Pediatr Gastroenterol Hepatol Nutr.
2017 Mar;20(1):1-13. 10.5223/pghn.2017.20.1.1.
The New Rome IV Criteria for Functional Gastrointestinal Disorders in Infants and Toddlers
- Affiliations
-
- 1Department of Pediatric Gastroenterology and Nutrition, Emma Children's Hospital/Academic Medical Center, Amsterdam, The Netherlands. j.zeevenhooven@amc.uva.nl
- KMID: 2375272
- DOI: http://doi.org/10.5223/pghn.2017.20.1.1
Abstract
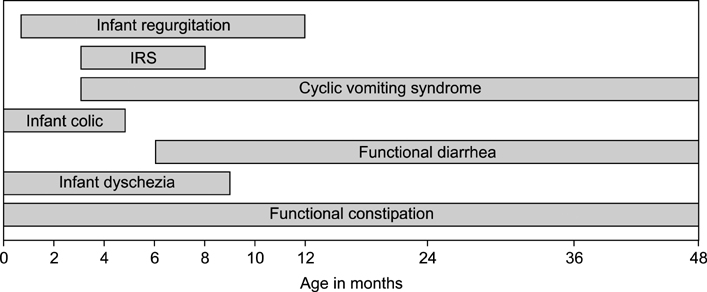
- Functional gastrointestinal disorders (FGIDs) are common worldwide and cover a wide range of disorders attributable to the gastrointestinal tract that cannot be explained by structural or biochemical abnormalities. The diagnosis of these disorders relies on the symptom-based Rome criteria. In 2016 the Rome criteria were revised for infants/toddlers and for children and adolescents. In this review, we discuss the novel Rome IV criteria for infants and toddlers. The criteria for infant colic were drastically changed, whereas only minor changes were made for regurgitation, cyclic vomiting syndrome, functional diarrhea, infant dyschezia and functional constipation. In addition to this, the new Rome IV discusses underlying mechanisms of pain in infants and toddlers, including the neuro-development of nociceptive and pain pathways, the various factors that are involved in pain experience, and methods of pain assessment in infants and toddlers is essential for the clinician who encounters functional pain in this age group. Overall, the Rome IV criteria have become more distinctive for all disorders in order to improve the process of diagnosing pediatric FGIDs.
MeSH Terms
Figure
Cited by 1 articles
-
Laxative Choice and Treatment Outcomes in Childhood Constipation: Clinical Data in a Longitudinal Retrospective Study
Atchariya Chanpong, Seksit Osatakul
Pediatr Gastroenterol Hepatol Nutr. 2018;21(2):101-110. doi: 10.5223/pghn.2018.21.2.101.
Reference
-
1. Benninga MA, Faure C, Hyman PE, St James Roberts I, Schechter NL, Nurko S. Childhood functional gastrointestinal disorders: neonate/toddler. Gastroenterology. 2016; 150:1443–1455.e2.
Article2. Drossman DA. Functional gastrointestinal disorders: history, pathophysiology, clinical features and Rome IV. Gastroenterology. 2016; 150:1262–1279.e2.
Article3. Rasquin-Weber A, Hyman PE, Cucchiara S, Fleisher DR, Hyams JS, Milla PJ, et al. Childhood functional gastrointestinal disorders. Gut. 1999; 45:Suppl 2. II60–II68.
Article4. Drossman DA. The functional gastrointestinal disorders and the Rome III process. Gastroenterology. 2006; 130:1377–1390.
Article5. Hyman PE, Milla PJ, Benninga MA, Davidson GP, Fleisher DF, Taminiau J. Childhood functional gastrointestinal disorders: neonate/toddler. Gastroenterology. 2006; 130:1519–1526.
Article6. Rasquin A, Di Lorenzo C, Forbes D, Guiraldes E, Hyams JS, Staiano A, et al. Childhood functional gastrointestinal disorders: child/adolescent. Gastroenterology. 2006; 130:1527–1537.
Article7. Ferreira-Maia AP, Matijasevich A, Wang YP. Epidemiology of functional gastrointestinal disorders in infants and toddlers: a systematic review. World J Gastroenterol. 2016; 22:6547–6558.
Article8. van Tilburg MA, Hyman PE, Walker L, Rouster A, Palsson OS, Kim SM, et al. Prevalence of functional gastrointestinal disorders in infants and toddlers. J Pediatr. 2015; 166:684–689.
Article9. Chogle A, Velasco-Benitez CA, Koppen IJ, Moreno JE, Ramírez Hernández CR, Saps M. A population-based study on the epidemiology of functional gastrointestinal disorders in young children. J Pediatr. 2016; 179:139–143.e1.
Article10. Osatakul S, Sriplung H, Puetpaiboon A, Junjana CO, Chamnongpakdi S. Prevalence and natural course of gastroesophageal reflux symptoms: a 1-year cohort study in Thai infants. J Pediatr Gastroenterol Nutr. 2002; 34:63–67.
Article11. Nelson SP, Chen EH, Syniar GM, Christoffel KK. Pediatric Practice Research Group. Prevalence of symptoms of gastroesophageal reflux during infancy. A pediatric practice-based survey. Arch Pediatr Adolesc Med. 1997; 151:569–572.
Article12. Vandenplas Y, Abkari A, Bellaiche M, Benninga M, Chouraqui JP, Çokura F, et al. Prevalence and health outcomes of functional gastrointestinal symptoms in infants from birth to 12 months of age. J Pediatr Gastroenterol Nutr. 2015; 61:531–537.
Article13. Vandenplas Y, Rudolph CD, Di Lorenzo C, Hassall E, Liptak G, Mazur L, et al. Pediatric gastroesophageal reflux clinical practice guidelines: joint recommendations of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN). J Pediatr Gastroenterol Nutr. 2009; 49:498–547.
Article14. Horvath A, Dziechciarz P, Szajewska H. The effect of thickened-feed interventions on gastroesophageal reflux in infants: systematic review and meta-analysis of randomized, controlled trials. Pediatrics. 2008; 122:e1268–e1277.
Article15. Vandenplas Y, Leluyer B, Cazaubiel M, Housez B, Bocquet A. Double-blind comparative trial with 2 antiregurgitation formulae. J Pediatr Gastroenterol Nutr. 2013; 57:389–393.
Article16. van Wijk MP, Benninga MA, Davidson GP, Haslam R, Omari TI. Small volumes of feed can trigger transient lower esophageal sphincter relaxation and gastroesophageal reflux in the right lateral position in infants. J Pediatr. 2010; 156:744–748.e1.
Article17. Task Force on Sudden Infant Death Syndrome. Moon RY. SIDS and other sleep-related infant deaths: expansion of recommendations for a safe infant sleeping environment. Pediatrics. 2011; 128:e1341–e1367.
Article18. Fleisher DR. Infant rumination syndrome: report of a case and review of the literature. Am J Dis Child. 1979; 133:266–269.19. Fleisher DR, Matar M. The cyclic vomiting syndrome: a report of 71 cases and literature review. J Pediatr Gastroenterol Nutr. 1993; 17:361–369.20. Li BU, Lefevre F, Chelimsky GG, Boles RG, Nelson SP, Lewis DW, et al. North american society for pediatric gastroenterology, hepatology, and nutrition consensus statement on the diagnosis and management of cyclic vomiting syndrome. J Pediatr Gastroenterol Nutr. 2008; 47:379–393.
Article21. Headache Classification Committee of the International Headache Society (IHS). The international classification of headache disorders, 3rd edition (beta version). Cephalalgia. 2013; 33:629–808.22. Saps M, Adams P, Bonilla S, Chogle A, Nichols-Vinueza D. Parental report of abdominal pain and abdominal pain-related functional gastrointestinal disorders from a community survey. J Pediatr Gastroenterol Nutr. 2012; 55:707–710.
Article23. Saps M, Nichols-Vinueza DX, Rosen JM, Velasco-Benítez CA. Prevalence of functional gastrointestinal disorders in Colombian school children. J Pediatr. 2014; 164:542–545.e1.24. Devanarayana NM, Adhikari C, Pannala W, Rajindrajith S. Prevalence of functional gastrointestinal diseases in a cohort of Sri Lankan adolescents: comparison between Rome II and Rome III criteria. J Trop Pediatr. 2011; 57:34–39.
Article25. Lewis ML, Palsson OS, Whitehead WE, van Tilburg MA. Prevalence of functional gastrointestinal disorders in children and adolescents. J Pediatr. 2016; 177:39–43.e3.26. Steutel NF, Benninga MA, Langendam MW, de Kruijff I, Tabbers MM. Reporting outcome measures in trials of infant colic. J Pediatr Gastroenterol Nutr. 2014; 59:341–346.
Article27. Lucassen PL, Assendelft WJ, van Eijk JT, Gubbels JW, Douwes AC, van Geldrop WJ. Systematic review of the occurrence of infantile colic in the community. Arch Dis Child. 2001; 84:398–403.28. James-Roberts IS, Conroy S, Wilsher K. Clinical, developmental and social aspects of infant crying and colic. Infant Child Dev. 1995; 4:177–189.
Article29. St James-Roberts I, Halil T. Infant crying patterns in the first year: normal community and clinical findings. J Child Psychol Psychiatry. 1991; 32:951–968.
Article30. Rautava P, Helenius H, Lehtonen L. Psychosocial predisposing factors for infantile colic. BMJ. 1993; 307:600–604.
Article31. Wolke D. Behavioural treatment of prolonged infant crying: evaluation, methods, and a proposal. In : Barr RG, St James-Roberts I, Keefe MR, editors. New evidence on unexplained early infant crying: its origins, nature and management. Skillman, NJ: Johnson & Johnson Pediatric Institute;2001. p. 187–208.32. Barr RG, St. James-Roberts I, Keefe MR. New evidence on unexplained early infant crying: its origins, nature and management. Skillman, NJ: Johnson & Johnson Pediatric Institute;2001.33. Treem WR. Infant colic. A pediatric gastroenterologist's perspective. Pediatr Clin North Am. 1994; 41:1121–1138.
Article34. Treem WR. Assessing crying complaints: the interaction with gastroesophageal reflux and cow's milk protein intolerance. New evidence on unexplained early infant crying: its origins, nature and management. Skillman, NJ: Johnson & Johnson Pediatric Institute;2001. p. 165–176.35. Shamir R. Infant colic and functional gastrointestinal disorders: is there more than a “gut feeling”? J Pediatr Gastroenterol Nutr. 2013; 57:S1–S2.36. Barr RG, Young SN, Wright JH, Gravel R, Alkawaf R. Differential calming responses to sucrose taste in crying infants with and without colic. Pediatrics. 1999; 103:e68.37. Lester BM, Boukydis CZ, Garcia-Coll CT, Hole WT. Colic for developmentalists. Infant Ment Health J. 1990; 11:321–333.
Article38. DeSantis A, Coster W, Bigsby R, Lester B. Colic and fussing in infancy, and sensory processing at 3 to 8 years of age. Infant Ment Health J. 2004; 25:522–539.
Article39. Milidou I, Søndergaard C, Jensen MS, Olsen J, Henriksen TB. Gestational age, small for gestational age, and infantile colic. Paediatr Perinat Epidemiol. 2014; 28:138–145.
Article40. Douglas P, Hill P. Managing infants who cry excessively in the first few months of life. BMJ. 2011; 343:d7772.
Article41. Talge NM, Neal C, Glover V. Early Stress, Translational Research and Prevention Science Network: Fetal and Neonatal Experience on Child and Adolescent Mental Health. Antenatal maternal stress and longterm effects on child neurodevelopment: how and why? J Child Psychol Psychiatry. 2007; 48:245–261.
Article42. van den Berg MP, van der Ende J, Crijnen AA, Jaddoe VW, Moll HA, Mackenbach JP, et al. Paternal depressive symptoms during pregnancy are related to excessive infant crying. Pediatrics. 2009; 124:e96–e103.
Article43. Indrio F, Riezzo G, Raimondi F, Di Mauro A, Francavilla R. Gut motility alterations in neonates and young infants. J Pediatr Gastroenterol Nutr. 2013; 57:S9–S11.
Article44. Gupta SK. Is colic a gastrointestinal disorder? Curr Opin Pediatr. 2002; 14:588–592.
Article45. Rhoads JM, Fatheree NY, Norori J, Liu Y, Lucke JF, Tyson JE, et al. Altered fecal microflora and increased fecal calprotectin in infants with colic. J Pediatr. 2009; 155:823–828.e1.
Article46. de Weerth C, Fuentes S, Puylaert P, de Vos WM. Intestinal microbiota of infants with colic: development and specific signatures. Pediatrics. 2013; 131:e550–e558.
Article47. Nooitgedagt JE, Zwart P, Brand PL. Causes, treatment and clinical outcome in infants admitted because of excessive crying to the paediatric department of the Isala clinics, Zwolle, the Netherlands, 1997/'03. Ned Tijdschr Geneeskd. 2005; 149:472–477.48. Lucassen PL, Assendelft WJ, Gubbels JW, van Eijk JT, van Geldrop WJ, Neven AK. Effectiveness of treatments for infantile colic: systematic review. BMJ. 1998; 316:1563–1569.
Article49. Barr RG. The normal crying curve: what do we really know? Dev Med Child Neurol. 1990; 32:356–362.
Article50. Freedman SB, Al-Harthy N, Thull-Freedman J. The crying infant: diagnostic testing and frequency of serious underlying disease. Pediatrics. 2009; 123:841–848.
Article51. Shamir R, St James-Roberts I, Di Lorenzo C, Burns AJ, Thapar N, Indrio F, et al. Infant crying, colic, and gastrointestinal discomfort in early childhood: a review of the evidence and most plausible mechanisms. J Pediatr Gastroenterol Nutr. 2013; 57:Suppl 1. S1–S45.52. Wessel MA, Cobb JC, Jackson EB, Harris GS Jr, Detwiler AC. Paroxysmal fussing in infancy, sometimes called colic. Pediatrics. 1954; 14:421–435.
Article53. Barr RG. Excessive crying. In : Sameroff AJ, Lewis M, Miller SM, editors. Handbook of developmental psychopathology. 2nd ed. New York: Kluwer Academic/Plenum Publishers;2000. p. 327–350.54. Fujiwara T, Barr RG, Brant R, Barr M. Infant distress at five weeks of age and caregiver frustration. J Pediatr. 2011; 159:425–430.e1-2.
Article55. Gustafson G, Wood R, Green J. Can we hear the causes of infants' crying?. In : Barr RG, Hopkins B, Green JA, editors. Crying as a sign, a symptom, and a signal. London: Mac Keith Press;2000. p. 8–22.56. James-Roberts IS, Conroy S, Wilsher K. Bases for maternal perceptions of infant crying and colic behaviour. Arch Dis Child. 1996; 75:375–384.
Article57. Meyer EC, Coll CT, Lester BM, Boukydis CF, McDonough SM, Oh W. Family-based intervention improves maternal psychological well-being and feeding interaction of preterm infants. Pediatrics. 1994; 93:241–246.
Article58. Vik T, Grote V, Escribano J, Socha J, Verduci E, Fritsch M, et al. Infantile colic, prolonged crying and maternal postnatal depression. Acta Paediatr. 2009; 98:1344–1348.
Article59. Kurth E, Kennedy HP, Spichiger E, Hösli I, Stutz EZ. Crying babies, tired mothers: what do we know? A systematic review. Midwifery. 2011; 27:187–194.
Article60. Murray L, Cooper P. The impact of irritable infant behavior on maternal mental state: a longitudinal study and a treatment trial. In : Barr RG, St James-Roberts I, Keefe MR, editors. New evidence on unexplained early infant crying: its origins, nature and management. Skillman, NJ: Johnson & Johnson Pediatric Institute;2001. p. 149–164.61. Savino F, Cordisco L, Tarasco V, Palumeri E, Calabrese R, Oggero R, et al. Lactobacillus reuteri DSM 17938 in infantile colic: a randomized, double-blind, placebo-controlled trial. Pediatrics. 2010; 126:e526–e533.
Article62. Szajewska H, Gyrczuk E, Horvath A. Lactobacillus reuteri DSM 17938 for the management of infantile colic in breastfed infants: a randomized, double-blind, placebo-controlled trial. J Pediatr. 2013; 162:257–262.
Article63. Sung V, Hiscock H, Tang ML, Mensah FK, Nation ML, Satzke C, et al. Treating infant colic with the probiotic Lactobacillus reuteri: double blind, placebo controlled randomised trial. BMJ. 2014; 348:g2107.
Article64. Sung V, Collett S, de Gooyer T, Hiscock H, Tang M, Wake M. Probiotics to prevent or treat excessive infant crying: systematic review and meta-analysis. JAMA Pediatr. 2013; 167:1150–1157.
Article65. Kramer EA, den Hertog-Kuijl JH, van den Broek LM, van Leengoed E, Bulk AM, Kneepkens CM, et al. Defecation patterns in infants: a prospective cohort study. Arch Dis Child. 2015; 100:533–536.
Article66. Malowitz S, Green M, Karpinski A, Rosenberg A, Hyman PE. Age of onset of functional constipation. J Pediatr Gastroenterol Nutr. 2016; 62:600–602.
Article67. Koppen IJ, Lammers LA, Benninga MA, Tabbers MM. Management of functional constipation in children: therapy in practice. Paediatr Drugs. 2015; 17:349–360.
Article68. Tabbers MM, DiLorenzo C, Berger MY, Faure C, Langendam MW, Nurko S, et al. Evaluation and treatment of functional constipation in infants and children: evidence-based recommendations from ESPGHAN and NASPGHAN. J Pediatr Gastroenterol Nutr. 2014; 58:258–274.
Article69. von Baeyer CL, Champion GD. Commentary: multiple pains as functional pain syndromes. J Pediatr Psychol. 2011; 36:433–437.
Article70. Lee SJ, Ralston HJ, Drey EA, Partridge JC, Rosen MA. Fetal pain: a systematic multidisciplinary review of the evidence. JAMA. 2005; 294:947–954.71. Fitzgerald M. The development of nociceptive circuits. Nat Rev Neurosci. 2005; 6:507–520.
Article72. Lowery CL, Hardman MP, Manning N, Hall RW, Anand KJ, Clancy B. Neurodevelopmental changes of fetal pain. Semin Perinatol. 2007; 31:275–282.
Article73. Fitzgerald M, Walker SM. Infant pain management: a developmental neurobiological approach. Nat Clin Pract Neurol. 2009; 5:35–50.
Article74. Chitkara DK, van Tilburg MA, Blois-Martin N, Whitehead WE. Early life risk factors that contribute to irritable bowel syndrome in adults: a systematic review. Am J Gastroenterol. 2008; 103:765–774. quiz 775.
Article75. Gebhart GF. Pathobiology of visceral pain: molecular mechanisms and therapeutic implications IV. Visceral afferent contributions to the pathobiology of visceral pain. Am J Physiol Gastrointest Liver Physiol. 2000; 278:G834–G838.76. Hjermstad MJ, Fayers PM, Haugen DF, Caraceni A, Hanks GW, Loge JH, et al. Studies comparing numerical rating scales, verbal rating scales, and visual analogue scales for assessment of pain intensity in adults: a systematic literature review. J Pain Symptom Manage. 2011; 41:1073–1093.
Article77. Tomlinson D, von Baeyer CL, Stinson JN, Sung L. A systematic review of faces scales for the self-report of pain intensity in children. Pediatrics. 2010; 126:e1168–e1198.
Article78. Slater R, Cantarella A, Gallella S, Worley A, Boyd S, Meek J, et al. Cortical pain responses in human infants. J Neurosci. 2006; 26:3662–3666.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Understanding the Rome IV: Functional Constipation and Anorectal Disorders
- Understanding the Rome IV: Background to the Rome IV Revision
- Functional Gastrointestinal Disorders in Neonates and Toddlers According to the Rome IV Criteria: A Systematic Review and Meta-Analysis
- Validation of Rome III Criteria in the Diagnosis of Functional Gastrointestinal Disorders in Korean Patients
- Rome IV Clinical Criteria and Management of Functional Constipation: Indonesian Health Care Professionals’ Perspective