Pediatr Gastroenterol Hepatol Nutr.
2015 Dec;18(4):286-291. 10.5223/pghn.2015.18.4.286.
Mesalizine-Induced Acute Pancreatitis and Interstitial Pneumonitis in a Patient with Ulcerative Colitis
- Affiliations
-
- 1Department of Pediatrics, Chosun University School of Medicine, Gwangju, Korea. krmoon@chosun.ac.kr
- KMID: 2383308
- DOI: http://doi.org/10.5223/pghn.2015.18.4.286
Abstract
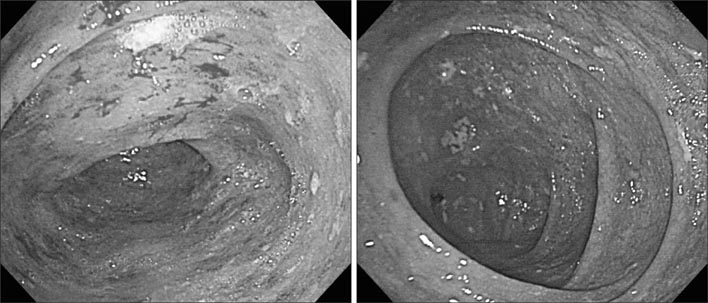
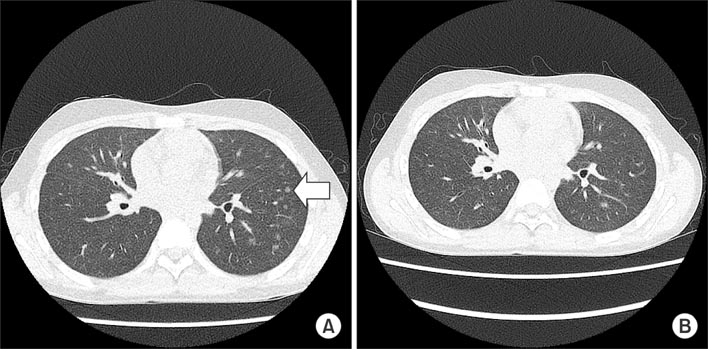
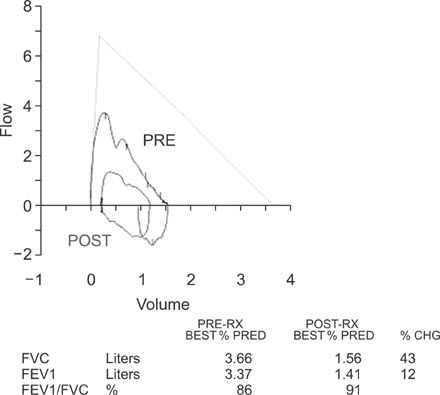
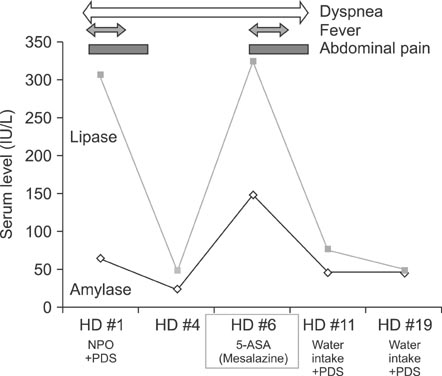
- Ulcerative colitis (UC) is a chronic idiopathic inflammatory bowel disease. Mesalizine for the first-line therapy of UC has adverse effects include pancreatitis, pneumonia and pericarditis. UC complicated by two coexisting conditions, however, is very rare. Moreover, drug-related pulmonary toxicity is particularly rare. An 11-year-old male patient was hospitalized for recurring upper abdominal pain after meals with vomiting, hematochezia and exertional dyspnea developing at 2 weeks of mesalizine therapy for UC. The serum level of lipase was elevated. Chest X-ray and thorax computed tomography showed interstitial pneumonitis. Mesalizine was discontinued and steroid therapy was initiated. Five days after admission, symptoms were resolved and mesalizine was resumed after a drop in amylase and lipase level. Symptoms returned the following day, however, accompanied by increased the serum levels of amylase and lipase. Mesalizine was discontinued again and recurring symptoms rapidly improved.
Keyword
MeSH Terms
Figure
Reference
-
1. Yang SK. Current status and clinical characteristics of inflammatory bowel disease in Korea. Korean J Gastroenterol. 2002; 40:1–14.2. Seo JK, Yeon KM, Chi JG. Inflammatory bowel disease in children--clinical, endoscopic, radiologic and histopathologic investigation. J Korean Med Sci. 1992; 7:221–235.
Article3. Xavier RJ, Podolsky DK. Unravelling the pathogenesis of inflammatory bowel disease. Nature. 2007; 448:427–434.
Article4. Ransford RA, Langman MJ. Sulphasalazine and mesalazine: serious adverse reactions re-evaluated on the basis of suspected adverse reaction reports to the Committee on Safety of Medicines. Gut. 2002; 51:536–539.
Article5. Candy S, Wright J, Gerber M, Adams G, Gerig M, Goodman R. A controlled double blind study of azathioprine in the management of Crohn's disease. Gut. 1995; 37:674–678.
Article6. Williams T, Eidus L, Thomas P. Fibrosing alveolitis, bronchiolitis obliterans, and sulfasalazine therapy. Chest. 1982; 81:766–768.
Article7. Fardy JM, Lloyd DA, Reynolds RP. Adverse effects with oral 5-aminosalicyclic acid. J Clin Gastroenterol. 1988; 10:635–637.
Article8. Toubanakis C, Batziou E, Sipsas N, Galanopoulos G, Tzivras M, Archimandritis A. Acute pancreatitis after long-term therapy with mesalazine, and hyperamylasaemia associated with azathioprine in a patient with ulcerative colitis. Eur J Gastroenterol Hepatol. 2003; 15:933–934.
Article9. Woltsche M, Woltsche-Kahr I, Roeger GM, Aberer W, Popper H. Sulfasalazine-induced extrinsic allergic alveolitis in a patient with psoriatic arthritis. Eur J Med Res. 2001; 6:495–497.10. Chikano S, Sawada K, Ohnishi K, Fukunaga K, Tanaka J, Shimoyama T. Interstitial pneumonia accompanying ulcerative colitis. Intern Med. 2001; 40:883–886.
Article11. Herrlinger KR, Stange EF. The pancreas and inflammatory bowel diseases. Int J Pancreatol. 2000; 27:171–179.
Article12. Fiorentini MT, Fracchia M, Galatola G, Barlotta A, de la Pierre M. Acute pancreatitis during oral 5-aminosalicylic acid therapy. Dig Dis Sci. 1990; 35:1180–1182.
Article13. Lankisch PG, Dröge M, Gottesleben F. Drug induced acute pancreatitis: incidence and severity. Gut. 1995; 37:565–567.
Article14. Balani AR, Grendell JH. Drug-induced pancreatitis : incidence, management and prevention. Drug Saf. 2008; 31:823–837.15. Castiglione F, Del Vecchio Blanco G, Rispo A, Mazzacca G. Prevention of pancreatitis by weekly amylase assay in patients with Crohn's disease treated with azathioprine. Am J Gastroenterol. 2000; 95:2394–2395.
Article16. Foster RA, Zander DS, Mergo PJ, Valentine JF. Mesalamine-related lung disease: clinical, radiographic, and pathologic manifestations. Inflamm Bowel Dis. 2003; 9:308–315.
Article17. Camus P, Piard F, Ashcroft T, Gal AA, Colby TV. The lung in inflammatory bowel disease. Medicine (Baltimore). 1993; 72:151–183.
Article18. Rothfuss KS, Stange EF, Herrlinger KR. Extraintestinal manifestations and complications in inflammatory bowel diseases. World J Gastroenterol. 2006; 12:4819–4831.
Article19. Rutgeerts P, Sandborn WJ, Feagan BG, Reinisch W, Olson A, Johanns J, et al. Infliximab for induction and maintenance therapy for ulcerative colitis. N Engl J Med. 2005; 353:2462–2476.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Acute Pancreatitis Induced by Multiple Drugs in a Patient with Ulcerative Colitis
- A Case of Acute Pancreatitis associated with Ulcerative Colitis
- Type 2 Autoimmune Pancreatitis with Ulcerative Colitis Manifesting as Acute Pancreatitis
- A Case of Acute Pancreatitis Caused by 5-aminosalicylic Acid Suppositories in a Patient with Ulcerative Colitis
- Acute Pancreatitis Induced by 5-Aminosalicylic Acid in a Patient with Ulcerative Colitis