Intest Res.
2017 Jul;15(3):352-357. 10.5217/ir.2017.15.3.352.
Changes in serum levels of lipopolysaccharides and CD26 in patients with Crohn's disease
- Affiliations
-
- 1Department of Surgery, Faculty of Medical Sciences, State University of Campinas, Campinas, Brazil. danimagro@terra.com.br
- 2Colorectal Surgery Unit, Cajuru University Hospital, Catholic University of Paraná, Curitiba, Brazil.
- 3Department of Internal Medicine, Faculty of Medical Sciences, State University of Campinas, Campinas, Brazil.
- 4Research Laboratory of Metabolism and Diabetes, Gastrocentro, State University of Campinas, Campinas, Brazil.
- 5Faculty of Applied Sciences, State University of Campinas, Campinas, Brazil.
- KMID: 2382379
- DOI: http://doi.org/10.5217/ir.2017.15.3.352
Abstract
- BACKGROUND/AIMS
Lipopolysaccharide (LPS) is a molecule formed by lipids and polysaccharides and is the major cell wall component of gram-negative bacteria. High LPS levels are known to block CD26 expression by activating Toll-like receptor 4. The aim of this study was to correlate the serum levels of LPS and CD26 in Crohn's disease (CD) patients with serum levels of C-reactive protein (CRP), interleukins, CD activity index, and tumor necrosis factor-α (TNF-α).
METHODS
Serum samples were collected from 27 individuals (10 with active CD, 10 with inactive CD, and 7 controls) and the levels of LPS, CD26, TNF-α, interleukin-1β (IL-1β), IL-6, IL-17, and CRP were determined by enzyme-linked immunosorbent assay. The levels of LPS and CD26 were then tested for correlation with TNF-α, IL-1β, IL-6, IL-17, and CRP.
RESULTS
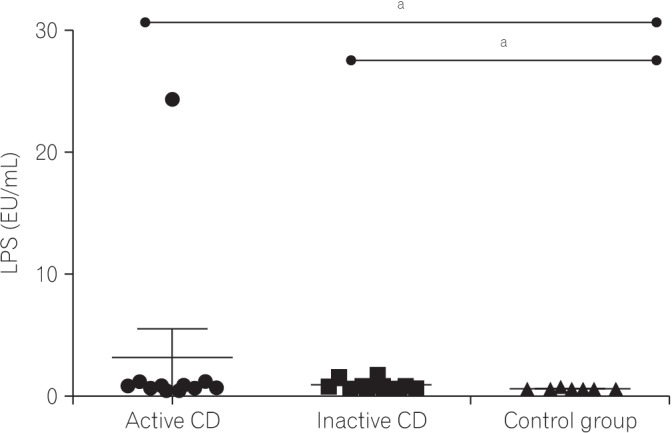
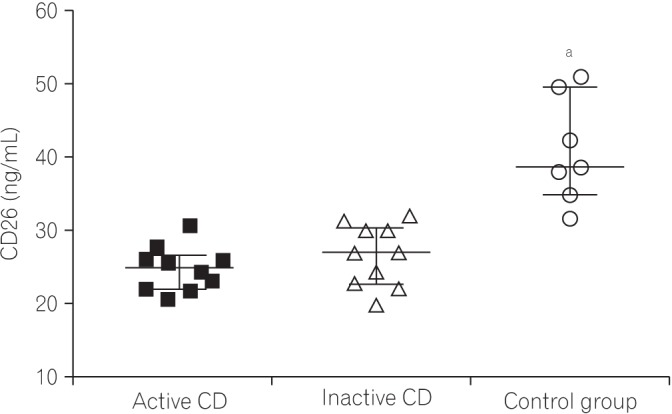
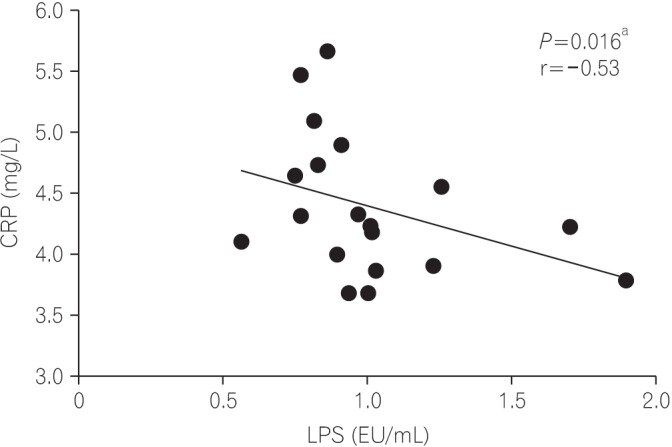
Serum levels of LPS were significantly elevated in the active CD group (P=0.003). Levels of IL-1β (P=0.002), IL-6 (P=0.003), and IL-17 (P<0.001) were lower in the CD groups. Serum TNF-α levels were increased in the active CD group. The CRP levels were elevated in the CD groups when compared to controls (P<0.001). The CD26 levels were lower in the CD groups than in the control group (P<0.001). Among the variables analyzed, there was a correlation between LPS and CRP (r=−0.53, P=0.016) in the CD groups.
CONCLUSIONS
Individuals with CD exhibited higher serum levels of LPS varying from a 2- to 6-fold increase depending on disease activity, when compared with healthy controls. CD26 levels were lower in the CD groups. Both LPS and CD26 correlated with disease severity and serve as potential CD biomarkers.
MeSH Terms
-
Biomarkers
C-Reactive Protein
Cell Wall
Crohn Disease*
Enzyme-Linked Immunosorbent Assay
Gram-Negative Bacteria
Humans
Inflammatory Bowel Diseases
Interleukin-17
Interleukin-6
Interleukins
Lipopolysaccharides*
Necrosis
Polysaccharides
Toll-Like Receptor 4
Biomarkers
C-Reactive Protein
Interleukin-17
Interleukin-6
Interleukins
Lipopolysaccharides
Polysaccharides
Toll-Like Receptor 4
Figure
Reference
-
1. Caricilli AM, Saad MJ. The role of gut microbiota on insulin resistance. Nutrients. 2013; 5:829–851. PMID: 23482058.
Article2. Sun Y, Shang D. Inhibitory effects of antimicrobial peptides on lipopolysaccharide-induced inflammation. Mediators Inflamm. 2015; 2015:167572. PMID: 26612970.3. Ikeda T, Kumagai E, Iwata S, Yamakawa A. Soluble CD26/dipeptidyl peptidase IV enhances the transcription of IL-6 and TNF-alpha in THP-1 cells and monocytes. PLoS One. 2013; 8:e66520. DOI: 10.1371/journal.pone.0066520. PMID: 23805228.4. Delzenne NM, Cani PD, Everard A, Neyrinck AM, Bindels LB. Gut microorganisms as promising targets for the management of type 2 diabetes. Diabetologia. 2015; 58:2206–2217. PMID: 26224102.5. Tsukumo DM, Carvalho BM, Carvalho Filho MA, Saad MJ. Translational research into gut microbiota: new horizons on obesity treatment: updated 2014. Arch Endocrinol Metab. 2015; 59:154–160. PMID: 25993679.6. Tsukahara T, Watanabe K, Watanabe T, et al. Tumor necrosis factor α decreases glucagon-like peptide-2 expression by upregulating G-protein-coupled receptor 120 in Crohn disease. Am J Pathol. 2015; 185:185–196. PMID: 25447053.7. Wellmann W, Fink PC, Benner F, Schmidt FW. Endotoxaemia in active Crohn's disease: treatment with whole gut irrigation and 5-aminosalicylic acid. Gut. 1986; 27:814–820. PMID: 3732891.
Article8. Gorrell MD, Gysbers V, McCaughan GW. CD26: a multifunctional integral membrane and secreted protein of activated lymphocytes. Scand J Immunol. 2001; 54:249–264. PMID: 11555388.
Article9. Busso N, Wagtmann N, Herling C, et al. Circulating CD26 is negatively associated with inflammation in human and experimental arthritis. Am J Pathol. 2005; 166:433–442. PMID: 15681827.
Article10. Moran GW, O'Neill C, Padfield P, McLaughlin JT. Dipeptidyl peptidase-4 expression is reduced in Crohn's disease. Regul Pept. 2012; 177:40–45. PMID: 22561447.
Article11. Hildebrandt M, Rose M, Rüter J, Salama A, Mönnikes H, Klapp BF. Dipeptidyl peptidase IV (DP IV, CD26) in patients with inflammatory bowel disease. Scand J Gastroenterol. 2001; 36:1067–1072. PMID: 11589380.
Article12. Best WR, Becktel JM, Singleton JW, Kern F Jr. Development of a Crohn's disease activity index: National Cooperative Crohn's Disease Study. Gastroenterology. 1976; 70:439–444. PMID: 1248701.13. Satsangi J, Silverberg MS, Vermeire S, Colombel JF. The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications. Gut. 2006; 55:749–753. PMID: 16698746.
Article14. Aoki K. A study of endotoxemia in ulcerative colitis and Crohn's disease. I: clinical study. Acta Med Okayama. 1978; 32:147–158. PMID: 150200.15. Guo Y, Zhou G, He C, Yang W, He Z, Liu Z. Serum levels of lipopolysaccharide and 1,3-beta-D-glucan refer to the severity in patients with Crohn's disease. Mediators Inflamm. 2015; 2015:843089. PMID: 26106258.16. Maloy KJ, Powrie F. Intestinal homeostasis and its breakdown in inflammatory bowel disease. Nature. 2011; 474:298–306. PMID: 21677746.
Article17. Rhee SH. Lipopolysaccharide: basic biochemistry, intracellular signaling, and physiological impacts in the gut. Intest Res. 2014; 12:90–95. PMID: 25349574.
Article18. Hölttä V, Klemetti P, Sipponen T, et al. IL-23/IL-17 immunity as a hallmark of Crohn's disease. Inflamm Bowel Dis. 2008; 14:1175–1184. PMID: 18512248.
Article19. Butler M, Boyle JJ, Powell JJ, Playford RJ, Ghosh S. Dietary microparticles implicated in Crohn's disease can impair macrophage phagocytic activity and act as adjuvants in the presence of bacterial stimuli. Inflamm Res. 2007; 56:353–361. PMID: 17878997.
Article20. Ott SJ, Musfeldt M, Wenderoth DF, et al. Reduction in diversity of the colonic mucosa associated bacterial microflora in patients with active inflammatory bowel disease. Gut. 2004; 53:685–693. PMID: 15082587.
Article21. Martinez-Medina M, Aldeguer X, Lopez-Siles M, et al. Molecular diversity of Escherichia coli in the human gut: new ecological evidence supporting the role of adherent-invasive E. coli (AIEC) in Crohn's disease. Inflamm Bowel Dis. 2009; 15:872–882. PMID: 19235912.
Article22. Sakamoto N, Kono S, Wakai K, et al. Dietary risk factors for inflammatory bowel disease: a multicenter case-control study in Japan. Inflamm Bowel Dis. 2005; 11:154–163. PMID: 15677909.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Age-Related CD26 Expression in Circulating T Cells in Peripheral Blood
- Primary hypertrophic osteoarthropathy accompanied by Crohn's disease: a case report
- The modification of the silver stain method in sodium dodecyl sulfatepolycarylamine gels for detecting lipopolysaccharides
- A case of Crohn disease
- Correlation of serum levels of anti-tumor necrosis factor agents with perianal fistula healing in Crohn’s disease: a narrative review