Korean J Gastroenterol.
2018 Feb;71(2):98-102. 10.4166/kjg.2018.71.2.98.
Pancreatic Neuroendocrine Tumor Presenting as Acute Pancreatitis
- Affiliations
-
- 1Department of Internal Medicine, Kangwon National University School of Medicine, Chuncheon, Korea. youreon.park@gmail.com
- 2Department of Anatomic Pathology, Kangwon National University School of Medicine, Chuncheon, Korea.
- 3Department of Radiology, Kangwon National University School of Medicine, Chuncheon, Korea.
- KMID: 2405003
- DOI: http://doi.org/10.4166/kjg.2018.71.2.98
Abstract
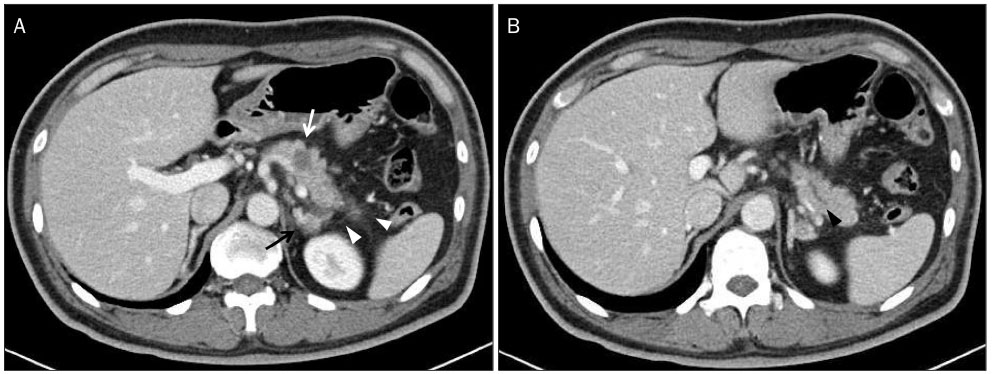
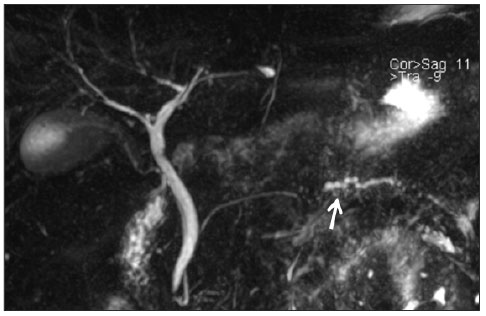
- We report a case of acute pancreatitis secondary to pancreatic neuroendocrine tumor. A 46-year old man presented with upper abdominal pain. The serum amylase and lipase were elevated. Abdominal computed tomography (CT) and magnetic resonance cholangiopancreatography revealed a 1.7 cm sized mass at the pancreas body with a dilatation of the upstream pancreatic duct and mild infiltrations of peripancreatic fat. An endoscopic ultrasound-guided fine needle biopsy was performed for the pancreatic mass, but only necrotic tissue was observed on the pathologic examination. A chest and neck CT scan revealed anterior mediastinal, paratracheal, and cervical lymph node enlargement, which were indicative of metastasis. An ultrasound-guided core needle biopsy was performed for the enlarged neck lymph node, and pathologic examination revealed a metastatic poorly differentiated carcinoma. Immunohistochemical analysis showed positive staining for synaptophysin, chromogranin A, and CD 56, indicative of a neuroendocrine carcinoma.
MeSH Terms
-
Abdominal Pain
Amylases
Biopsy, Fine-Needle
Biopsy, Large-Core Needle
Carcinoma, Neuroendocrine
Cholangiopancreatography, Magnetic Resonance
Chromogranin A
Dilatation
Endoscopic Ultrasound-Guided Fine Needle Aspiration
Lipase
Lymph Nodes
Neck
Neoplasm Metastasis
Neuroendocrine Tumors*
Pancreas
Pancreatic Ducts
Pancreatitis*
Synaptophysin
Thorax
Tomography, X-Ray Computed
Amylases
Chromogranin A
Lipase
Synaptophysin
Figure
Reference
-
1. Jin SY. Recent update of pathology of the pancreatic neuroendocrine tumor. Korean J Med. 2011; 80:371–377.2. Chang HM. Consensus guideline for advanced pancreatic neuroendocrine tumor. Korean J Med. 2011; 80:393–396.3. Kimura W, Kuroda A, Morioka Y. Clinical pathology of endocrine tumors of the pancreas. Analysis of autopsy cases. Dig Dis Sci. 1991; 36:933–942.4. Viúdez A, De Jesus-Acosta A, Carvalho FL, Vera R, Martín-Algarra S, Ramírez N. Pancreatic neuroendocrine tumors: challenges in an underestimated disease. Crit Rev Oncol Hematol. 2016; 101:193–206.
Article5. Tejedor Bravo M, Justo LM, Lasala JP, Moreira Vicente VF, Ruiz AC, Scapa Mde L. Acute pancreatitis secondary to neuroendocrine pancreatic tumors: report of 3 cases and literature review. Pancreas. 2012; 41:485–489.6. Ahn SS, Kim MJ, Kim D. An insidious pancreatic lesion in a young woman with recurrent pancreatitis. Gastroenterology. 2010; 139:e9–e10.
Article7. Maimone S, Agrawal D, Pollack MJ, et al. Variability in measurements of pancreatic cyst size among EUS, CT, and magnetic resonance imaging modalities. Gastrointest Endosc. 2010; 71:945–950.
Article8. Griñó P, Martínez J, Griñó E, et al. Acute pancreatitis secondary to pancreatic neuroendocrine tumours. JOP. 2003; 4:104–110.9. Jang DK, Park JM, Lee M, et al. A Case of Long-term Survivor of Pancreatic Neuroendocrine Tumor with Multiple Liver Metastases. Korean J Pancreas Biliary Tract. 2013; 18:62–66.
Article10. Tsutsumi K, Ohtsuka T, Mori Y, et al. Analysis of lymph node metastasis in pancreatic neuroendocrine tumors (PNETs) based on the tumor size and hormonal production. J Gastroenterol. 2012; 47:678–685.
Article11. Kawamoto S, Shi C, Hruban RH, et al. Small serotonin-producing neuroendocrine tumor of the pancreas associated with pancreatic duct obstruction. AJR Am J Roentgenol. 2011; 197:W482–W488.
Article12. Hamada Y, Nakayama Y, Maeshiro K, Ikeda T, Hayashi H, Iwasaki H. Two cases of primary carcinoid tumor of the pancreas associated with marked stenosis of the main pancreatic duct. Pancreas. 2009; 38:834–835.
Article13. Dhir V, Joshi N, Vivekanandarajah S, Bhandari S, Bapat M, Maydeo A. Recurrent acute pancreatitis in a patient with wirsungocele and neuroendocrine tumor of ampulla of Vater. JOP. 2013; 14:99–101.14. Oh TG, Bang S. Pathogenesis of acute pancreatitis. Korean J Med. 2013; 85:111–115.
Article15. Pavel ME, Hassler G, Baum U, Hahn EG, Lohmann T, Schuppan D. Circulating levels of angiogenic cytokines can predict tumour progression and prognosis in neuroendocrine carcinomas. Clin Endocrinol (Oxf). 2005; 62:434–443.
Article16. Blogowski W, Deskur A, Budkowska M, et al. Selected cytokines in patients with pancreatic cancer: a preliminary report. PLoS One. 2014; 9:e97613.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Experimental Animal Models of Pancreatic Diseases
- A Case of Congenital Anomaly of the Pancreatic Duct Discovered in a Child with Recurrent Acute Pancreatitis
- Robotic enucleation of a pancreatic uncinate neuroendocrine tumor – a unique parenchyma-saving strategy for uncinate tumors
- A Case of Pancreatic Pseudocyst Presenting as Duodenal Bleeding
- Mucinous Cystic Neoplasm of the Pancreas Presenting with Acute Pancreatitis, Initially Misdiagnosed as a Pseudocyst