Yonsei Med J.
2008 Feb;49(1):1-18.
Role of Brain Inflammation in Epileptogenesis
- Affiliations
-
- 1Department of Pediatrics, Division of Neurology, Northwestern University Children's Memorial Hospital, Chicago, IL, USA. skoh@childrens memorial.org
- 2Department of Pediatrics, Seoul National University Boramae Hospital, Seoul, Korea.
Abstract
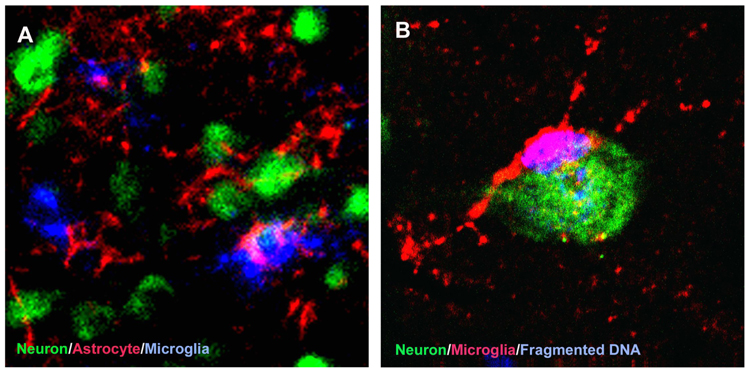
- Inflammation is known to participate in the mediation of a growing number of acute and chronic neurological disorders. Even so, the involvement of inflammation in the pathogenesis of epilepsy and seizure-induced brain damage has only recently been appreciated. Inflammatory processes, including activation of microglia and astrocytes and production of proinflammatory cytokines and related molecules, have been described in human epilepsy patients as well as in experimental models of epilepsy. For many decades, a functional role for brain inflammation has been implied by the effective use of anti-inflammatory treatments, such as steroids, in treating intractable pediatric epilepsy of diverse causes. Conversely, common pediatric infectious or autoimmune diseases are often accompanied by seizures during the course of illness. In addition, genetic susceptibility to inflammation correlated with an increased risk of epilepsy. Mounting evidence thus supports the hypothesis that inflammation may contribute to epileptogenesis and cause neuronal injury in epilepsy. We provide an overview of the current knowledge that implicates brain inflammation as a common predisposing factor in epilepsy, particularly childhood epilepsy.
Keyword
MeSH Terms
Figure
Reference
-
1. Hauser WA. The prevalence and incidence of convulsive disorders in children. Epilepsia. 1994. 35:Suppl 2. S1–S6.
Article2. Shinnar S, Pellock JM. Update on the epidemiology and prognosis of pediatric epilepsy. J Child Neurol. 2002. 17:Suppl 1. S4–S17.
Article3. Berg AT, Shinnar S, Levy SR, Testa FM. Newly diagnosed epilepsy in children: presentation at diagnosis. Epilepsia. 1999. 40:445–452.
Article4. Hauser WA HD. Epilepsy: Frequency, Causes and Consequences. 1990. New York: Demos.5. Ballabh P, Braun A, Nedergaard M. The blood-brain barrier: an overview: structure, regulation, and clinical implications. Neurobiol Dis. 2004. 16:1–13.6. Neuhaus J, Risau W, Wolburg H. Induction of blood-brain barrier characteristics in bovine brain endothelial cells by rat astroglial cells in transfilter coculture. Ann N Y Acad Sci. 1991. 633:578–580.
Article7. Krizanac-Bengez L, Mayberg MR, Janigro D. The cerebral vasculature as a therapeutic target for neurological disorders and the role of shear stress in vascular homeostatis and pathophysiology. Neurol Res. 2004. 26:846–853.
Article8. Feuerstein GZ, Liu T, Barone FC. Cytokines, inflammation, and brain injury: role of tumor necrosis factor-alpha. Cerebrovasc Brain Metab Rev. 1994. 6:341–360.9. Tarkowski E, Rosengren L, Blomstrand C, Wikkelsö C, Jensen C, Ekholm S, et al. Intrathecal release of pro- and anti-inflammatory cytokines during stroke. Clin Exp Immunol. 1997. 110:492–499.
Article10. Rider LG, Thapa PB, Del Beccaro MA, Gale JL, Foy HM, Farwell JR, et al. Cerebrospinal fluid analysis in children with seizures. Pediatr Emerg Care. 1995. 11:226–229.
Article11. Zhang W, Smith C, Howlett C, Stanimirovic D. Inflammatory activation of human brain endothelial cells by hypoxic astrocytes in vitro is mediated by IL-1beta. J Cereb Blood Flow Metab. 2000. 20:967–978.
Article12. deVeber G, Roach ES, Riela AR, Wiznitzer M. Stroke in children: recognition, treatment, and future directions. Semin Pediatr Neurol. 2000. 7:309–317.
Article13. Lynch JK, Nelson KB. Epidemiology of perinatal stroke. Curr Opin Pediatr. 2001. 13:499–505.
Article14. Kirkham FJ, DeBaun MR. Stroke in Children with Sickle Cell Disease. Curr Treat Options Neurol. 2004. 6:357–375.
Article15. Aso K, Scher MS, Barmada MA. Cerebral infarcts and seizures in the neonate. J Child Neurol. 1990. 5:224–228.
Article16. Nelson KB, Lynch JK. Stroke in newborn infants. Lancet Neurol. 2004. 3:150–158.
Article17. Sreenan C, Bhargava R, Robertson CM. Cerebral infarction in the term newborn: clinical presentation and long-term outcome. J Pediatr. 2000. 137:351–355.
Article18. Golomb MR, Garg BP, Carvalho KS, Johnson CS, Williams LS. Perinatal stroke and the risk of developing childhood epilepsy. J Pediatr. 2007. 151:409–413. 413.e1–413.e2.
Article19. Yang JS, Park YD, Hartlage PL. Seizures associated with stroke in childhood. Pediatr Neurol. 1995. 12:136–138.
Article20. Lanska MJ, Lanska DJ, Horwitz SJ, Aram DM. Presentation, clinical course, and outcome of childhood stroke. Pediatr Neurol. 1991. 7:333–341.
Article21. Tarkowski E, Rosengren L, Blomstrand C, Wikkelsö C, Jensen C, Ekholm S, et al. Early intrathecal production of interleukin-6 predicts the size of brain lesion in stroke. Stroke. 1995. 26:1393–1398.
Article22. Cutler SM, Pettus EH, Hoffman SW, Stein DG. Tapered progesterone withdrawal enhances behavioral and molecular recovery after traumatic brain injury. Exp Neurol. 2005. 195:423–429.
Article23. Lee T, von Scheven E, Sandborg C. Systemic lupus erythematosus and antiphospholipid syndrome in children and adolescents. Curr Opin Rheumatol. 2001. 13:415–421.
Article24. Toubi E, Khamashta MA, Panarra A, Hughes GR. Association of antiphospholipid antibodies with central nervous system disease in systemic lupus erythematosus. Am J Med. 1995. 99:397–401.
Article25. Liou HH, Wang CR, Chen CJ, Chen RC, Chuang CY, Chiang IP, et al. Elevated levels of anticardiolipin antibodies and epilepsy in lupus patients. Lupus. 1996. 5:307–312.
Article26. Watemberg N, Greenstein D, Levine A. Encephalopathy associated with Hashimoto thyroiditis: pediatric perspective. J Child Neurol. 2006. 21:1–5.
Article27. Stratigos AJ, Laskaris G, Stratigos JD. Behçet's disease. Semin Neurol. 1992. 12:346–357.
Article28. Joseph FG, Scolding NJ. Neuro-Behçet's disease in Caucasians: a study of 22 patients. Eur J Neurol. 2007. 14:174–180.
Article29. Mantegazza R, Bernasconi P, Baggi F, Spreafico R, Ragona F, Antozzi C, et al. Antibodies against GluR3 peptides are not specific for Rasmussen's encephalitis but are also present in epilepsy patients with severe, early onset disease and intractable seizures. J Neuroimmunol. 2002. 131:179–185.
Article30. Peltola JT, Haapala A, Isojärvi JI, Auvinen A, Palmio J, Latvala K, et al. Antiphospholipid and antinuclear antibodies in patients with epilepsy or new-onset seizure disorders. Am J Med. 2000. 109:712–717.
Article31. Eriksson K, Peltola J, Keränen T, Haapala AM, Koivikko M. High prevalence of antiphospholipid antibodies in children with epilepsy: a controlled study of 50 cases. Epilepsy Res. 2001. 46:129–137.
Article32. Yoshimura K, Konishi T, Kotani H, Wakiguchi H, Kurashige T. Prevalence of positive anticardiolipin antibody in benign infantile convulsion. Brain Dev. 2001. 23:317–320.
Article33. Shrivastava A, Dwivedi S, Aggarwal A, Misra R. Anti-cardiolipin and anti-beta2 glycoprotein I antibodies in Indian patients with systemic lupus erythematosus: association with the presence of seizures. Lupus. 2001. 10:45–50.
Article34. Nelson KB, Ellenberg JH. Predictors of epilepsy in children who have experienced febrile seizures. N Engl J Med. 1976. 295:1029–1033.
Article35. Millichap JG. Studies in febrile seizures. I. Height of body temperature as a measure of the febrile-seizure threshold. Pediatrics. 1959. 23(1 Pt 1):76–85.36. Virta M, Hurme M, Helminen M. Increased frequency of interleukin-1beta (-511) allele 2 in febrile seizures. Pediatr Neurol. 2002. 26:192–195.37. Kanemoto K, Kawasaki J, Yuasa S, Kumaki T, Tomohiro O, Kaji R, et al. Increased frequency of interleukin-1beta-511T allele in patients with temporal lobe epilepsy, hippocampal sclerosis, and prolonged febrile convulsion. Epilepsia. 2003. 44:796–799.
Article38. Dubé C, Vezzani A, Behrens M, Bartfai T, Baram TZ. Interleukin-1beta contributes to the generation of experimental febrile seizures. Ann Neurol. 2005. 57:152–155.
Article39. Hall CB, Long CE, Schnabel KC, Caserta MT, McIntyre KM, Costanzo MA, et al. Human herpesvirus-6 infection in children. A prospective study of complications and reactivation. N Engl J Med. 1994. 331:432–438.
Article40. Chiu SS, Tse CY, Lau YL, Peiris M. Influenza A infection is an important cause of febrile seizures. Pediatrics. 2001. 108:E63.
Article41. Asano Y, Yoshikawa T, Suga S, Kobayashi I, Nakashima T, Yazaki T, et al. Clinical features of infants with primary human herpesvirus 6 infection (exanthem subitum, roseola infantum). Pediatrics. 1994. 93:104–108.
Article42. Jee SH, Long CE, Schnabel KC, Sehgal N, Epstein LG, Hall CB. Risk of recurrent seizures after a primary human herpesvirus 6-induced febrile seizure. Pediatr Infect Dis J. 1998. 17:43–48.
Article43. Bertolani MF, Portolani M, Marotti F, Sabbattini AM, Chiossi C, Bandieri MR, et al. A study of childhood febrile convulsions with particular reference to HHV-6 infection: pathogenic considerations. Childs Nerv Syst. 1996. 12:534–539.
Article44. Kondo K, Nagafuji H, Hata A, Tomomori C, Yamanishi K. Association of human herpesvirus 6 infection of the central nervous system with recurrence of febrile convulsions. J Infect Dis. 1993. 167:1197–1200.
Article45. Kawada J, Kimura H, Ito Y, Hara S, Iriyama M, Yoshikawa T, et al. Systemic cytokine responses in patients with influenza-associated encephalopathy. J Infect Dis. 2003. 188:690–698.
Article46. Masuyama T, Matsuo M, Ichimaru T, Ishii K, Tsuchiya K, Hamasaki Y. Possible contribution of interferon-alpha to febrile seizures in influenza. Pediatr Neurol. 2002. 27:289–292.47. Vestergaard M, Hviid A, Madsen KM, Wohlfahrt J, Thorsen P, Schendel D, et al. MMR vaccination and febrile seizures: evaluation of susceptible subgroups and long-term prognosis. JAMA. 2004. 292:351–357.48. Barlow WE, Davis RL, Glasser JW, Rhodes PH, Thompson RS, Mullooly JP, et al. The risk of seizures after receipt of whole-cell pertussis or measles, mumps, and rubella vaccine. N Engl J Med. 2001. 345:656–661.
Article49. Hirtz DG, Nelson KB, Ellenberg JH. Seizures following childhood immunizations. J Pediatr. 1983. 102:14–18.
Article50. Contino MF, Lebby T, Arcinue EL. Rotaviral gastrointestinal infection causing afebrile seizures in infancy and childhood. Am J Emerg Med. 1994. 12:94–95.
Article51. Nishimura S, Ushijima H, Nishimura S, Shiraishi H, Kanazawa C, Abe T, et al. Detection of rotavirus in cerebrospinal fluid and blood of patients with convulsions and gastroenteritis by means of the reverse transcription polymerase chain reaction. Brain Dev. 1993. 15:457–459.
Article52. Ushijima H, Bosu K, Abe T, Shinozaki T. Suspected rotavirus encephalitis. Arch Dis Child. 1986. 61:692–694.
Article53. Saulsbury FT, Winkelstein JA, Yolken RH. Chronic rotavirus infection in immunodeficiency. J Pediatr. 1980. 97:61–65.
Article54. Chen HJ, Chen BS, Wang SF, Lai MH. Rotavirus gastroenteritis in children: a clinical study of 125 patients in Hsin-Tien area. Zhonghua Min Guo Xiao Er Ke Yi Xue Hui Za Zhi. 1991. 32:73–78.55. Prasad AN, Stafstrom CF, Holmes GL. Alternative epilepsy therapies: the ketogenic diet, immunoglobulins, and steroids. Epilepsia. 1996. 37:Suppl 1. S81–S95.
Article56. Klein R, Livingston S. The effect of adrenocorticotropic hormone in epilepsy. J Pediatr. 1950. 37:733–742.
Article57. Hrachovy RA, Frost JD Jr, Glaze DG. High-dose, long-duration versus low-dose, short-duration corticotropin therapy for infantile spasms. The Journal of pediatrics. 1994. 124(5 Pt 1):803–806.
Article58. Joëls M. Corticosteroid actions in the hippocampus. J Neuroendocrinol. 2001. 13:657–669.
Article59. Reddy DS, Rogawski MA. Enhanced anticonvulsant activity of ganaxolone after neurosteroid withdrawal in a rat model of catamenial epilepsy. J Pharmacol Exp Ther. 2000. 294:909–915.60. Baram TZ, Hatalski CG. Neuropeptide-mediated excitability: a key triggering mechanism for seizure generation in the developing brain. Trends Neurosci. 1998. 21:471–476.
Article61. Rasmussen T, Olszewski J, Lloydsmith D. Focal seizures due to chronic localized encephalitis. Neurology. 1958. 8:435–445.
Article62. Bauer J, Elger CE, Hans VH, Schramm J, Urbach H, Lassmann H, et al. Astrocytes are a specific immunological target in Rasmussen's encephalitis. Ann Neurol. 2007. 62:67–80.
Article63. Rogers SW, Andrews PI, Gahring LC, Whisenand T, Cauley K, Crain B, et al. Autoantibodies to glutamate receptor GluR3 in Rasmussen's encephalitis. Science. 1994. 265:648–651.
Article64. Bahi-Buisson N, Villanueva V, Bulteau C, Delalande O, Dulac O, Chiron C, et al. Long term response to steroid therapy in Rasmussen encephalitis. Seizure. 2007. 16:485–492.
Article65. Cowan LD, Hudson LS. The epidemiology and natural history of infantile spasms. J Child Neurol. 1991. 6:355–364.
Article66. Cowan LD, Bodensteiner JB, Leviton A, Doherty L. Prevalence of the epilepsies in children and adolescents. Epilepsia. 1989. 30:94–106.
Article67. Aicardi J. Aicardi J, editor. Infantile spasms and related syndromes. Epilepsy in children. 1986. New York: Raven Press.68. Riikonen R. Infantile spasms: some new theoretical aspects. Epilepsia. 1983. 24:159–168.
Article69. Baram TZ. Pathophysiology of massive infantile spasms: perspective on the putative role of the brain adrenal axis. Ann Neurol. 1993. 33:231–236.
Article70. Low NL. Infantile spasms with mental retardation. II. Treatment with cortisone and adrenocorticotropin. Pediatrics. 1958. 22:1165–1169.71. Mackay MT, Weiss SK, Adams-Webber T, Ashwal S, Stephens D, Ballaban-Gill K, et al. Practice parameter: medical treatment of infantile spasms: report of the American Academy of Neurology and the Child Neurology Society. Neurology. 2004. 62:1668–1681.
Article72. Baram TZ, Mitchell WG, Tournay A, Snead OC, Hanson RA, Horton EJ. High-dose corticotropin (ACTH) versus prednisone for infantile spasms: a prospective, randomized, blinded study. Pediatrics. 1996. 97:375–379.
Article73. Hrachovy RA, Frost JD Jr, Kellaway P, Zion TE. Double-blind study of ACTH vs prednisone therapy in infantile spasms. J Pediatr. 1983. 103:641–645.
Article74. Lombroso CT. A prospective study of infantile spasms: clinical and therapeutic correlations. Epilepsia. 1983. 24:135–158.
Article75. Eisermann MM, DeLaRaillère A, Dellatolas G, Tozzi E, Nabbout R, Dulac O, et al. Infantile spasms in Down syndrome--effects of delayed anticonvulsive treatment. Epilepsy Res. 2003. 55:21–27.
Article76. Heiskala H. Community-based study of Lennox-Gastaut syndrome. Epilepsia. 1997. 38:526–531.
Article77. Sinclair DB. Prednisone therapy in pediatric epilepsy. Pediatr Neurol. 2003. 28:194–198.
Article78. Yamatogi Y, Ohtsuka Y, Ishida T, Ichiba N, Ishida S, Miyake S, et al. Treatment of the Lennox syndrome with ACTH: a clinical and electroencephalographic study. Brain Dev. 1979. 1:267–276.
Article79. Landau WM, Kleffner FR. Syndrome of acquired aphasia with convulsive disorder in children. Neurology. 1957. 7:523–530.
Article80. Sinclair DB, Snyder TJ. Corticosteroids for the treatment of Landau-kleffner syndrome and continuous spike-wave discharge during sleep. Pediatr Neurol. 2005. 32:300–306.
Article81. Tsuru T, Mori M, Mizuguchi M, Momoi MY. Effects of high-dose intravenous corticosteroid therapy in Landau-Kleffner syndrome. Pediatr Neurol. 2000. 22:145–147.
Article82. Tassinari CA BM, Dravet C, Dalla Bernardina B, Roger J. Roger J, Bureau M, Dravet C, Genton P, Tassinari CA, Wolf P, editors. Epilepsy with continuous spikes and waves during slow sleep-otherwise described as epilepsy with electrical status epilepticus during slow sleep (ESES). Epileptic syndromes in infancy, childhood and adolescence. 2002. 3rd ed. London: John Libbey.83. Gallagher S, Weiss S, Oram Cardy J, Humphries T, Harman KE, Menascu S. Efficacy of very high dose steroid treatment in a case of Landau-Kleffner syndrome. Dev Med Child Neurol. 2006. 48:766–769.
Article84. Snead OC 3rd, Benton JW, Myers GJ. ACTH and prednisone in childhood seizure disorders. Neurology. 1983. 33:966–970.
Article85. Oguni H, Hayashi K, Awaya Y, Fukuyama Y, Osawa M. Severe myoclonic epilepsy in infants--a review based on the Tokyo Women's Medical University series of 84 cases. Brain Dev. 2001. 23:736–748.
Article86. Verhelst H, Boon P, Buyse G, Ceulemans B, D'Hooghe M, Meirleir LD, et al. Steroids in intractable childhood epilepsy: clinical experience and review of the literature. Seizure. 2005. 14:412–421.
Article87. Plata-Salamán CR, Ilyin SE, Turrin NP, Gayle D, Flynn MC, Romanovitch AE, et al. Kindling modulates the IL-1beta system, TNF-alpha, TGF-beta1, and neuropeptide mRNAs in specific brain regions. Brain Res Mol Brain Res. 2000. 75:248–258.
Article88. Zimmer LA, Ennis M, Shipley MT. Soman-induced seizures rapidly activate astrocytes and microglia in discrete brain regions. J Comp Neurol. 1997. 378:482–492.
Article89. Turrin NP, Rivest S. Innate immune reaction in response to seizures: implications for the neuropathology associated with epilepsy. Neurobiol Dis. 2004. 16:321–334.
Article90. Jankowsky JL, Patterson PH. The role of cytokines and growth factors in seizures and their sequelae. Prog Neurobiol. 2001. 63:125–149.
Article91. McNamara JO. Cellular and molecular basis of epilepsy. J Neurosci. 1994. 14:3413–3425.
Article92. Parent JM, Yu TW, Leibowitz RT, Geschwind DH, Sloviter RS, Lowenstein DH. Dentate granule cell neurogenesis is increased by seizures and contributes to aberrant network reorganization in the adult rat hippocampus. J Neurosci. 1997. 17:3727–3738.
Article93. Koh S, Storey TW, Santos TC, Mian AY, Cole AJ. Early-life seizures in rats increase susceptibility to seizure-induced brain injury in adulthood. Neurology. 1999. 53:915–921.
Article94. Aloisi F. Immune function of microglia. Glia. 2001. 36:165–179.
Article95. Kreutzberg GW. Microglia: a sensor for pathological events in the CNS. Trends Neurosci. 1996. 19:312–318.
Article96. Block ML, Hong JS. Microglia and inflammation-mediated neurodegeneration: multiple triggers with a common mechanism. Prog Neurobiol. 2005. 76:77–98.
Article97. Taniwaki Y, Kato M, Araki T, Kobayashi T. Microglial activation by epileptic activities through the propagation pathway of kainic acid-induced hippocampal seizures in the rat. Neurosci Lett. 1996. 217:29–32.
Article98. Rizzi M, Perego C, Aliprandi M, Richichi C, Ravizza T, Colella D, et al. Glia activation and cytokine increase in rat hippocampus by kainic acid-induced status epilepticus during postnatal development. Neurobiol Dis. 2003. 14:494–503.
Article99. Ravizza T, Rizzi M, Perego C, Richichi C, Velísková J, Moshé SL, et al. Inflammatory response and glia activation in developing rat hippocampus after status epilepticus. Epilepsia. 2005. 46:Suppl 5. 113–117.
Article100. Fountain NB. Status epilepticus: risk factors and complications. Epilepsia. 2000. 41:Suppl 2. S23–S30.
Article101. Henshall DC. Apoptosis signalling pathways in seizure-induced neuronal death and epilepsy. Biochem Soc Trans. 2007. 35(Pt 2):421–423.
Article102. Kang TC, Kim DS, Kwak SE, Kim JE, Won MH, Kim DW, et al. Epileptogenic roles of astroglial death and regeneration in the dentate gyrus of experimental temporal lobe epilepsy. Glia. 2006. 54:258–271.
Article103. Streit WJ, Walter SA, Pennell NA. Reactive microgliosis. Prog Neurobiol. 1999. 57:563–581.
Article104. Ekdahl CT, Claasen JH, Bonde S, Kokaia Z, Lindvall O. Inflammation is detrimental for neurogenesis in adult brain. Proc Natl Acad Sci U S A. 2003. 100:13632–13637.
Article105. Borges K, Gearing M, McDermott DL, Smith AB, Almonte AG, Wainer BH, et al. Neuronal and glial pathological changes during epileptogenesis in the mouse pilocarpine model. Exp Neurol. 2003. 182:21–34.
Article106. Brandt C, Potschka H, Löscher W, Ebert U. N-methyl-D-aspartate receptor blockade after status epilepticus protects against limbic brain damage but not against epilepsy in the kainate model of temporal lobe epilepsy. Neuroscience. 2003. 118:727–740.
Article107. Hanisch UK. Microglia as a source and target of cytokines. Glia. 2002. 40:140–155.
Article108. Aronica E, Gorter JA, Rozemuller AJ, Yankaya B, Troost D. Interleukin-1 beta down-regulates the expression of metabotropic glutamate receptor 5 in cultured human astrocytes. J Neuroimmunol. 2005. 160:188–194.
Article109. Tilleux S, Berger J, Hermans E. Induction of astrogliosis by activated microglia is associated with a down-regulation of metabotropic glutamate receptor 5. J Neuroimmunol. 2007. 189:23–30.
Article110. Seifert G, Schilling K, Steinhäuser C. Astrocyte dysfunction in neurological disorders: a molecular perspective. Nat Rev Neurosci. 2006. 7:194–206.
Article111. Gloor P. Epilepsy surgery. 1999. New York: Raven Press.112. Tian GF, Azmi H, Takano T, Xu Q, Peng W, Lin J, et al. An astrocytic basis of epilepsy. Nat Med. 2005. 11:973–981.
Article113. O'Connor ER, Sontheimer H, Spencer DD, de Lanerolle NC. Astrocytes from human hippocampal epileptogenic foci exhibit action potential-like responses. Epilepsia. 1998. 39:347–354.114. Jørgensen MB, Finsen BR, Jensen MB, Castellano B, Diemer NH, Zimmer J. Microglial and astroglial reactions to ischemic and kainic acid-induced lesions of the adult rat hippocampus. Exp Neurol. 1993. 120:70–88.
Article115. Somera-Molina KC, Robin B, Somera CA, Anderson C, Stine C, Koh S, et al. Glial activation links early-life seizures and long-term neurologic dysfunction: evidence using a small molecule inhibitor of proinflammatory cytokine upregulation. Epilepsia. 2007. 48:1785–1800.
Article116. Seifert G, Schröder W, Hinterkeuser S, Schumacher T, Schramm J, Steinhäuser C. Changes in flip/flop splicing of astroglial AMPA receptors in human temporal lobe epilepsy. Epilepsia. 2002. 43:Suppl 5. 162–167.
Article117. Schröder W, Hinterkeuser S, Seifert G, Schramm J, Jabs R, Wilkin GP, et al. Functional and molecular properties of human astrocytes in acute hippocampal slices obtained from patients with temporal lobe epilepsy. Epilepsia. 2000. 41:Suppl 6. S181–S184.
Article118. Fedele DE, Gouder N, Guttinger M, Gabernet L, Scheurer L, Rülicke T, et al. Astrogliosis in epilepsy leads to overexpression of adenosine kinase, resulting in seizure aggravation. Brain. 2005. 128(Pt 10):2383–2395.
Article119. Chung HKS. Encyclopedia of Basic Epilepsy Research. Elsevier: Burlington;in press.120. Vezzani A, Conti M, De Luigi A, Ravizza T, Moneta D, Marchesi F, et al. Interleukin-1beta immunoreactivity and microglia are enhanced in the rat hippocampus by focal kainate application: functional evidence for enhancement of electrographic seizures. J Neurosci. 1999. 19:5054–5065.
Article121. Oprica M, Eriksson C, Schultzberg M. Inflammatory mechanisms associated with brain damage induced by kainic acid with special reference to the interleukin-1 system. J Cell Mol Med. 2003. 7:127–140.
Article122. Vezzani A, Moneta D, Conti M, Richichi C, Ravizza T, De Luigi A, et al. Powerful anticonvulsant action of IL-1 receptor antagonist on intracerebral injection and astrocytic overexpression in mice. Proc Natl Acad Sci U S A. 2000. 97:11534–11539.
Article123. Bernardino L, Xapelli S, Silva AP, Jakobsen B, Poulsen FR, Oliveira CR, et al. Modulator effects of interleukin-1beta and tumor necrosis factor-alpha on AMPA-induced excitotoxicity in mouse organotypic hippocampal slice cultures. J Neurosci. 2005. 25:6734–6744.
Article124. Ravizza T, Gagliardi B, Noé F, Boer K, Aronica E, Vezzani A. Innate and adaptive immunity during epileptogenesis and spontaneous seizures: evidence from experimental models and human temporal lobe epilepsy. Neurobiol Dis. 2008. 29:142–160.
Article125. Beattie EC, Stellwagen D, Morishita W, Bresnahan JC, Ha BK, Von Zastrow M, et al. Control of synaptic strength by glial TNFalpha. Science. 2002. 295:2282–2285.126. Viviani B, Bartesaghi S, Gardoni F, Vezzani A, Behrens MM, Bartfai T, et al. Interleukin-1beta enhances NMDA receptor-mediated intracellular calcium increase through activation of the Src family of kinases. J Neurosci. 2003. 23:8692–8700.
Article127. Ye ZC, Sontheimer H. Cytokine modulation of glial glutamate uptake: a possible involvement of nitric oxide. Neuroreport. 1996. 7:2181–2185.128. Bezzi P, Volterra A. A neuron-glia signalling network in the active brain. Curr Opin Neurobiol. 2001. 11:387–394.
Article129. Samland H, Huitron-Resendiz S, Masliah E, Criado J, Henriksen SJ, Campbell IL. Profound increase in sensitivity to glutamatergic- but not cholinergic agonist-induced seizures in transgenic mice with astrocyte production of IL-6. J Neurosci Res. 2003. 73:176–187.
Article130. Patel HC, Boutin H, Allan SM. Interleukin-1 in the brain: mechanisms of action in acute neurodegeneration. Ann N Y Acad Sci. 2003. 992:39–47.131. Rothwell NJ, Luheshi GN. Interleukin 1 in the brain: biology, pathology and therapeutic target. Trends Neurosci. 2000. 23:618–625.
Article132. Panegyres PK, Hughes J. The neuroprotective effects of the recombinant interleukin-1 receptor antagonist rhIL-1ra after excitotoxic stimulation with kainic acid and its relationship to the amyloid precursor protein gene. J Neurol Sci. 1998. 154:123–132.
Article133. Giulian D, Li J, Li X, George J, Rutecki PA. The impact of microglia-derived cytokines upon gliosis in the CNS. Dev Neurosci. 1994. 16:128–136.
Article134. Bruce AJ, Boling W, Kindy MS, Peschon J, Kraemer PJ, Carpenter MK, et al. Altered neuronal and microglial responses to excitotoxic and ischemic brain injury in mice lacking TNF receptors. Nat Med. 1996. 2:788–794.
Article135. Ridet JL, Malhotra SK, Privat A, Gage FH. Reactive astrocytes: cellular and molecular cues to biological function. Trends Neurosci. 1997. 20:570–577.
Article136. Brett FM, Mizisin AP, Powell HC, Campbell IL. Evolution of neuropathologic abnormalities associated with blood-brain barrier breakdown in transgenic mice expressing interleukin-6 in astrocytes. J Neuropathol Exp Neurol. 1995. 54:766–775.
Article137. Campbell IL, Abraham CR, Masliah E, Kemper P, Inglis JD, Oldstone MB, et al. Neurologic disease induced in transgenic mice by cerebral overexpression of interleukin 6. Proc Natl Acad Sci U S A. 1993. 90:10061–10065.
Article138. Campbell IL. Transgenic mice and cytokine actions in the brain: bridging the gap between structural and functional neuropathology. Brain Res Brain Res Rev. 1998. 26:327–336.
Article139. Steffensen SC, Campbell IL, Henriksen SJ. Site-specific hippocampal pathophysiology due to cerebral overexpression of interleukin-6 in transgenic mice. Brain Res. 1994. 652:149–153.
Article140. Penkowa M, Molinero A, Carrasco J, Hidalgo J. Interleukin-6 deficiency reduces the brain inflammatory response and increases oxidative stress and neurodegeneration after kainic acid-induced seizures. Neuroscience. 2001. 102:805–818.
Article141. Brigande JV, Wieraszko A, Albert MD, Balkema GW, Seyfried TN. Biochemical correlates of epilepsy in the E1 mouse: analysis of glial fibrillary acidic protein and gangliosides. J Neurochem. 1992. 58:752–760.
Article142. Drage MG, Holmes GL, Seyfried TN. Hippocampal neurons and glia in epileptic EL mice. J Neurocytol. 2002. 31:681–692.143. Ingram EM, Wiseman JW, Tessler S, Emson PC. Reduction of glial glutamate transporters in the parietal cortex and hippocampus of the EL mouse. J Neurochem. 2001. 79:564–575.
Article144. Sheng JG, Boop FA, Mrak RE, Griffin WS. Increased neuronal beta-amyloid precursor protein expression in human temporal lobe epilepsy: association with interleukin-1 alpha immunoreactivity. J Neurochem. 1994. 63:1872–1879.
Article145. Crespel A, Coubes P, Rousset MC, Brana C, Rougier A, Rondouin G, et al. Inflammatory reactions in human medial temporal lobe epilepsy with hippocampal sclerosis. Brain Res. 2002. 952:159–169.
Article146. Maldonado M, Baybis M, Newman D, Kolson DL, Chen W, McKhann G 2nd, et al. Expression of ICAM-1, TNF-alpha, NF kappa B, and MAP kinase in tubers of the tuberous sclerosis complex. Neurobiol Dis. 2003. 14:279–290.
Article147. Baranzini SE, Laxer K, Bollen A, Oksenberg JR. Gene expression analysis reveals altered brain transcription of glutamate receptors and inflammatory genes in a patient with chronic focal (Rasmussen's) encephalitis. J Neuroimmunol. 2002. 128:9–15.
Article148. Vezzani A, Granata T. Brain inflammation in epilepsy: experimental and clinical evidence. Epilepsia. 2005. 46:1724–1743.
Article149. Hulkkonen J, Koskikallio E, Rainesalo S, Keränen T, Hurme M, Peltola J. The balance of inhibitory and excitatory cytokines is differently regulated in vivo and in vitro among therapy resistant epilepsy patients. Epilepsy Res. 2004. 59:199–205.
Article150. Peltola J, Hurme M, Miettinen A, Keränen T. Elevated levels of interleukin-6 may occur in cerebrospinal fluid from patients with recent epileptic seizures. Epilepsy Res. 1998. 31:129–133.
Article151. Peltola J, Palmio J, Korhonen L, Suhonen J, Miettinen A, Hurme M, et al. Interleukin-6 and interleukin-1 receptor antagonist in cerebrospinal fluid from patients with recent tonic-clonic seizures. Epilepsy Res. 2000. 41:205–211.
Article152. Kira R, Torisu H, Takemoto M, Nomura A, Sakai Y, Sanefuji M, et al. Genetic susceptibility to simple febrile seizures: interleukin-1beta promoter polymorphisms are associated with sporadic cases. Neurosci Lett. 2005. 384:239–244.
Article153. Beach TG, Woodhurst WB, MacDonald DB, Jones MW. Reactive microglia in hippocampal sclerosis associated with human temporal lobe epilepsy. Neurosci Lett. 1995. 191:27–30.
Article154. Aronica E, Gorter JA, Redeker S, Ramkema M, Spliet WG, van Rijen PC, et al. Distribution, characterization and clinical significance of microglia in glioneuronal tumours from patients with chronic intractable epilepsy. Neuropathol Appl Neurobiol. 2005. 31:280–291.
Article155. Boer K, Spliet WG, van Rijen PC, Redeker S, Troost D, Aronica E. Evidence of activated microglia in focal cortical dysplasia. J Neuroimmunol. 2006. 173:188–195.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Post-Traumatic Ictogenesis and Epileptogenesis
- Role of Inflammation in Neurological Disorders Associated with Epilepsy
- The role of cytokines in seizures: interleukin (IL)-1beta, IL-1Ra, IL-8, and IL-10
- The Mechanism of Anti-Epileptogenesis by Levetiracetam Treatment is Similar to the Spontaneous Recovery of Idiopathic Generalized Epilepsy during Adolescence
- Brain Inflammation and Epilepsy in Experimental Animals