Increasing Resistance to Extended-Spectrum Cephalosporins, Fluoroquinolone, and Carbapenem in Gram-Negative Bacilli and the Emergence of Carbapenem Non-Susceptibility in Klebsiella pneumoniae: Analysis of Korean Antimicrobial Resistance Monitoring System (KARMS) Data From 2013 to 2015
- Affiliations
-
- 1Department of Laboratory Medicine and Research Institute of Bacterial Resistance, Yonsei University College of Medicine, Seoul, Korea. hmlee.labmed@gmail.com
- 2Department of Laboratory Medicine, Soonchunhyang University College of Medicine, Cheonan, Korea.
- 3Department of Laboratory Medicine, College of Medicine, Yeungnam University College of Medicine, Daegu, Korea.
- 4Department of Laboratory Medicine, Chosun University College of Medicine, Gwangju, Korea.
- KMID: 2369748
- DOI: http://doi.org/10.3343/alm.2017.37.3.231
Abstract
- BACKGROUND
National surveillance of antimicrobial resistance becomes more important for the control of antimicrobial resistance and determination of treatment guidelines. We analyzed Korean Antimicrobial Resistance Monitoring System (KARMS) data collected from 2013 to 2015.
METHODS
Of the KARMS participants, 16 secondary or tertiary hospitals consecutively reported antimicrobial resistance rates from 2013 to 2015. Data from duplicate isolates and institutions with fewer than 20 isolates were excluded. To determine the long-term trends, previous KARMS data from 2004 to 2012 were also considered.
RESULTS
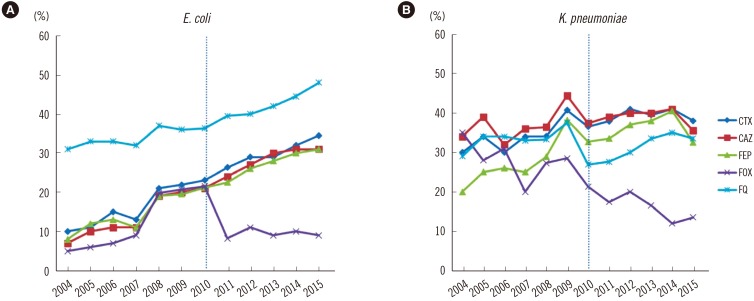
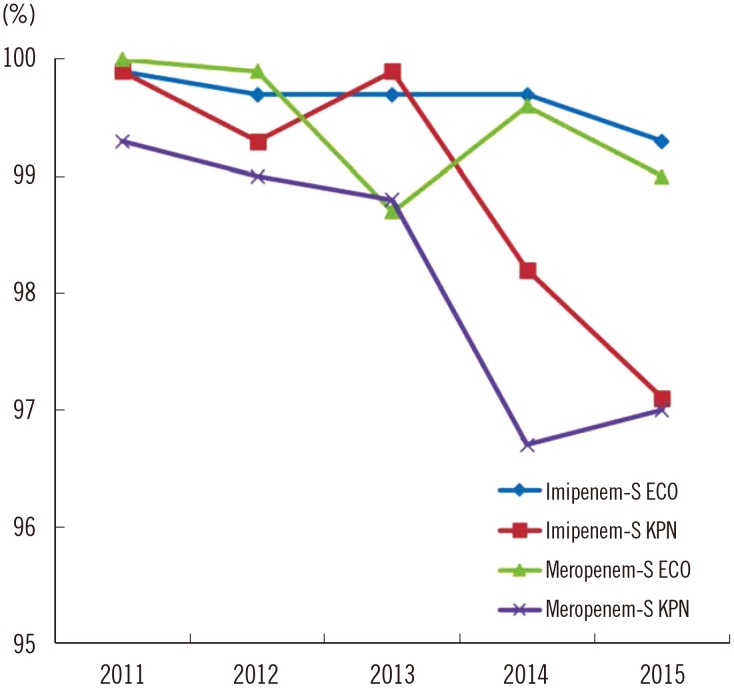
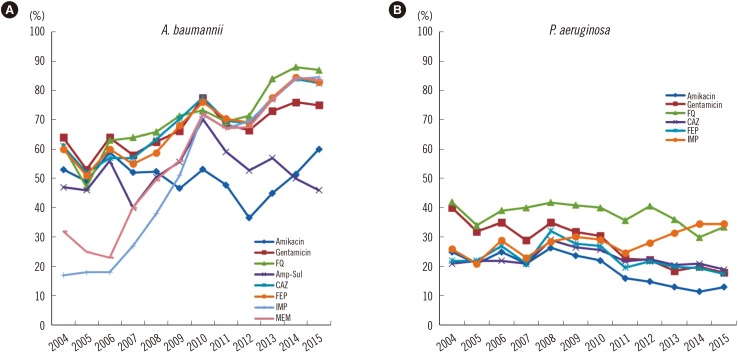
The prevalence of methicillin-resistant Staphylococcus aureus and vancomycin-resistant Enterococcus faecium from 2013 to 2015 was 66-72% and 29-31%, respectively. The resistance rates of Escherichia coli to cefotaxime and cefepime gradually increased to 35% and 31%, respectively, and fluoroquinolone resistance reached 48% in 2015. The resistance rates of Klebsiella pneumoniae to cefotaxime, cefepime, and carbapenem were 38-41%, 33-41%, and <0.1-2%, respectively, from 2013 to 2015. The carbapenem susceptibility rates of E. coli and K. pneumoniae decreased from 100% and 99.3% in 2011 to 99.0% and 97.0% in 2015, respectively. The resistance rate of Pseudomonas aeruginosa to carbapenem increased to 35% and the prevalence of carbapenem-resistant Acinetobacter baumannii increased from 77% in 2013 to 85% in 2015.
CONCLUSIONS
Between 2013 and 2015, the resistance rates of E. coli to third- and fourth-generation cephalosporins increased continuously, while carbapenem-susceptibility gradually decreased, particularly in K. pneumoniae. The prevalence of carbapenem-resistant P. aeruginosa and A. baumannii increased significantly; therefore, few treatment options remain for these resistant strains.
MeSH Terms
Figure
Cited by 5 articles
-
Colonization Prevalence and Risk Factor Analysis of Carbapenem-Resistant Acinetobacter baumannii in an Intensive Care Unit without Outbreaks
Young Ah Kim, Yoon Soo Park, Sang Sun Lee, Young Jun Son, Jeong Hwa Yeon, Young Hee Seo, Kyungwon Lee
Korean J Healthc Assoc Infect Control Prev. 2019;24(2):81-87. doi: 10.14192/kjicp.2019.24.2.81.Management of multi-drug resistant organisms in healthcare settings
Sun Hee Park
J Korean Med Assoc. 2018;61(1):26-35. doi: 10.5124/jkma.2018.61.1.26.The Changes in Epidemiology of Imipenem-Resistant
Acinetobacter baumannii Bacteremia in a Pediatric Intensive Care Unit for 17 Years
Dongsub Kim, Haejeong Lee, Joon-sik Choi, Christina M. Croney, Ki-Sup Park, Hyo Jung Park, Joongbum Cho, Sohee Son, Jin Yeong Kim, Soo-Han Choi, Hee Jae Huh, Kwan Soo Ko, Nam Yong Lee, Yae-Jean Kim
J Korean Med Sci. 2022;37(24):e196. doi: 10.3346/jkms.2022.37.e196.Microorganisms Isolated from Urine Cultures and Their Antimicrobial Susceptibility Patterns at a Commercial Laboratory during 2018-2020
Byeonghak Kwak, Jungmi Hong, Hye Gyung Bae, Yoon Soo Park, Mi Kyeong Lee, Kyungwon Lee, Kyoung Ryul Lee
Korean J Healthc Assoc Infect Control Prev. 2022;27(1):51-58. doi: 10.14192/kjicp.2022.27.1.51.Current Status and Prospects of the National Antimicrobial Resistance Surveillance System, Kor-GLASS
Dokyun Kim, Min Hyuk Choi, Jun Sung Hong, Jong Hee Shin, Seok Hoon Jeong
Korean J Healthc Assoc Infect Control Prev. 2022;27(2):96-103. doi: 10.14192/kjicp.2022.27.2.96.
Reference
-
1. Centers for Disease Control and Prevention. Antibiotic resistance threat in the United States, 2013. Atlanta, GA: Centers for Disease Control and Prevention, US Department of Health and Human Service;2013.2. Hong SG, Yong D, Lee K, Kim EC, Lee WK, Jeong SH, et al. Antimicrobial resistance of clinically important bacteria isolated from hospitals located in representative provinces of Korea. Korean J Clin Microbiol. 2003; 6:29–36.3. Lee K, Lee MA, Lee CH, Lee J, Roh KH, Kim S, et al. Increase of ceftazidime- and fluoroquinolone-resistant Klebsiella pneumoniae and imipenem-resistant Acinetobacter spp. in Korea: analysis of KONSAR study data from 2005 and 2007. Yonsei Med J. 2010; 51:901–911. PMID: 20879058.4. Lee K, Kim MN, Kim JS, Hong HL, Kang JO, Shin JH, et al. Further increases in carbapenem-, amikacin-, and fluoroquinolone-resistant isolates of Acinetobacter spp. and P. aeruginosa in Korea: KONSAR study 2009. Yonsei Med J. 2011; 52:793–802. PMID: 21786445.5. Lee Y, Kim BS, Chun J, Yong JH, Lee YS, Yoo JS, et al. Clonality and resistome analysis of KPC-producing Klebsiella pneumoniae strain isolated in Korea using whole genome sequencing. Biomed Res Int. 2014; 2014:352862. PMID: 25105122.6. O'Brien TF, Stelling JM. WHONET: removing obstacles to the full use of information about antimicrobial resistance. Diagn Microbiol Infect Dis. 1996; 25:162–168. PMID: 8937840.7. Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing. Twenty fourth Informational supplement, M100-S24. Wayne, PA: Clinical and Laboratory Standards Institute;2014.8. Lee H, Yong D, Lee K, Hong SG, Kim EC, Jeong SH, et al. Antimicrobial resistance of clinically important bacteria from 12 hospitals in Korea in 2004. Korean J Clin Microbiol. 2005; 8:66–73.9. Lee H, Kim CK, Lee J, Lee SH, Ahn JY, Hong SG, et al. Antimicrobial resistance of clinically important bacteria isolated from 12 hospitals in Korea in 2005 and 2006. Korean J Clin Microbiol. 2007; 10:59–69.10. Shibayama K, Lee H, Kim S. Comparison of antibiotic resistance rate of medically important microorganisms between Japan and Korea. Ann Clin Microbiol. 2015; 18:111–118.11. European Centre for Disease Prevention and Control. Antimicrobial resistance surveillance in Europe 2014. Solna, Sweden: 2015;http://ecdc.europa.eu/en/.12. Ministry of Health, Labour and Welfare. Japan Nosocomial Infections Surveillance (JANIS); Annual Open Report. 2014. http://www.nih-janis.jp/.13. Barnes SL, Morgan DJ, Harris AD, Carling PC, Thom KA. Preventing the transmission of multidrug-resistant organisms: modeling the relative importance of hand hygiene and environmental cleaning interventions. Infect Control Hosp Epidemiol. 2014; 35:1156–1162. PMID: 25111924.14. Kim MK, Nam EY, Na SH, Shin MJ, Lee HS, Kim NH, et al. Discrepancy in perceptions regarding patient participation in hand hygiene between patients and health care workers. Am J Infect Control. 2015; 43:510–515. PMID: 25752956.15. Choi SH, Chung JW, Sung H, Kim MN, Kim SH, Lee SO, et al. Impact of penicillin nonsusceptibility on clinical outcomes of patients with nonmeningeal Streptococcus pneumoniae bacteremia in the era of the 2008 clinical and laboratory standards institute penicillin breakpoints. Antimicrob Agents Chemother. 2012; 56:4650–4655. PMID: 22687517.16. Kim HI, Kim SW, Chang HH, Lee JM, Peck KR. A 2011-2012 survey of doctors' perceptions of korean guidelines and empirical treatment of community-acquired pneumonia. Infect Chemother. 2013; 45:394–405. PMID: 24475353.17. Park KS, Kim MH, Park TS, Suh JT, Lee HJ. Antimicrobial resistance of enterococcal isolates from blood and risk factors for vancomycin resistant enterococcal bacteremia in a tertiary care university hospital from 2003 to 2007. Korean J Clin Microbiol. 2010; 13:59–67.18. Kang CI, Song JH, Kim SH, Chung DR, Peck KR, So TM, et al. Risk factors for levofloxacin-nonsusceptible Streptococcus pneumoniae in community-acquired pneumococcal pneumonia: a nested case-control study. Eur J Clin Microbiol Infect Dis. 2014; 33:55–59. PMID: 24062235.19. Jung MK, Ahn SH, Lee WG, Lee EH. Molecular epidemiology of vancomycin-resistant enterococci isolated from non-tertiary-care and tertiary-care hospitals in Korea. Epidemiol Infect. 2014; 142:2372–2377. PMID: 25267406.20. Boucher HW, Sakoulas G. Perspectives on Daptomycin resistance, with emphasis on resistance in Staphylococcus aureus. Clin Infect Dis. 2007; 45:601–608. PMID: 17682996.21. Park SH, Byun JH, Choi SM, Lee DG, Kim SH, Kwon JC, et al. Molecular epidemiology of extended-spectrum β-lactamase-producing Escherichia coli in the community and hospital in Korea: emergence of ST131 producing CTX-M-15. BMC Infect Dis. 2012; 12:149. PMID: 22747570.22. Jeon JH, Kim K, Han WD, Song SH, Park KU, Rhee JE, et al. Empirical use of ciprofloxacin for acute uncomplicated pyelonephritis caused by Escherichia coli in communities where the prevalence of fluoroquinolone resistance is high. Antimicrob Agents Chemother. 2012; 56:3043–3046. PMID: 22391544.23. Jacoby GA. Mechanisms of resistance to quinolones. Clin Infect Dis. 2005; 41(S2):S120–S126. PMID: 15942878.24. Yang HY, Nam YS, Lee HJ. Prevalence of plasmid-mediated quinolone resistance genes among ciprofloxacin-nonsusceptible Escherichia coli and Klebsiella pneumonia isolated from blood cultures in Korea. Can J Infect Dis Med Microbiol. 2014; 25:163–169. PMID: 25285114.25. Lee K, Lee M, Shin JH, Lee MH, Kang SH, Park AJ, et al. Prevalence of plasmid-mediated AmpC beta-lactamases in Escherichia coli and Klebsiella pneumoniae in Korea. Microb Drug Resist. 2006; 12:44–49. PMID: 16584308.26. Seok Y, Bae IK, Jeong SH, Kim SH, Lee H, Lee K. Dissemination of IMP-6 metallo-β-lactamase-producing Pseudomonas aeruginosa sequence type 235 in Korea. J Antimicrob Chemother. 2011; 66:2791–2796. PMID: 21933788.27. Yong D, Choi YS, Roh KH, Kim CK, Park YH, Yum JH, et al. Increasing prevalence and diversity of metallo-beta-lactamases in Pseudomonas spp., Acinetobacter spp., and Enterobacteriaceae from Korea. Antimicrob Agents Chemother. 2006; 50:1884–1886. PMID: 16641469.28. Yano H, Kuga A, Okamoto R, Kitasato H, Kobayashi T, Inoue M. Plasmid-encoded metallo-beta-lactamase (IMP-6) conferring resistance to carbapenems, especially meropenem. Antimicrob Agents Chemother. 2001; 45:1343–1348. PMID: 11302793.29. Lee Y, Kim YR, Kim J, Park YJ, Song W, Shin JH, et al. Increasing prevalence of blaOXA-23-carrying Acinetobacter baumannii and the emergence of blaOXA-182-carrying Acinetobacter nosocomialis in Korea. Diagn Microbiol Infect Dis. 2013; 77:160–163. PMID: 23891219.30. Kuo LC, Lai CC, Liao CH, Hsu CK, Chang YL, Chang CY, et al. Multidrug-resistant Acinetobacter baumannii bacteraemia: clinical features, antimicrobial therapy and outcome. Clin Microbiol Infect. 2007; 13:196–198. PMID: 17328733.31. Prasad P, Sun J, Danner RL, Natanson C. Excess deaths associated with tigecycline after approval based on noninferiority trials. Clin Infect Dis. 2012; 54:1699–1709. PMID: 22467668.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Antimicrobial Therapy for Infections Caused by Carbapenem-Resistant Gram-Negative Bacteria
- The Impact of Antibiotic Burden on the Selective Resistance of Gram Negative Bacteria in Children
- The Impact of the Antibiotic Burden on the Selection of its Resistance among Gram Negative Bacteria Isolated from Children
- Trend of Bacterial Resistance for the Past 50 Years in Korea and Future Perspectives - Gram-negative Bacteria
- Antibiotics for multidrug-resistant gram-negative bacteria