26. da Silva DJ, Borges AF, Souza PO, de Souza PR, Cardoso CR, Dorta ML, et al. Decreased toll-like receptor 2 and toll-like receptor 7/8-induced cytokines in Parkinson's disease patients. Neuroimmunomodulation. 2016; 23:58–66. PMID: 26886382.
Article27. Ramaker C, Marinus J, Stiggelbout AM, Van Hilten BJ. Systematic evaluation of rating scales for impairment and disability in Parkinson's disease. Mov Disord. 2002; 17:867–876. PMID: 12360535.
Article28. Morris S, Morris ME, Iansek R. Reliability of measurements obtained with the timed “Up & Go” test in people with Parkinson disease. Phys Ther. 2001; 81:810–818. PMID: 11175678.29. Gelb DJ, Oliver E, Gilman S. Diagnostic criteria for Parkinson disease. Arch Neurol. 1999; 56:33–39. PMID: 9923759.
Article30. Goetz CG, Poewe W, Rascol O, Sampaio C, Stebbins GT, Counsell C, et al. Movement Disorder Society Task Force report on the Hoehn and Yahr staging scale: status and recommendations. Mov Disord. 2004; 19:1020–1028. PMID: 15372591.31. Zadikoff C, Fox SH, Tang-Wai DF, Thomsen T, de Bie RM, Wadia P, et al. A comparison of the mini mental state exam to the Montreal cognitive assessment in identifying cognitive deficits in Parkinson's disease. Mov Disord. 2008; 23:297–299. PMID: 18044697.
Article32. Martínez-Martín P, Gil-Nagel A, Gracia LM, Gómez JB, Martínez-Sarriés J, Bermejo F. Unified Parkinson's disease rating scale characteristics and structure. the cooperative multicentric group. Mov Disord. 1994; 9:76–83. PMID: 8139608.33. Nieuwboer A, Rochester L, Herman T, Vandenberghe W, Emil GE, Thomaes T, et al. Reliability of the new freezing of gait questionnaire: agreement between patients with Parkinson's disease and their carers. Gait Posture. 2009; 30:459–463. PMID: 19660949.
Article34. Peto V, Jenkinson C, Fitzpatrick R. PDQ-39: a review of the development, validation and application of a Parkinson's disease quality of life questionnaire and its associated measures. J Neurol. 1998; 245(Suppl 1):S10–S14. PMID: 9617716.
Article35. Martinez-Martin P, Prieto L, Forjaz MJ. Longitudinal metric properties of disability rating scales for Parkinson's disease. Value Health. 2006; 9:386–393. PMID: 17076869.
Article36. Dewan N, MacDermid JC. Fall efficacy scale-international (FES-I). J Physiother. 2014; 60:60. PMID: 24856947.37. Busner J, Targum SD. The clinical global impressions scale: applying a research tool in clinical practice. Psychiatry (Edgmont). 2007; 4:28–37.38. Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982; 14:377–381. PMID: 7154893.
Article39. Karvonen MJ, Kentala E, Mustala O. The effects of training on heart rate; a longitudinal study. Ann Med Exp Biol Fenn. 1957; 35:307–315. PMID: 13470504.40. Barker S, Craik R, Freedman W, Herrmann N, Hillstrom H. Accuracy, reliability, and validity of a spatiotemporal gait analysis system. Med Eng Phys. 2006; 28:460–467. PMID: 16122966.
Article41. Shulman LM, Gruber-Baldini AL, Anderson KE, Fishman PS, Reich SG, Weiner WJ. The clinically important difference on the unified Parkinson's disease rating scale. Arch Neurol. 2010; 67:64–70. PMID: 20065131.
Article42. Marsden CD. Slowness of movement in Parkinson's disease. Mov Disord. 1989; 4(Suppl 1):S26–S37. PMID: 2657408.
Article43. Hallett M. Bradykinesia: why do Parkinson's patients have it and what trouble does it cause? Mov Disord. 2011; 26:1579–1581. PMID: 21547949.
Article44. Lotze M, Braun C, Birbaumer N, Anders S, Cohen LG. Motor learning elicited by voluntary drive. Brain. 2003; 126:866–872. PMID: 12615644.
Article45. Perez MA, Lungholt BK, Nyborg K, Nielsen JB. Motor skill training induces changes in the excitability of the leg cortical area in healthy humans. Exp Brain Res. 2004; 159:197–205. PMID: 15549279.
Article46. Corcos DM, Chen CM, Quinn NP, McAuley J, Rothwell JC. Strength in Parkinson's disease: relationship to rate of force generation and clinical status. Ann Neurol. 1996; 39:79–88. PMID: 8572671.47. Jenkins IH, Fernandez W, Playford ED, Lees AJ, Frackowiak RS, Passingham RE, et al. Impaired activation of the supplementary motor area in Parkinson's disease is reversed when akinesia is treated with apomorphine. Ann Neurol. 1992; 32:749–757. PMID: 1471865.
Article48. Katz-Leurer M, Sender I, Keren O, Dvir Z. The influence of early cycling training on balance in stroke patients at the subacute stage. Results of a preliminary trial. Clin Rehabil. 2006; 20:398–405. PMID: 16774090.
Article49. Hass CJ, Bishop M, Moscovich M, Stegemöller EL, Skinner J, Malaty IA, et al. Defining the clinically meaningful difference in gait speed in persons with Parkinson disease. J Neurol Phys Ther. 2014; 38:233–238. PMID: 25198866.
Article50. Ahlskog JE. Does vigorous exercise have a neuroprotective effect in Parkinson disease? Neurology. 2011; 77:288–294. PMID: 21768599.
Article51. Zigmond MJ, Cameron JL, Hoffer BJ, Smeyne RJ. Neurorestoration by physical exercise: moving forward. Parkinsonism Relat Disord. 2012; 18(Suppl 1):S147–S150. PMID: 22166417.
Article52. Chen H, Zhang SM, Schwarzschild MA, Hernán MA, Ascherio A. Physical activity and the risk of Parkinson disease. Neurology. 2005; 64:664–669. PMID: 15728289.
Article53. Thacker EL, Chen H, Patel AV, McCullough ML, Calle EE, Thun MJ, et al. Recreational physical activity and risk of Parkinson's disease. Mov Disord. 2008; 23:69–74. PMID: 17960818.
Article54. Xu Q, Park Y, Huang X, Hollenbeck A, Blair A, Schatzkin A, et al. Physical activities and future risk of Parkinson disease. Neurology. 2010; 75:341–348. PMID: 20660864.
Article55. Iansek R, Huxham F, McGinley J. The sequence effect and gait festination in Parkinson disease: contributors to freezing of gait? Mov Disord. 2006; 21:1419–1424. PMID: 16773644.
Article56. Chee R, Murphy A, Danoudis M, Georgiou-Karistianis N, Iansek R. Gait freezing in Parkinson's disease and the stride length sequence effect interaction. Brain. 2009; 132:2151–2160. PMID: 19433440.
Article57. Lacquaniti F, Grasso R, Zago M. Motor patterns in walking. News Physiol Sci. 1999; 14:168–174. PMID: 11390844.
Article58. David FJ, Robichaud JA, Leurgans SE, Poon C, Kohrt WM, Goldman JG, et al. Exercise improves cognition in Parkinson's disease: the PRET-PD randomized, clinical trial. Mov Disord. 2015; 30:1657–1663. PMID: 26148003.
Article59. Gerecke KM, Jiao Y, Pani A, Pagala V, Smeyne RJ. Exercise protects against MPTP-induced neurotoxicity in mice. Brain Res. 2010; 1341:72–83. PMID: 20116369.
Article60. Petzinger GM, Fisher BE, McEwen S, Beeler JA, Walsh JP, Jakowec MW. Exercise-enhanced neuroplasticity targeting motor and cognitive circuitry in Parkinson's disease. Lancet Neurol. 2013; 12:716–726. PMID: 23769598.
Article61. Ridgel AL, Abdar HM, Alberts JL, Discenzo FM, Loparo KA. Variability in cadence during forced cycling predicts motor improvement in individuals with Parkinson's disease. IEEE Trans Neural Syst Rehabil Eng. 2013; 21:481–489. PMID: 23144045.
Article62. Smith PJ, Blumenthal JA, Hoffman BM, Cooper H, Strauman TA, Welsh-Bohmer K, et al. Aerobic exercise and neurocognitive performance: a meta-analytic review of randomized controlled trials. Psychosom Med. 2010; 72:239–252. PMID: 20223924.
Article63. Mirelman A, Maidan I, Herman T, Deutsch JE, Giladi N, Hausdorff JM. Virtual reality for gait training: can it induce motor learning to enhance complex walking and reduce fall risk in patients with Parkinson's disease? J Gerontol A Biol Sci Med Sci. 2011; 66:234–240. PMID: 21106702.
Article64. Ebersbach G, Ebersbach A, Edler D, Kaufhold O, Kusch M, Kupsch A, et al. Comparing exercise in Parkinson's disease--the Berlin LSVT®BIG study. Mov Disord. 2010; 25:1902–1908. PMID: 20669294.65. Okun MS. Management of Parkinson disease in 2017: personalized approaches for patient-specific needs. JAMA. 2017; 318:791–792. PMID: 28828469.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Dance Intervention Using the Feldenkrais Method Improves Motor, and Non-Motor Symptoms and Gait in Parkinson’s Disease: A 12-Month Study
- Biomarker in Parkinson’s Disease: Clinical and Biochemical Biomarker
- Effects of Short-term Repeated Sprint Exercise Training and Moderate Intensity Continuous Exercise Training on Vascular Function in Healthy Young Adults
- Improvement of Cognitive Function after Computer-Based Cognitive Training in Early Stage of Alzheimer's Dementia
- Exercise Therapy for Hypertensive Patients