Pediatr Gastroenterol Hepatol Nutr.
2016 Sep;19(3):153-161. 10.5223/pghn.2016.19.3.153.
Middle East Consensus Statement on the Diagnosis and Management of Functional Gastrointestinal Disorders in <12 Months Old Infants
- Affiliations
-
- 1Department of Pediatrics, Universitair Ziekenhuis Brussel, Vrije Universiteit Brussel, Brussels, Belgium. yvan.vandenplas@uzbrussel.be
- 2Department of Pediatrics, King Salman Hospital, Riyadh, Saudi Arabia.
- 3Faculty of Medicine, Kuwait University, Kuwait City, Kuwait.
- 4Department of Pediatrics, Al Adan Hospital, Kuwait City, Kuwait.
- 5Department of Pediatric Gastroentrology, Hepatology and Pediatric Nutrition, St. Joseph Hospital, Beirut, Lebanon.
- 6Department of Pediatric Gastroenterology, Hotel Dieu de France, Beirut, Lebanon.
- 7Department of Pediatrics, Cairo University, Cairo, Egypt.
- 8Department of Pediatric Gastroenterology, King Faisal Specialist Hospital and Research Center, Ryiadh, Saudi Arabia.
- 9Department of Pediatric Gastroenterology, St. Georges Orthodox, Beirut, Lebanon.
- KMID: 2364773
- DOI: http://doi.org/10.5223/pghn.2016.19.3.153
Abstract
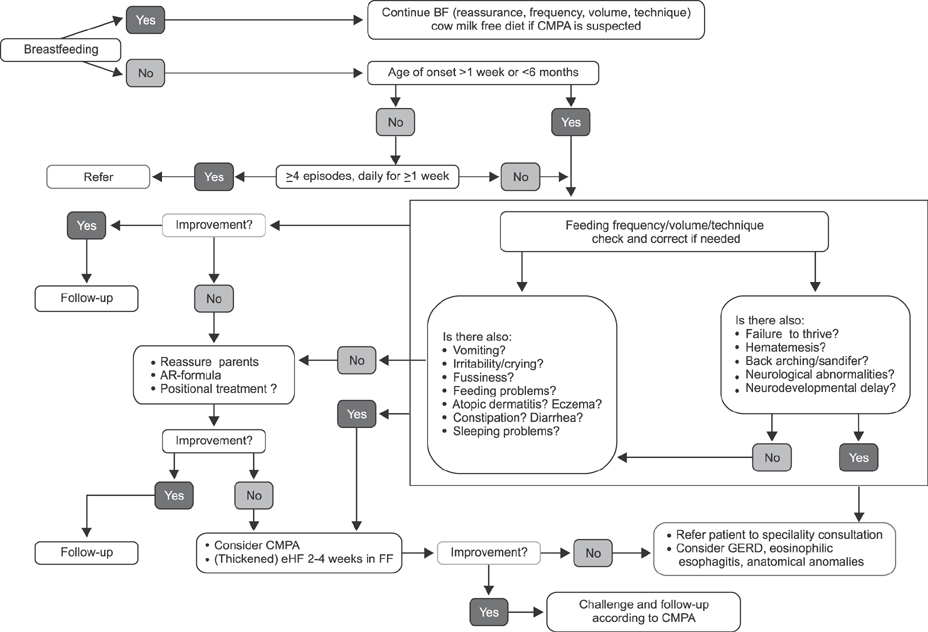
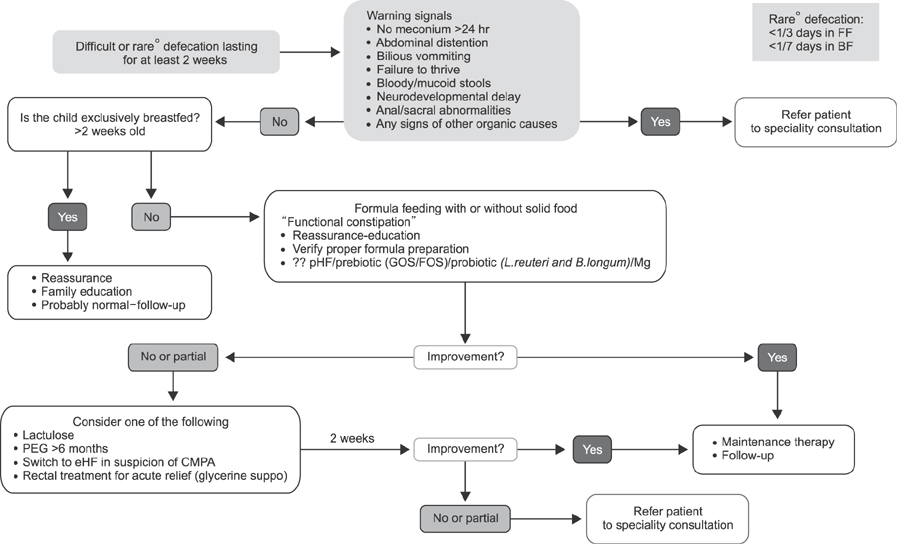
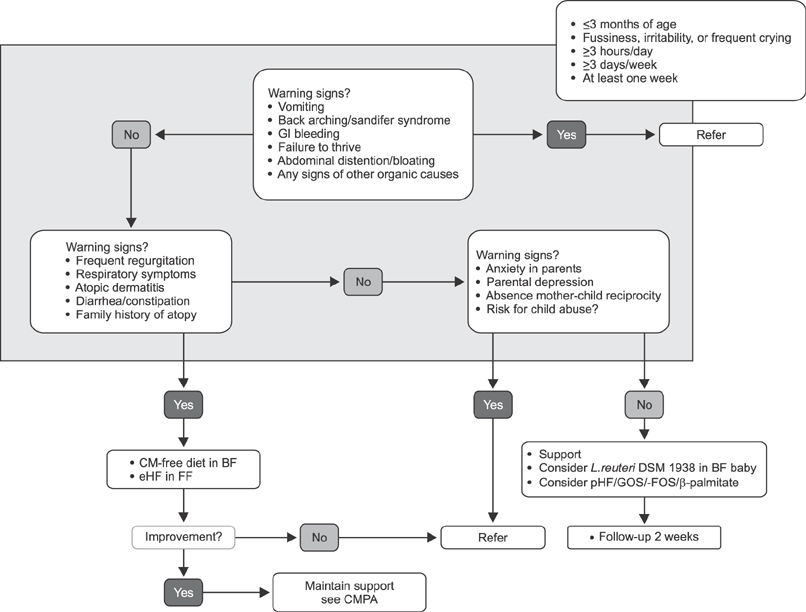
- This paper covers algorithms for the management of regurgitation, constipation and infantile colic in infants. Anti-regurgitation formula may be considered in infants with troublesome regurgitation, while diagnostic investigations or drug therapy are not indicated in the absence of warning signs. Although probiotics have shown some positive evidence for the management of functional gastrointestinal disorders (FGIDs), the evidence is not strong enough to make a recommendation. A partially hydrolyzed infant formula with prebiotics and β-palmitate may be considered as a dietary intervention for functional constipation in formula fed infants. Lactulose has been shown to be effective and safe in infants younger than 6 months that are constipated. Macrogol (polyethylene glycol, PEG) is not approved for use in infants less than 6 months of age. However, PEG is preferred over lactulose in infants >6 months of age. Limited data suggests that infant formula with a partial hydrolysate, galacto-oligosaccharides/fructo-oligosaccharides, added β-palmitate may be of benefit in reducing infantile colic in formula fed infants in cases where cow's milk protein allergy (CMPA) is not suspected. Evidence suggests that the use of extensively hydrolyzed infant formula for a formula-fed baby and a cow's milk free diet for a breastfeeding mother may be beneficial to decrease infantile colic if CMPA is suspected. None of the FGIDs is a reason to stop breastfeeding.
Keyword
MeSH Terms
Figure
Reference
-
1. Vandenplas Y, Abkari A, Bellaiche M, Benninga M, Chouraqui JP, Çokura F, et al. Prevalence and health outcomes of functional gastrointestinal symptoms in infants from birth to 12 months of age. J Pediatr Gastroenterol Nutr. 2015; 61:531–537.
Article2. Vandenplas Y, Ludwig T, van Elburg R, Bouritius H, Huet F. Association of infantile colic and functional gastrointestinal disorders and symptoms. In : ESPGHAN 48th Annual Meeting of the European Society for Paediatric Gastroenterology, Hepatology and Nutrition; 2015 May 6-9; Amsterdam, The Netherlands. PO-G-016.3. Vandenplas Y, Dupont C, Eigenmann P, Host A, Kuitunen M, Ribes-Koninckx C, et al. A workshop report on the development of the cow's milk-related symptom score awareness tool for young children. Acta Paediatr. 2015; 104:334–339.
Article4. McMurray AR. Three decision-making aids: brainstorming, nominal group, and Delphi technique. J Nurs Staff Dev. 1994; 10:62–65.5. Vandenplas Y, Rudolph CD, Di Lorenzo C, Hassall E, Liptak G, Mazur L, et al. Pediatric gastroesophageal reflux clinical practice guidelines: joint recommendations of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN). J Pediatr Gastroenterol Nutr. 2009; 49:498–547.
Article6. Alfaleh K, Alluwaimi E, Aljefri S, Alosaimi A, Behaisi M. Infant formula in Saudi Arabia: a cross sectional survey. Kuwaiti Med J. 2014; 46:328–332.7. Moro G, Minoli I, Mosca M, Fanaro S, Jelinek J, Stahl B, et al. Dosage-related bifidogenic effects of galacto- and fructooligosaccharides in formula-fed term infants. J Pediatr Gastroenterol Nutr. 2002; 34:291–295.
Article8. Moro GE, Boehm G. Clinical outcomes of prebiotic intervention trials during infancy: a review. Funct Food Rev. 2012; 4:101–113.9. Vandenplas Y, Alarcon P, Alliet P, De Greef E, De Ronne N, Hoffman I, et al. Algorithms for managing infant constipation, colic, regurgitation and cow's milk allergy in formula-fed infants. Acta Paediatr. 2015; 104:449–457.
Article10. Vandenplas Y, Gutierrez-Castrellon P, Velasco-Benitez C, Palacios J, Jaen D, Ribeiro H, et al. Practical algorithms for managing common gastrointestinal symptoms in infants. Nutrition. 2013; 29:184–194.
Article11. Coccorullo P, Strisciuglio C, Martinelli M, Miele E, Greco L, Staiano A. Lactobacillus reuteri (DSM 17938) in infants with functional chronic constipation: a double-blind, randomized, placebo-controlled study. J Pediatr. 2010; 157:598–602.
Article12. Indrio F, Di Mauro A, Riezzo G, Civardi E, Intini C, Corvaglia L, et al. Prophylactic use of a probiotic in the prevention of colic, regurgitation, and functional constipation: a randomized clinical trial. JAMA Pediatr. 2014; 168:228–233.
Article13. Bongers ME, de Lorijn F, Reitsma JB, Groeneweg M, Taminiau JA, Benninga MA. The clinical effect of a new infant formula in term infants with constipation: a double-blind, randomized cross-over trial. Nutr J. 2007; 6:8.
Article14. Savino F, Cresi F, Maccario S, Cavallo F, Dalmasso P, Fanaro S, et al. "Minor" feeding problems during the first months of life: effect of a partially hydrolysed milk formula containing fructo- and galacto-oligosaccharides. Acta Paediatr Suppl. 2003; 91:86–90.
Article15. Ali AM. Helicobacter pylori and infantile colic. Arch Pediatr Adolesc Med. 2012; 166:648–650.
Article16. Ali ASA, Elhady MAA. Prevalence and risk factors for infantile colic in Egyptian infants. J Am Sci. 2013; 9:340–343.17. Schreck Bird A, Gregory PJ, Jalloh MA, Risoldi Cochrane Z, Hein DJ. Probiotics for the treatment of infantile colic: a systematic review. J Pharm Pract. 2016; pii: 0897190016634516. [Epub ahead of print].
Article18. Harb T, Matsuyama M, David M, Hill RJ. Infant colic-what works: a systematic review of interventions for breast-fed infants. J Pediatr Gastroenterol Nutr. 2016; 62:668–686.19. Xu M, Wang J, Wang N, Sun F, Wang L, Liu XH. The efficacy and safety of the probiotic bacterium lactobacillus reuteri dsm 17938 for infantile colic: a meta-analysis of randomized controlled trials. PLoS One. 2015; 10:e0141445.
Article20. Chau K, Lau E, Greenberg S, Jacobson S, Yazdani-Brojeni P, Verma N, et al. Probiotics for infantile colic: a randomized, double-blind, placebo-controlled trial investigating Lactobacillus reuteri DSM 17938. J Pediatr. 2015; 166:74–78.
Article21. Savino F, Cordisco L, Tarasco V, Palumeri E, Calabrese R, Oggero R, et al. Lactobacillus reuteri DSM 17938 in infantile colic: a randomized, double-blind, placebo-controlled trial. Pediatrics. 2010; 126:e526–e533.
Article22. Savino F, Palumeri E, Castagno E, Cresi F, Dalmasso P, Cavallo F, et al. Reduction of crying episodes owing to infantile colic: A randomized controlled study on the efficacy of a new infant formula. Eur J Clin Nutr. 2006; 60:1304–1310.
Article23. van de Heijning BJ, Berton A, Bouritius H, Goulet O. GI symptoms in infants are a potential target for fermented infant milk formulae: a review. Nutrients. 2014; 6:3942–3967.
Article24. Kearney PJ, Malone AJ, Hayes T, Cole M, Hyland M. A trial of lactase in the management of infant colic. J Hum Nutr Diet. 1998; 11:281–285.
Article25. Kanabar D, Randhawa M, Clayton P. Improvement of symptoms in infant colic following reduction of lactose load with lactase. J Hum Nutr Diet. 2001; 14:359–363.
Article26. Vandenplas Y, Benninga M, Broekaert I, Falconer J, Gottrand F, Guarino A, et al. Functional gastro-intestinal disorder algorithms focus on early recognition, parental reassurance and nutritional strategies. Acta Paediatr. 2016; 105:244–252.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Correction: Middle East Consensus Statement on the Prevention, Diagnosis, and Management of Cow's Milk Protein Allergy
- Correction: Middle East Consensus Statement on the Diagnosis and Management of Functional Gastrointestinal Disorders in <12 Months Old Infants
- The New Rome IV Criteria for Functional Gastrointestinal Disorders in Infants and Toddlers
- Regional differences in diagnosis and management of cow's milk allergy
- Validation of Rome III Criteria in the Diagnosis of Functional Gastrointestinal Disorders in Korean Patients