Perinatology.
2017 Jun;28(2):74-78. 10.14734/PN.2017.28.2.74.
A Case of Neonatal Alloimmune Thrombocytopenia Due to Anti-HLA A29 Antibody
- Affiliations
-
- 1Department of Pediatrics, Korea University College of Medicine, Seoul, Korea. hongys@korea.ac.kr
- 2Department of Laboratory Medicine, Korea University College of Medicine, Seoul, Korea.
- KMID: 2386356
- DOI: http://doi.org/10.14734/PN.2017.28.2.74
Abstract
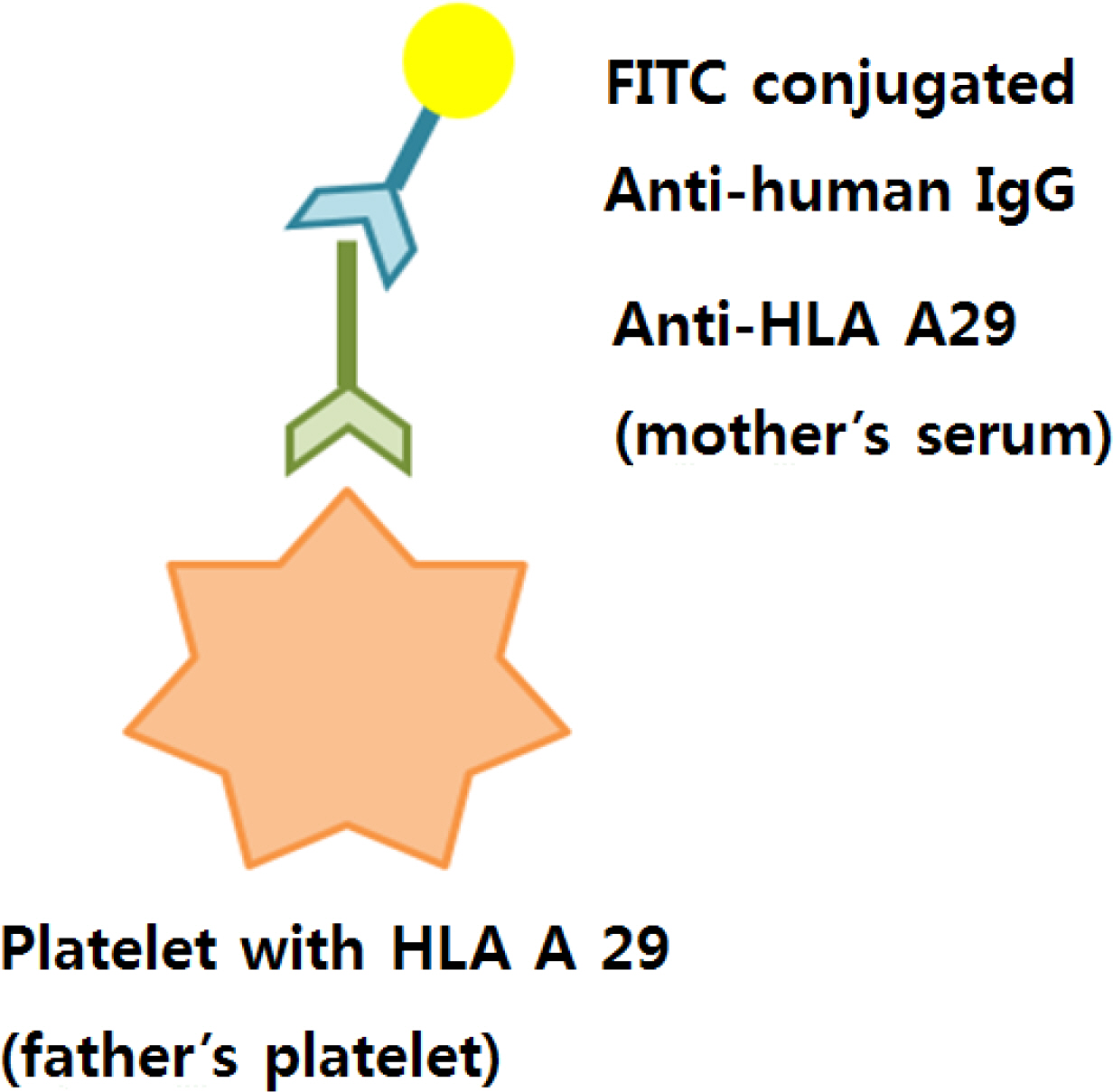
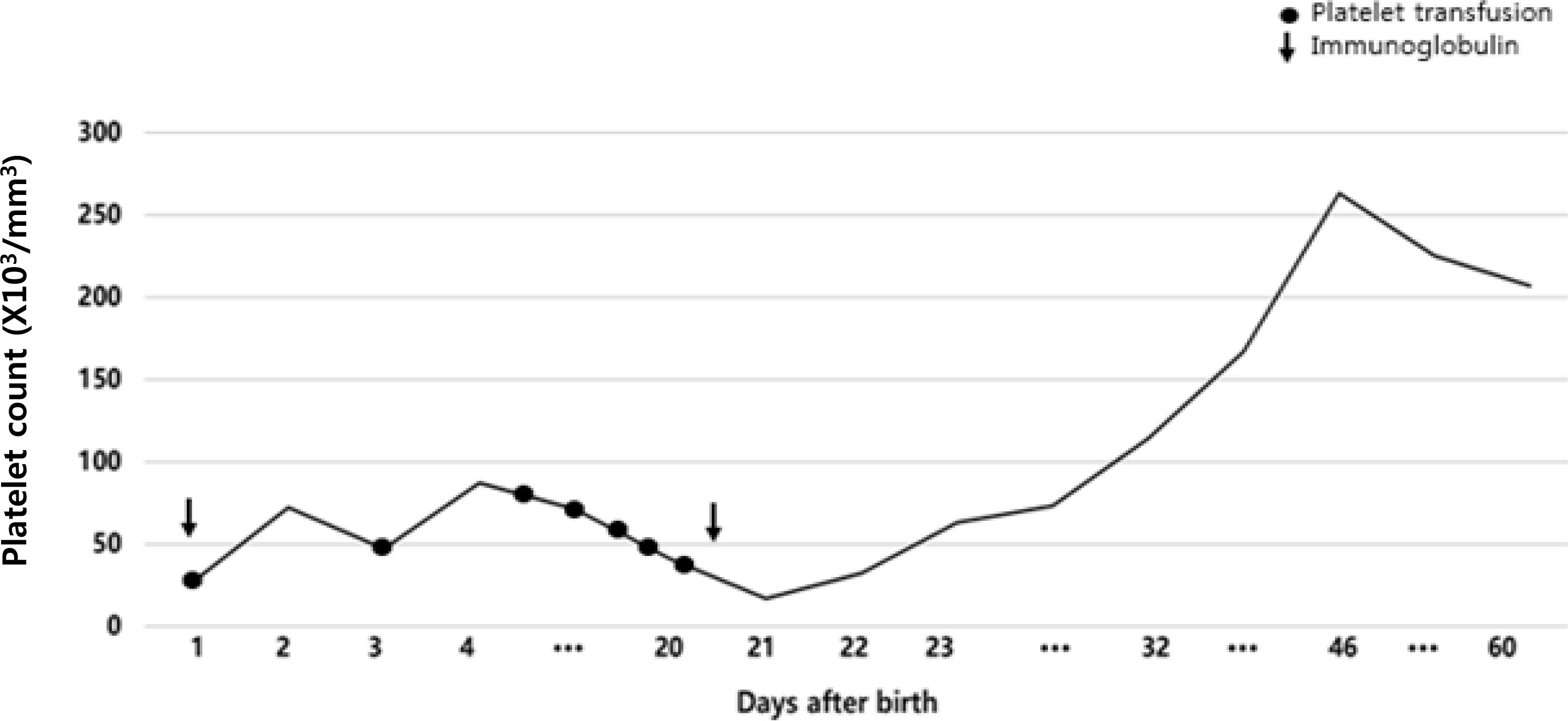
- Neonatal alloimmune thrombocytopenia (NAIT) occurs when a mother is immunized against fetal platelet-specific alloantigen and rarely human leukocyte antigen (HLA) inherited from the father. We experienced a case of NAIT caused by anti-HLA A29 antibody. The patient was first born female preterm infant. She had no petechiae or purpura and no evidence of infection at birth, but the platelet count was 27,000/mm³. The human platelet antigen specific antibodies were not detected in infant and her mother's sera. On panel reactive antibody (PRA) test, her mother's serum showed 96% HLA A29 antibody. On sequence specific primed polymerase chain reaction (SSP-PCR), anti-HLA A24, A31, B7, B51 antibodies were detected in her mother's serum, and anti-HLA A29, A31, B7, B51 antibodies in infant's serum. And on platelet immunofluorescent flow cytometry test (FCM) her mother's serum showed positive reaction with her father's platelet. These findings suggested that NAIT was caused by anti-HLA A29 antibody. The patient received platelet concentrates and intravenous immunoglobulin. The platelet count increased to 110,000/mm³ on the 32nd day of life and was maintained. On the CGH array performed because of her dysmorphic features, 16p 11.2 (1.2 Mb gain), which was considered benign copy number variation were revealed. We report a case of NAIT caused by anti-HLA A29 antibody accompanied by 16p11.2 (1.2 Mb gain).
MeSH Terms
Figure
Reference
-
1). Goldman M., Filion M., Proulx C., Chartrand P., Décary F. Neonatal alloimmune thrombocytopenia. Transfus Med Rev. 1994. 8:123–31.
Article2). Kaplan C. Foetal and neonatal alloimmune thrombocytopenia. Orphanet J Rare Dis. 2006. 1:39.3). Peterson JA., McFarland JG., Curtis BR., Aster RH. Neonatal alloimmune thrombocytopenia: pathogenesis, diagnosis and management. Br J Haematol. 2013. 161:3–14.
Article4). Lee MS., LEE HS., Kim HO. A case of neonatal alloimmune thrombocytopenia related to HLA antibody. J Korean Pediatr Soc. 2001. 44:1454–8.5). Shibata Y., Matsuda I., Miyaji T., Ichikawa Y. Yuka, a new platelet antigen involved in two cases of neonatal alloimmune thrombocytopenia. Vox Sang. 1986. 50:177–80.
Article6). Kim SY., Kim ER., Kim YJ., Park MH., Song EY., Han KS. A case of neonatal alloimmune trombocytopenia due to anti-HLA A2. J Korean Pediatr Soc. 2000. 43:861–5.7). Choi JS., Kim SY., Ihm C., Kim SY. A case of neonatal alloimmune trombocytopenia due to Anti-HLA-B35. J Korean Soc Neonatol. 2009. 16:248–54.8). Barber JC., Hall V., Maloney VK., Huang S., Roberts AM., Brady AF, et al. 16p11.2–p12.2 duplication syndrome; a genomic condition differentiated from euchromatic variation of 16p11.2. Eur J Hum Genet. 2013. 21:182–9.
Article9). Davoren A., Curtis BR., Aster RH., McFarland JG. Human platelet antigenspecific alloantibodies implicated in 1162 cases of neonatal alloimmune thrombocytopenia. Transfusion. 2004. 44:1220–5.
Article10). Curtis BR. Recent progress in understanding the pathogenesis of fetal and neonatal alloimmune thrombocytopenia. Br J Haematol. 2015. 171:671–82.
Article11). Han KS., Um TH., Park HM., Shin BM., Park YW., Kim SW. A case of neonatal alloimmune thrombocytopenia due to anti-HLA-B7+B60+B61. Korean J Blood Transfus. 1994. 5:45–51.12). Han KS., Cho HI., Kim SI. Frequency of platelet specific-antigens among Koreans determined by a simplified immunofluorescence test. Transfusion. 1989. 29:708–10.13). Espinoza JP., Caradeux J., Norwitz ER., Illanes SE. Fetal and neonatal alloimmune trombocytopenia. Rev Obstet Gynecol. 2013. 6:e15–21.14). Udom-Rice I., Bussel JB. Fetal and neonatal thrombocytopenia. Blood Rev. 1995. 9:57–64.
Article15). Taaning E., Antonsen H., Petersen S., Svejgaard A., Thomsen M. HLA antigens and maternal antibodies in alloimmune neonatal thrombocytopenia. Tissue Antigens. 1983. 21:351–9.
Article16). Kim Y., Oh EJ., Kim Y., Lee J., Sung IK. Neonatal alloimmune thrombocytopenia caused by anti–HLA–A2 alloantibodies determined by Luminex single antigen bead assay. Lab Med Online. 2013. 3:45–9.
Article17). Jung S., Oh EJ., Yang CW., Ahn WS., Kim Y., Park YJ, et al. Comparative evaluation of ELISA and luminex panel reactive antibody assays for HLA alloantibody screening. Korean J Lab Med. 2009. 29:473–80.
Article18). Oh EJ., Lee J., Yang CW., Moon IS., Park YJ., Han K. Comparison of anti-HLA detecting methods; cytotoxicity, flow cytometric crossmatch, multiple antigen-ELISA, single antigen-ELISA. J Korean Soc Transplant. 2008. 22:85–91.19). Banchette VS., Johnson J., Rand M. The management of alloimmune neonatal thrombocytopenia. Baillieres Best Pract Res Clin Haematol. 2000. 13:365–90.20). Madani K., Kamphuis MM., Lopriore E., Porcelijn L., Oepkes D. Delayed diagnosis of fetal and neonatal alloimmune thrombocytopenia: a cause of perinatal mortality and morbidity. BJOG. 2012. 119:1612–6.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Neonatal Alloimmune Thrombodytopenia Due to Anti - HLA Antibody
- A Case of Neonatal Alloimmune Thrombocytopenia Related to HLA Antibody
- A Case of Saethre - Chotzen Syndrome
- A Case of Neonatal Alloimmune Thrombocytopenia dut to Anti-HLA A2
- A case of neonatal alloimmune thrombocytopenia due to anti-HLA B44