Asia Pac Allergy.
2014 Oct;4(4):241-252. 10.5415/apallergy.2014.4.4.241.
House dust mite allergy: environment evaluation and disease prevention
- Affiliations
-
- 1Institute of Biomedical Sciences, National Chung Hsing University, Taichung 40705, Taiwan. jawji@vghtc.gov.tw
- 2Section of Immunology and Rheumatology, Department of Internal Medicine, Taichung Veterans General Hospital, Taichung 40705, Taiwan.
- 3Center for Translational Medicine, Department of Medical Research, Taichung Veterans General Hospital, Taichung 40705, Taiwan.
- 4Department of BioIndustry Technology, Da Yeh University, Changhua 51591, Taiwan.
- 5Department of Medical Technology, Jen Ten College of Medicine, Nursing and Management, Miaoli 35664, Taiwan.
- 6Institute of Clinical Medicine, National Yang Ming University, Taipei 11221, Taiwan.
- KMID: 2397105
- DOI: http://doi.org/10.5415/apallergy.2014.4.4.241
Abstract
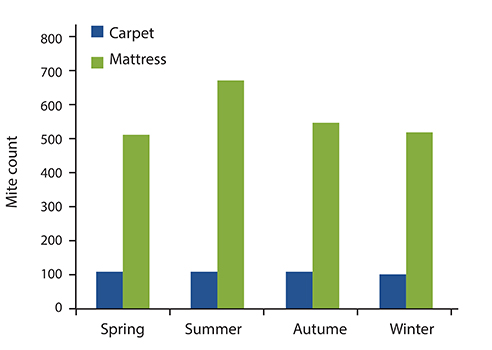
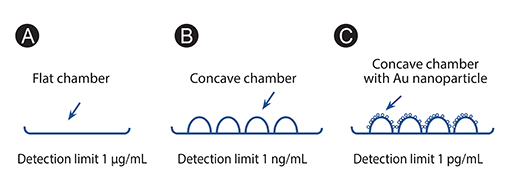
- There are two groups of dust mites, house dust mites (HDMs) and storage mites (SMs), that have been identified in the household environment. Both could induce airway inflammation through activation of innate and adaptive immunity and lead to asthma. In order to monitor environmental dust mite infestation, different methods can be used to detect their presence, such as the use of floating methods, monoclonal antibodies, and nanostructured biosensor. SM could be identified in the storage room, mainly in contaminated food such as mushrooms and corn starch. In HDM-sensitive subjects and mice that were challenged with HDM or SM after sensitization, these mites could up-regulate IgE levels, T helper 2 associated cytokine production and airway hypersensitivity. Different age groups of subjects were sensitized by different species of mites. More subjects above 70 years were sensitized by SM and more subjects below the age of 40 years were sensitized to HDM. Different allergenic components of dust mite extracts, such as Der p 1, Der p 2, could activate innate immunity through activating pattern recognition receptor (PRR) and then lead to allergic inflammation. The best modality to treat HDM allergy is immunomodulation through Treg cells and IgA production. In the recent years, many studies indicated probiotics could increase IgA secretion and the number of Treg cells. However, some studies conducted in adults have contradictory effects in reducing allergic symptoms. Therefore, probiotics confer inconclusive benefits on the allergic symptoms.
MeSH Terms
-
Acaridae
Adaptive Immunity
Adult
Agaricales
Animals
Antibodies, Monoclonal
Asthma
Biosensing Techniques
Dust*
Family Characteristics
Humans
Hypersensitivity
Immunity, Innate
Immunoglobulin A
Immunoglobulin E
Immunomodulation
Inflammation
Mice
Mite Infestations
Mites
Probiotics
Pyroglyphidae*
Rhinitis, Allergic
Starch
T-Lymphocytes, Regulatory
Zea mays
Antibodies, Monoclonal
Dust
Immunoglobulin A
Immunoglobulin E
Starch
Figure
Cited by 2 articles
-
In the memory of Professor Felicidad Cua-Lim
Yoon-Seok Chang
Asia Pac Allergy. 2014;4(4):185-186. doi: 10.5415/apallergy.2014.4.4.185.Acute and chronic exposure to Tyrophagus putrescentiae induces allergic pulmonary response in a murine model
Nailê Karine Nuñez, Aline Andrea da Cunha, Moisés dos Santos Dutra, Gustavo Leivas Barbosa, Alessandra Loureiro Morassutti, Rodrigo Godinho de Souza, Mauro Henrique Moraes Vargas, Géssica Luana Antunes, Josiane Silva Silveira, Guilherme Liberato da Silva, Paulo Márcio Pitrez
Asia Pac Allergy. 2016;6(1):48-55. doi: 10.5415/apallergy.2016.6.1.48.
Reference
-
1. Arlian LG, Morgan MS. Biology, ecology, and prevalence of dust mites. Immunol Allergy Clin North Am. 2003; 23:443–468.
Article2. Fernandez-Caldas E, Iraola V, Carnes J. Molecular and biochemical properties of storage mites (except Blomia species). Protein Pept Lett. 2007; 14:954–959.
Article3. Thomas WR, Smith WA, Hales BJ. The allergenic specificities of the house dust mite. Chang Gung Med J. 2004; 27:563–569.4. Tsai JJ, Wu HH, Shen HD, Hsu EL, Wang SR. Sensitization to Blomia tropicalis among asthmatic patients in Taiwan. Int Arch Allergy Immunol. 1998; 115:144–149.
Article5. Tsai JJ, Yi FC, Chua KY, Liu YH, Lee BW, Cheong N. Identification of the major allergenic components in Blomia tropicalis and the relevance of the specific IgE in asthmatic patients. Ann Allergy Asthma Immunol. 2003; 91:485–489.
Article6. Tsai JJ, Shen HD, Chua KY. Purification of group 2 Dermatophagoides pteronyssinus allergen and prevalence of its specific IgE in asthmatics. Int Arch Allergy Immunol. 2000; 121:205–210.7. Liao EC, Lin YH, Tsai JJ. Detection of group 2 Dermatophagoides pteronyssinus allergen for environmental monitoring of dust mite infestation. Biosci Trends. 2013; 7:82–88.
Article8. Tsai JJ, Bau IJ, Chen HT, Lin YT, Wang GJ. A novel nanostructured biosensor for the detection of the dust mite antigen Der p2. Int J Nanomedicine. 2011; 6:1201–1208.9. Lambrecht BN. Dendritic cells and the regulation of the allergic immune response. Allergy. 2005; 60:271–282.
Article10. Novak N, Haberstok J, Geiger E, Bieber T. Dendritic cells in allergy. Allergy. 1999; 54:792–803.
Article11. Vermaelen KY, Carro-Muino I, Lambrecht BN, Pauwels RA. Specific migratory dendritic cells rapidly transport antigen from the airways to the thoracic lymph nodes. J Exp Med. 2001; 193:51–60.
Article12. Lambrecht BN, Hammad H. The role of dendritic and epithelial cells as master regulators of allergic airway inflammation. Lancet. 2010; 376:835–843.
Article13. Tsai JJ, Ho CY, Wang SR. Relationship between nasal resistance and airway hyperreactivity following nasal provocation with Dermatophagoides pteronyssinus in allergic rhinitis. Int Arch Allergy Immunol. 1995; 106:286–290.14. Johnson JR, Wiley RE, Fattouh R, Swirski FK, Gajewska BU, Coyle AJ, Gutierrez-Ramos JC, Ellis R, Inman MD, Jordana M. Continuous exposure to house dust mite elicits chronic airway inflammation and structural remodeling. Am J Respir Crit Care Med. 2004; 169:378–385.
Article15. Tomlinson KL, Davies GC, Sutton DJ, Palframan RT. Neutralisation of interleukin-13 in mice prevents airway pathology caused by chronic exposure to house dust mite. PLoS One. 2010; 5:e13136.
Article16. Barnes PJ. Pathophysiology of allergic inflammation. Immunol Rev. 2011; 242:31–50.
Article17. Sánchez-Machín I, Glez-Paloma Poza R, Iglesias-Souto J, Iraola V, Matheu V. Oral mite anaphylaxis. Allergy. 2010; 65:1345–1347.
Article18. Arlian LG, Geis DP, Vyszenski-Moher DL, Bernstein IL, Gallagher JS. Antigenic and allergenic properties of the storage mite Tyrophagus putrescentiae. J Allergy Clin Immunol. 1984; 74:166–171.
Article19. Arlian LG, Vyszenski-Moher DL, Johansson SG, van Hage-Hamsten M. Allergenic characterization of Tyrophagus putrescentiae using sera from occupationally exposed farmers. Ann Allergy Asthma Immunol. 1997; 79:525–529.
Article20. van Hage-Hamsten M, Johansson E. Clinical and immunologic aspects of storage mite allergy. Allergy. 1998; 53:48 Suppl. 49–53.21. Thomas WR, Hales BJ, Smith WA. House dust mite allergens in asthma and allergy. Trends Mol Med. 2010; 16:321–328.
Article22. Henszel L, Kuzna-Grygiel W. House dust mites in the etiology of allergic diseases. Ann Acad Med Stetin. 2006; 52:123–127.23. Liao EC, Ho CM, Yin SC, Tsai JJ. Immune responses to tyrophagus putrescentiae-induced airway inflammation in mice. J Investig Allergol Clin Immunol. 2013; 23:20–29.24. Chang YC, Hsieh KH. The study of house dust mites in Taiwan. Ann Allergy. 1989; 62:101–106.25. Kam KL, Hsieh KH. Comparison of three in vitro assays for serum IgE with skin testing in asthmatic children. Ann Allergy. 1994; 73:329–336.26. Liao EC, Hsu EL, Tsai JJ, Ho CM. Immunologic characterization and allergenicity of recombinant Tyr p 3 allergen from the storage mite Tyrophagus putrescentiae. Int Arch Allergy Immunol. 2009; 150:15–24.27. Vidal C, Boquete O, Gude F, Rey J, Meijide LM, Fernandez-Merino MC, González-Quintela A. High prevalence of storage mite sensitization in a general adult population. Allergy. 2004; 59:401–405.
Article28. Munhbayarlah S, Park JW, Ko SH, Ree HI, Hong CS. Identification of Tyrophagus putrescentiae allergens and evaluation of cross-reactivity with Dermatophagoides pteronyssinus. Yonsei Med J. 1998; 39:109–115.29. Liao EC, Ho CM, Tsai JJ. Prevalence of Tyrophagus putrescentiae hypersensitivity in subjects over 70 years of age in a veterans' nursing home in Taiwan. Int Arch Allergy Immunol. 2010; 152:368–377.30. Tsai JJ, Liao EC, Hsu JY, Lee WJ, Lai YK. The differences of eosinophil- and neutrophil-related inflammation in elderly allergic and non-allergic chronic obstructive pulmonary disease. J Asthma. 2010; 47:1040–1044.
Article31. Cho HJ, Lee HJ, Kim SC, Kim K, Kim YS, Kim CH, Lee JG, Yoon JH, Choi JY. Protease-activated receptor 2-dependent fluid secretion from airway submucosal glands by house dust mite extract. J Allergy Clin Immunol. 2012; 129:529–535. 535.e1–535.e5.
Article32. Asokananthan N, Graham PT, Fink J, Knight DA, Bakker AJ, McWilliam AS, Thompson PJ, Stewart GA. Activation of protease-activated receptor (PAR)-1, PAR-2, and PAR-4 stimulates IL-6, IL-8, and prostaglandin E2 release from human respiratory epithelial cells. J Immunol. 2002; 168:3577–3585.33. Asokananthan N, Graham PT, Stewart DJ, Bakker AJ, Eidne KA, Thompson PJ, Stewart GA. House dust mite allergens induce proinflammatory cytokines from respiratory epithelial cells: the cysteine protease allergen, Der p 1, activates protease-activated receptor (PAR)-2 and inactivates PAR-1. J Immunol. 2002; 169:4572–4578.
Article34. Trombone AP, Tobias KR, Ferriani VP, Schuurman J, Aalberse RC, Smith AM, Chapman MD, Arruda LK. Use of a chimeric ELISA to investigate immunoglobulin E antibody responses to Der p 1 and Der p 2 in mite-allergic patients with asthma, wheezing and/or rhinitis. Clin Exp Allergy. 2002; 32:1323–1328.35. Abreu MT, Arditi M. Innate immunity and toll-like receptors: clinical implications of basic science research. J Pediatr. 2004; 144:421–429.
Article36. Tsai JJ, Liu SH, Yin SC, Yang CN, Hsu HS, Chen WB, Liao EC, Lee WJ, Pan HC, Sheu ML. Mite allergen Der-p2 triggers human B lymphocyte activation and Toll-like receptor-4 induction. PLoS One. 2011; 6:e23249.37. D'Andrea MR, Derian CK, Leturcq D, Baker SM, Brunmark A, Ling P, Darrow AL, Santulli RJ, Brass LF, Andrade-Gordon P. Characterization of protease-activated receptor-2 immunoreactivity in normal human tissues. J Histochem Cytochem. 1998; 46:157–164.38. Brown JR, Kleimberg J, Marini M, Sun G, Bellini A, Mattoli S. Kinetics of eotaxin expression and its relationship to eosinophil accumulation and activation in bronchial biopsies and bronchoalveolar lavage (BAL) of asthmatic patients after allergen inhalation. Clin Exp Immunol. 1998; 114:137–146.
Article39. Ackerman V, Marini M, Vittori E, Bellini A, Vassali G, Mattoli S. Detection of cytokines and their cell sources in bronchial biopsy specimens from asthmatic patients. Relationship to atopic status, symptoms, and level of airway hyperresponsiveness. Chest. 1994; 105:687–696.40. Ying S, Robinson DS, Meng Q, Rottman J, Kennedy R, Ringler DJ, Mackay CR, Daugherty BL, Springer MS, Durham SR, Williams TJ, Kay AB. Enhanced expression of eotaxin and CCR3 mRNA and protein in atopic asthma. Association with airway hyperresponsiveness and predominant co-localization of eotaxin mRNA to bronchial epithelial and endothelial cells. Eur J Immunol. 1997; 27:3507–3516.
Article41. Soloperto M, Mattoso VL, Fasoli A, Mattoli S. A bronchial epithelial cell-derived factor in asthma that promotes eosinophil activation and survival as GM-CSF. Am J Physiol. 1991; 260(6 Pt 1):L530–L538.
Article42. Mattoli S, Stacey MA, Sun G, Bellini A, Marini M. Eotaxin expression and eosinophilic inflammation in asthma. Biochem Biophys Res Commun. 1997; 236:299–301.
Article43. Seminario MC, Gleich GJ. The role of eosinophils in the pathogenesis of asthma. Curr Opin Immunol. 1994; 6:860–864.
Article44. Akan A, Azkur D, Ginis T, Toyran M, Kaya A, Vezir E, Ozcan C, Ginis Z, Kocabas CN. Vitamin D level in children is correlated with severity of atopic dermatitis but only in patients with allergic sensitizations. Pediatr Dermatol. 2013; 30:359–363.
Article45. Zuercher AW, Weiss M, Holvoet S, Moser M, Moussu H, van Overtvelt L, Horiot S, Moingeon P, Nutten S, Prioult G, Singh A, Mercenier A. Lactococcus lactis NCC 2287 alleviates food allergic manifestations in sensitized mice by reducing IL-13 expression specifically in the ileum. Clin Dev Immunol. 2012; 2012:485750.46. Hawrelak JA, Myers SP. The causes of intestinal dysbiosis: a review. Altern Med Rev. 2004; 9:180–197.47. Abrahamsson TR, Jakobsson HE, Andersson AF, Bjorksten B, Engstrand L, Jenmalm MC. Low gut microbiota diversity in early infancy precedes asthma at school age. Clin Exp Allergy. 2014; 44:842–850.
Article48. Osborn DA, Sinn JK. Probiotics in infants for prevention of allergic disease and food hypersensitivity. Cochrane Database Syst Rev. 2007; (4):CD006475.
Article49. Pyar H, Liong MT, Peh KK. Recent advances in probiotics and biomedical applications. J Med Sci. 2013; 13:601–614.
Article50. Vong L, Lorentz RJ, Assa A, Glogauer M, Sherman PM. Probiotic Lactobacillus rhamnosus inhibits the formation of neutrophil extracellular traps. J Immunol. 2014; 192:1870–1877.51. Hinz D, Simon JC, Maier-Simon C, Milkova L, Roder S, Sack U, Borte M, Lehmann I, Herberth G. Reduced maternal regulatory T cell numbers and increased T helper type 2 cytokine production are associated with elevated levels of immunoglobulin E in cord blood. Clin Exp Allergy. 2010; 40:419–426.
Article52. Wu CC, Liao EC, Lee MF, Tsai JJ. Augmentation of regulatory T cells in allergic individuals by recombinant Der f 2 peptide with fungal immunomodulatory peptide fve. Ann Allergy Asthma Immunol. 2009; 102:216–222.
Article53. Schwarze J, Cieslewicz G, Joetham A, Sun LK, Sun WN, Chang TW, Hamelmann E, Gelfand EW. Antigen-specific immunoglobulin-A prevents increased airway responsiveness and lung eosinophilia after airway challenge in sensitized mice. Am J Respir Crit Care Med. 1998; 158:519–525.
Article54. Takabayashi K, Libet L, Chisholm D, Zubeldia J, Horner AA. Intranasal immunotherapy is more effective than intradermal immunotherapy for the induction of airway allergen tolerance in Th2-sensitized mice. J Immunol. 2003; 170:3898–3905.
Article55. Liu YH, Tsai JJ. Production of salivary immunoglobulin A and suppression of Dermatophagoides pteronyssinus-induced airway inflammation by local nasal immunotherapy. Int Arch Allergy Immunol. 2005; 138:161–168.56. Chiu YH, Lin SL, Tsai JJ, Lin MY. Probiotic actions on diseases: implications for therapeutic treatments. Food Funct. 2014; 5:625–634.
Article57. Chiua YH, Tsaib JJ, Linc SL, Chotirosvakina C, Lina MY. Characterisation of bifidobacteria with immunomodulatory properties isolated from human breast milk. J Funct Food. 2014; 7:700–708.58. Penders J, Thijs C, van den Brandt PA, Kummeling I, Snijders B, Stelma F, Adams H, van Ree R, Stobberingh EE. Gut microbiota composition and development of atopic manifestations in infancy: the KOALA Birth Cohort Study. Gut. 2007; 56:661–667.
Article59. Dolle S, Berg J, Rasche C, Worm M. Tolerability and clinical outcome of coseasonal treatment with Escherichia coli strain Nissle 1917 in grass pollen-allergic subjects. Int Arch Allergy Immunol. 2014; 163:29–35.60. Martinez-Canavate A, Sierra S, Lara-Villoslada F, Romero J, Maldonado J, Boza J, Xaus J, Olivares M. A probiotic dairy product containing L. gasseri CECT5714 and L. coryniformis CECT5711 induces immunological changes in children suffering from allergy. Pediatr Allergy Immunol. 2009; 20:592–600.61. Boyle RJ, Ismail IH, Kivivuori S, Licciardi PV, Robins-Browne RM, Mah LJ, Axelrad C, Moore S, Donath S, Carlin JB, Lahtinen SJ, Tang ML. Lactobacillus GG treatment during pregnancy for the prevention of eczema: a randomized controlled trial. Allergy. 2011; 66:509–516.
Article62. Allen SJ, Jordan S, Storey M, Thornton CA, Gravenor MB, Garaiova I, Plummer SF, Wang D, Morgan G. Probiotics in the prevention of eczema: a randomised controlled trial. Arch Dis Child. 2014; 99:1014–1019.
Article63. Yoshida T, Fujiwara W, Enomoto M, Nakayama S, Matsuda H, Sugiyama H, Shimojoh M, Okada S, Hattori M. An increased number of CD4+CD25+ cells induced by an oral administration of Lactobacillus plantarum NRIC0380 are involved in antiallergic activity. Int Arch Allergy Immunol. 2013; 162:283–289.64. Kim HJ, Kim YJ, Kang MJ, Seo JH, Kim HY, Jeong SK, Lee SH, Kim JM, Hong SJ. A novel mouse model of atopic dermatitis with epicutaneous allergen sensitization and the effect of Lactobacillus rhamnosus. Exp Dermatol. 2012; 21:672–675.65. Jang SO, Kim HJ, Kim YJ, Kang MJ, Kwon JW, Seo JH, Kim HY, Kim BJ, Yu J, Hong SJ. Asthma prevention by Lactobacillus Rhamnosus in a mouse model is associated with CD4(+)CD25(+)Foxp3(+) T cells. Allergy Asthma Immunol Res. 2012; 4:150–156.66. Lue KH, Sun HL, Lu KH, Ku MS, Sheu JN, Chan CH, Wang YH. A trial of adding Lactobacillus johnsonii EM1 to levocetirizine for treatment of perennial allergic rhinitis in children aged 7-12 years. Int J Pediatr Otorhinolaryngol. 2012; 76:994–1001.67. Lin TY, Chen CJ, Chen LK, Wen SH, Jan RH. Effect of probiotics on allergic rhinitis in Df, Dp or dust-sensitive children: a randomized double blind controlled trial. Indian Pediatr. 2013; 50:209–213.
Article68. Wassenberg J, Nutten S, Audran R, Barbier N, Aubert V, Moulin J, Mercenier A, Spertini F. Effect of Lactobacillus paracasei ST11 on a nasal provocation test with grass pollen in allergic rhinitis. Clin Exp Allergy. 2011; 41:565–573.
Article69. Schabussova I, Hufnagl K, Tang ML, Hoflehner E, Wagner A, Loupal G, Nutten S, Zuercher A, Mercenier A, Wiedermann U. Perinatal maternal administration of Lactobacillus paracasei NCC 2461 prevents allergic inflammation in a mouse model of birch pollen allergy. PLoS One. 2012; 7:e40271.
Article70. Lin WY, Fu LS, Lin HK, Shen CY, Chen YJ. Evaluation of the effect of Lactobacillus paracasei (HF.A00232) in children (6-13 years old) with perennial allergic rhinitis: a 12-week, double-blind, randomized, placebo-controlled study. Pediatr Neonatol. 2014; 55:181–188.
Article71. Loo EX, Llanora GV, Lu Q, Aw MM, Lee BW, Shek LP. Supplementation with probiotics in the first 6 months of life did not protect against eczema and allergy in at-risk Asian infants: a 5-year follow-up. Int Arch Allergy Immunol. 2014; 163:25–28.
Article72. West CE, Hammarström ML, Hernell O. Probiotics in primary prevention of allergic disease: follow-up at 8-9 years of age. Allergy. 2013; 68:1015–1020.73. Ivory K, Wilson AM, Sankaran P, Westwood M, McCarville J, Brockwell C, Clark A, Dainty JR, Zuidmeer-Jongejan L, Nicoletti C. Oral delivery of a probiotic induced changes at the nasal mucosa of seasonal allergic rhinitis subjects after local allergen challenge: a randomised clinical trial. PLoS One. 2013; 8:e78650.
Article74. Chiu YH, Tsai JJ, Lin SL, Lin MY. Lactobacillus casei MYL01 modulates the proinflammatory state induced by ethanol in an in vitro model. J Dairy Sci. 2014; 97:2009–2016.
Article75. Ou CC, Lin SL, Tsai JJ, Lin MY. Heat-killed lactic acid bacteria enhance immunomodulatory potential by skewing the immune response toward Th1 polarization. J Food Sci. 2011; 76:M260–M267.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Sensitization of house dust mites in the allergic patients and mite ecology in their house dusts
- Effectiveness of Indoor Environment Management Education for Prevention of Allergic Asthma
- T lymphocyte responses to house dust mite in asthmatic children
- Determination of specific IgE to two major allergens(Der fI and Der fII) of house dust mite(D.farinae) in Korean adult respiratory allergy patients
- Indoor Allergen Avoidance and Asthma