Ann Lab Med.
2016 Sep;36(5):420-426. 10.3343/alm.2016.36.5.420.
The Prognostic Value of Serum Levels of Heart-Type Fatty Acid Binding Protein and High Sensitivity C-Reactive Protein in Patients With Increased Levels of Amino-Terminal Pro-B Type Natriuretic Peptide
- Affiliations
-
- 1Department of Laboratory Medicine, Gachon University Gil Medical Center, Incheon, Korea. pwpark@gilhospital.com
- KMID: 2373571
- DOI: http://doi.org/10.3343/alm.2016.36.5.420
Abstract
- BACKGROUND
Amino-terminal pro-B type natriuretic peptide (NT-proBNP) is a well-established prognostic factor in heart failure (HF). However, numerous causes may lead to elevations in NT-proBNP, and thus, an increased NT-proBNP level alone is not sufficient to predict outcome. The aim of this study was to evaluate the utility of two acute response markers, high sensitivity C-reactive protein (hsCRP) and heart-type fatty acid binding protein (H-FABP), in patients with an increased NT-proBNP level.
METHODS
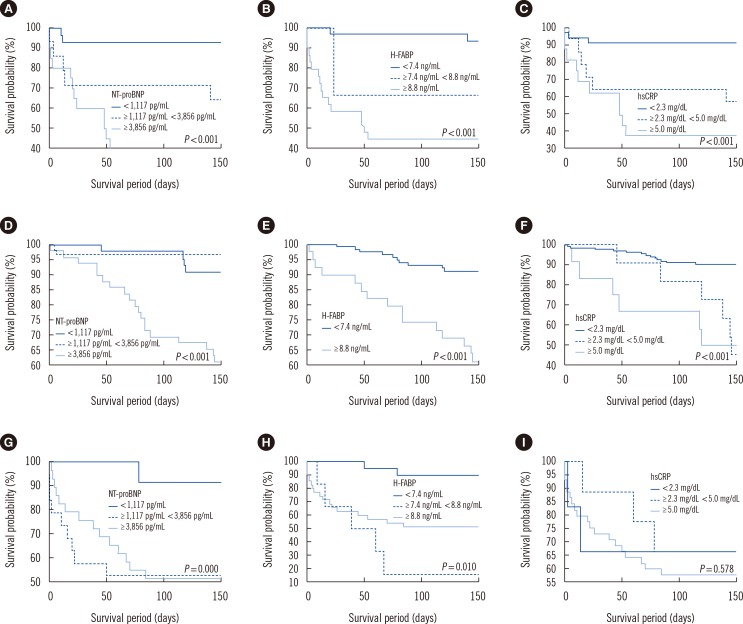
The 278 patients were classified into three groups by etiology: 1) acute coronary syndrome (ACS) (n=62), 2) non-ACS cardiac disease (n=156), and 3) infectious disease (n=60). Survival was determined on day 1, 7, 14, 21, 28, 60, 90, 120, and 150 after enrollment.
RESULTS
H-FABP (P<0.001), NT-proBNP (P=0.006), hsCRP (P<0.001) levels, and survival (P<0.001) were significantly different in the three disease groups. Patients were divided into three classes by using receiver operating characteristic curves for NT-proBNP, H-FABP, and hsCRP. Patients with elevated NT-proBNP (≥3,856 pg/mL) and H-FABP (≥8.8 ng/mL) levels were associated with higher hazard ratio for mortality (5.15 in NT-proBNP and 3.25 in H-FABP). Area under the receiver operating characteristic curve analysis showed H-FABP was a better predictor of 60-day mortality than NT-proBNP.
CONCLUSIONS
The combined measurement of H-FABP with NT-proBNP provides a highly reliable means of short-term mortality prediction for patients hospitalized for ACS, non-ACS cardiac disease, or infectious disease.
Keyword
MeSH Terms
-
Acute Coronary Syndrome/blood/*diagnosis/mortality
Aged
Area Under Curve
Biomarkers/blood
C-Reactive Protein/*analysis
Fatty Acid-Binding Proteins/*blood
Female
Humans
Kaplan-Meier Estimate
Male
Middle Aged
Natriuretic Peptide, Brain/*blood
Peptide Fragments/*blood
Prognosis
Proportional Hazards Models
ROC Curve
Biomarkers
C-Reactive Protein
Fatty Acid-Binding Proteins
Natriuretic Peptide, Brain
Peptide Fragments
Figure
Reference
-
1. Baggish AL, van Kimmenade RR, Januzzi JL Jr. Amino-terminal pro-B-type natriuretic peptide testing and prognosis in patients with acute dyspnea, including those with acute heart failure. Am J Cardiol. 2008; 101:49–55. PMID: 18243859.2. Doust JA, Glasziou PP, Pietrzak E, Dobson AJ. A systematic review of the diagnostic accuracy of natriuretic peptides for heart failure. Arch Intern Med. 2004; 164:1978–1984. PMID: 15477431.3. Mathewkutty S, Sethi SS, Aneja A, Shah K, Iyengar RL, Hermann L, et al. Biomarkers after risk stratification in acute chest pain (from the BRIC Study). Am J Cardiol. 2013; 111:493–498. PMID: 23218997.4. Christenson E, Christenson RH. The role of cardiac biomarkers in the diagnosis and management of patients presenting with suspected acute coronary syndrome. Ann Lab Med. 2013; 33:309–318. PMID: 24003420.5. Ray P, Delerme S, Jourdain P, Chenevier-Gobeaux C. Differential diagnosis of acute dyspnea: the value of B natriuretic peptides in the emergency department. QJM. 2008; 101:831–843. PMID: 18664534.6. Lindahl B. Acute coronary syndrome-the present and future role of biomarkers. Clin Chem Lab Med. 2013; 51:1699–1706. PMID: 23525876.7. Kim H, Yang DH, Park Y, Han J, Lee H, Kang H, et al. Incremental prognostic value of C-reactive protein and N-terminal proB-type natriuretic peptide in acute coronary syndrome. Circ J. 2006; 70:1379–1384. PMID: 17062957.8. Windram JD, Loh PH, Rigby AS, Hanning I, Clark AL, Cleland JG. Relationship of high-sensitivity C-reactive protein to prognosis and other prognostic markers in outpatients with heart failure. Am Heart J. 2007; 153:1048–1055. PMID: 17540208.9. Offner GD, Brecher P, Sawlivich WB, Costello CE, Troxler RF. Characterization and amino acid sequence of a fatty acid-binding protein from human heart. Biochem J. 1988; 252:191–198. PMID: 3421901.10. Glatz JF, van der Vusse GJ. Cellular fatty acid-binding proteins: their function and physiological significance. Prog Lipid Res. 1996; 35:243–282. PMID: 9082452.11. Lippi G, Mattiuzzi C, Cervellin G. Critical review and meta-analysis on the combination of heart-type fatty acid binding protein (H-FABP) and troponin for early diagnosis of acute myocardial infarction. Clin Biochem. 2013; 46:26–30. PMID: 23099200.12. Komamura K, Sasaki T, Hanatani A, Kim J, Hashimura K, Ishida Y, et al. Heart-type fatty acid binding protein is a novel prognostic marker in patients with non-ischaemic dilated cardiomyopathy. Heart. 2006; 92:615–618. PMID: 16387818.13. Liao J, Chan CP, Cheung YC, Lu JH, Luo Y, Cautherley GW, et al. Human heart-type fatty acid-binding protein for on-site diagnosis of early acute myocardial infarction. Int J Cardiol. 2009; 133:420–423. PMID: 18571749.14. Okamoto F, Sohmiya K, Ohkaru Y, Kawamura K, Asayama K, Kimura H, et al. Human heart-type cytoplasmic fatty acid-binding protein (H-FABP) for the diagnosis of acute myocardial infarction. Clinical evaluation of H-FABP in comparison with myoglobin and creatine kinase isoenzyme MB. Clin Chem Lab Med. 2000; 38:231–238. PMID: 10905760.15. DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988; 44:837–845. PMID: 3203132.16. Viswanathan K, Kilcullen N, Morrell C, Thistlethwaite SJ, Sivananthan MU, Hassan TB, et al. Heart-type fatty acid-binding protein predicts long-term mortality and re-infarction in consecutive patients with suspected acute coronary syndrome who are troponin-negative. J Am Coll Cardiol. 2010; 55:2590–2598. PMID: 20513600.17. Jo YH, Kim K, Lee JH, Rhee JE, Kang KW, Rim KP, et al. Heart-type fatty acid-binding protein as a prognostic factor in patients with severe sepsis and septic shock. Am J Emerg Med. 2012; 30:1749–1755. PMID: 22463971.18. Lagrand WK, Visser CA, Hermens WT, Niessen HW, Verheugt FW, Wolbink GJ, et al. C-reactive protein as a cardiovascular risk factor: more than an epiphenomenon? Circulation. 1999; 100:96–102. PMID: 10393687.19. Ridker PM. Clinical application of C-reactive protein for cardiovascular disease detection and prevention. Circulation. 2003; 107:363–369. PMID: 12551853.20. Silvestre J, Póvoa P, Coelho L, Almeida E, Moreira P, Fernandes A, et al. Is C-reactive protein a good prognostic marker in septic patients? Intensive Care Med. 2009; 35:909–913. PMID: 19169668.21. Müller B, Harbarth S, Stolz D, Bingisser R, Mueller C, Leuppi J, et al. Diagnostic and prognostic accuracy of clinical and laboratory parameters in community-acquired pneumonia. BMC Infect Dis. 2007; 7:10. PMID: 17335562.22. Krüger S, Ewig S, Marre R, Papassotiriou J, Richter K, von Baum H, et al. Procalcitonin predicts patients at low risk of death from community-acquired pneumonia across all CRB-65 classes. Eur Respir J. 2008; 31:349–355. PMID: 17959641.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Biomarkers in Heart Failure: Focus on B-type Natriuretic Peptide
- Effects of Super-Ultramarathon Races (622 km) on Cardiac Bio-Markers and Markers of Muscle Damage
- Serial Monitoring of B-Type Natriuretic Peptide in Heart Failure Patients
- Changes in N-terminal pro-B-type natriuretic peptide in a neonate with symptomatic isolated left ventricular noncompaction
- Clinical Implication of B-type Natriuretic Peptide in the Elderly