Tandem High-Dose Chemotherapy and Autologous Stem Cell Transplantation for Atypical Teratoid/Rhabdoid Tumor
- Affiliations
-
- 1Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 2Department of Radiation Oncology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Department of Radiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 4Department of Pathology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 5Department of Psychiatry, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 6Department of Neurosurgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. shinhj@skku.edu
- KMID: 2356243
- DOI: http://doi.org/10.4143/crt.2015.347
Abstract
- PURPOSE
We prospectively evaluated the effectiveness of tandem high-dose chemotherapy and autologous stem cell transplantation (HDCT/auto-SCT) in improving the survival of patients with atypical teratoid/rhabdoid tumors while reducing the risks of late adverse effects from radiotherapy (RT).
MATERIALS AND METHODS
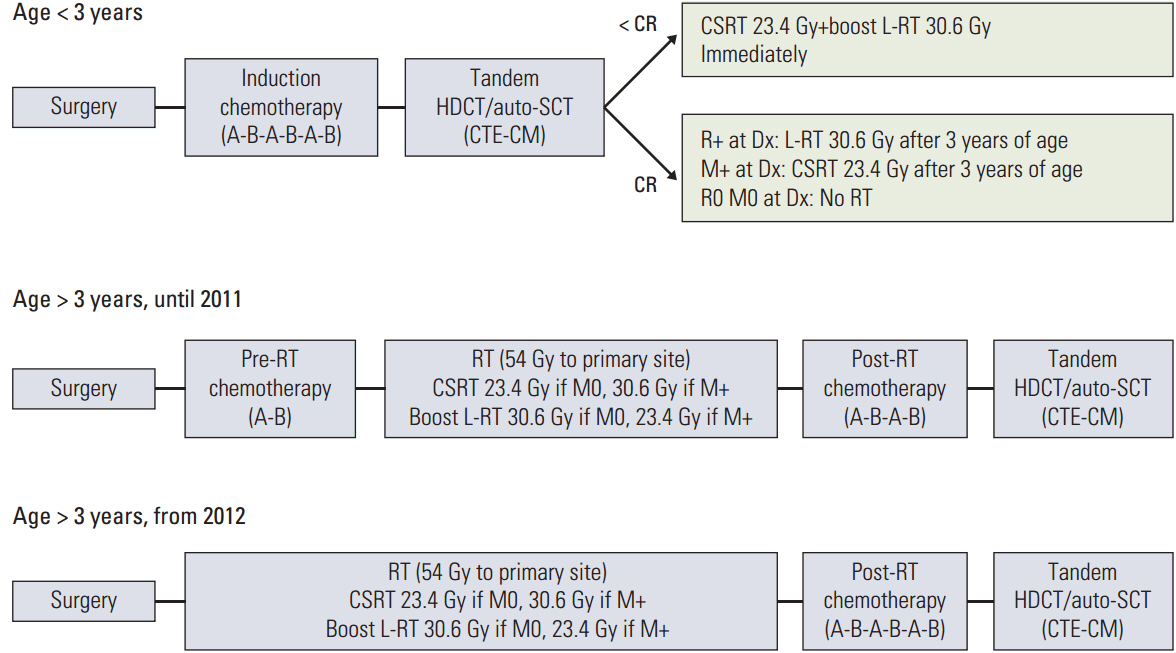
For young children (< 3 years old), tandem HDCT/auto-SCT was administered after six cycles of induction chemotherapy. RT was deferred until after 3 years of age unless the tumor showed relapse or progression. For older patients (> 3 years old), RT including reduced-dose craniospinal RT (23.4 or 30.6 Gy) was administered either after two cycles of induction chemotherapy or after surgery, and tandem HDCT/auto-SCT was administered after six cycles of induction chemotherapy.
RESULTS
A total of 13 patients (five young and eight older) were enrolled from November 2004 to June 2012. Eight patients, including all five young patients, had metastatic disease at diagnosis. Six patients (four young and two older) experienced progression before initiation of RT, and seven were able to proceed to HDCT/auto-SCT without progression during induction treatment. Three of six patients who experienced progression during induction treatment underwent HDCT/auto-SCT as salvage treatment. All five young patients died from disease progression. However, four of the eight older patients remain progression-freewith a median follow-up period of 64 months (range, 39 to 108 months). Treatment-related late toxicities were acceptable.
CONCLUSION
The required dose of craniospinal RT might be reduced in older patients if the intensity of chemotherapy is increased. However, early administration of RT should be considered to prevent early progression in young patients.
MeSH Terms
Figure
Cited by 5 articles
-
Atypical Teratoid/Rhabdoid Tumor of the Central Nervous System in Children under the Age of 3 Years
Meerim Park, Jung Woo Han, Seung Min Hahn, Jun Ah Lee, Joo-Young Kim, Sang Hoon Shin, Dong-Seok Kim, Hong In Yoon, Kyung Taek Hong, Jung Yoon Choi, Hyoung Jin Kang, Hee Young Shin, Ji Hoon Phi, Seung-Ki Kim, Ji Won Lee, Keon Hee Yoo, Ki Woong Sung, Hong Hoe Koo, Do Hoon Lim, Hyung Jin Shin, Hyery Kim, Kyung-Nam Koh, Ho Joon Im, Seung Do Ahn, Young-Shin Ra, Hee-Jo Baek, Hoon Kook, Tae-Young Jung, Hyoung Soo Choi, Chae-Yong Kim, Hyeon Jin Park, Chuhl Joo Lyu
Cancer Res Treat. 2021;53(2):378-388. doi: 10.4143/crt.2020.756.Radiation Therapy against Pediatric Malignant Central Nervous System Tumors : Embryonal Tumors and Proton Beam Therapy
Do Hoon Lim
J Korean Neurosurg Soc. 2018;61(3):386-392. doi: 10.3340/jkns.2018.0004.Tandem High-dose Chemotherapy and Autologous Stem Cell Transplantation in Children with Brain Tumors : Review of Single Center Experience
Ki Woong Sung, Do Hoon Lim, Hyung Jin Shin
J Korean Neurosurg Soc. 2018;61(3):393-401. doi: 10.3340/jkns.2018.0039.Atypical Teratoid Rhabdoid Tumour : From Tumours to Therapies
Elizabeth Anne Richardson, Ben Ho, Annie Huang
J Korean Neurosurg Soc. 2018;61(3):302-311. doi: 10.3340/jkns.2018.0061.Tandem High-Dose Chemotherapy Increases the Risk of Secondary Malignant Neoplasm in Pediatric Solid Tumors
Hana Lim, Minji Im, Eun Seop Seo, Hee Won Cho, Hee Young Ju, Keon Hee Yoo, Sung Yoon Cho, Jong-Won Kim, Do Hoon Lim, Ki Woong Sung, Ji Won Lee
Cancer Res Treat. 2024;56(2):642-651. doi: 10.4143/crt.2023.999.
Reference
-
References
1. Hilden JM, Meerbaum S, Burger P, Finlay J, Janss A, Scheithauer BW, et al. Central nervous system atypical teratoid/rhabdoid tumor: results of therapy in children enrolled in a registry. J Clin Oncol. 2004; 22:2877–84.
Article2. Tekautz TM, Fuller CE, Blaney S, Fouladi M, Broniscer A, Merchant TE, et al. Atypical teratoid/rhabdoid tumors (ATRT): improved survival in children 3 years of age and older with radiation therapy and high-dose alkylator-based chemotherapy. J Clin Oncol. 2005; 23:1491–9.
Article3. Bikowska B, Grajkowska W, Jozwiak J. Atypical teratoid/rhabdoid tumor: short clinical description and insight into possible mechanism of the disease. Eur J Neurol. 2011; 18:813–8.
Article4. von Hoff K, Hinkes B, Dannenmann-Stern E, von Bueren AO, Warmuth-Metz M, Soerensen N, et al. Frequency, risk-factors and survival of children with atypical teratoid rhabdoid tumors (AT/RT) of the CNS diagnosed between 1988 and 2004, and registered to the German HIT database. Pediatr Blood Cancer. 2011; 57:978–85.
Article5. Athale UH, Duckworth J, Odame I, Barr R. Childhood atypical teratoid rhabdoid tumor of the central nervous system: a meta-analysis of observational studies. J Pediatr Hematol Oncol. 2009; 31:651–63.6. Lafay-Cousin L, Hawkins C, Carret AS, Johnston D, Zelcer S, Wilson B, et al. Central nervous system atypical teratoid rhabdoid tumours: the Canadian Paediatric Brain Tumour Consortium experience. Eur J Cancer. 2012; 48:353–9.
Article7. Mulhern RK, Merchant TE, Gajjar A, Reddick WE, Kun LE. Late neurocognitive sequelae in survivors of brain tumours in childhood. Lancet Oncol. 2004; 5:399–408.
Article8. Matthay KK, Reynolds CP, Seeger RC, Shimada H, Adkins ES, Haas-Kogan D, et al. Long-term results for children with high-risk neuroblastoma treated on a randomized trial of myeloablative therapy followed by 13-cis-retinoic acid: a children's oncology group study. J Clin Oncol. 2009; 27:1007–13.
Article9. Fangusaro J, Finlay J, Sposto R, Ji L, Saly M, Zacharoulis S, et al. Intensive chemotherapy followed by consolidative myeloablative chemotherapy with autologous hematopoietic cell rescue (AuHCR) in young children with newly diagnosed supratentorial primitive neuroectodermal tumors (sPNETs): report of the Head Start I and II experi-ence. Pediatr Blood Cancer. 2008; 50:312–8.
Article10. Mason WP, Grovas A, Halpern S, Dunkel IJ, Garvin J, Heller G, et al. Intensive chemotherapy and bone marrow rescue for young children with newly diagnosed malignant brain tumors. J Clin Oncol. 1998; 16:210–21.
Article11. Gardner SL, Asgharzadeh S, Green A, Horn B, McCowage G, Finlay J. Intensive induction chemotherapy followed by high dose chemotherapy with autologous hematopoietic progenitor cell rescue in young children newly diagnosed with central nervous system atypical teratoid rhabdoid tumors. Pediatr Blood Cancer. 2008; 51:235–40.
Article12. Sung KW, Yoo KH, Cho EJ, Koo HH, Lim DH, Shin HJ, et al. High-dose chemotherapy and autologous stem cell rescue in children with newly diagnosed high-risk or relapsed medulloblastoma or supratentorial primitive neuroectodermal tumor. Pediatr Blood Cancer. 2007; 48:408–15.
Article13. Gajjar A, Chintagumpala M, Ashley D, Kellie S, Kun LE, Merchant TE, et al. Risk-adapted craniospinal radiotherapy followed by high-dose chemotherapy and stem-cell rescue in children with newly diagnosed medulloblastoma (St Jude Medulloblastoma-96): long-term results from a prospective, multicentre trial. Lancet Oncol. 2006; 7:813–20.
Article14. Sung KW, Lim DH, Lee SH, Yoo KH, Koo HH, Kim JH, et al. Tandem high-dose chemotherapy and auto-SCT for malignant brain tumors in children under 3 years of age. Bone Marrow Transplant. 2013; 48:932–8.
Article15. Sung KW, Lim DH, Son MH, Lee SH, Yoo KH, Koo HH, et al. Reduced-dose craniospinal radiotherapy followed by tandem high-dose chemotherapy and autologous stem cell transplantation in patients with high-risk medulloblastoma. Neuro Oncol. 2013; 15:352–9.
Article16. Laurent JP, Chang CH, Cohen ME. A classification system for primitive neuroectodermal tumors (medulloblastoma) of the posterior fossa. Cancer. 1985; 56:1807–9.
Article17. Finkelstein-Shechter T, Gassas A, Mabbott D, Huang A, Bartels U, Tabori U, et al. Atypical teratoid or rhabdoid tumors: improved outcome with high-dose chemotherapy. J Pediatr Hematol Oncol. 2010; 32:e182–6.
Article18. Park ES, Sung KW, Baek HJ, Park KD, Park HJ, Won SC, et al. Tandem high-dose chemotherapy and autologous stem cell transplantation in young children with atypical teratoid/rhabdoid tumor of the central nervous system. J Korean Med Sci. 2012; 27:135–40.
Article19. Zaky W, Dhall G, Ji L, Haley K, Allen J, Atlas M, et al. Intensive induction chemotherapy followed by myeloablative chemotherapy with autologous hematopoietic progenitor cell rescue for young children newly-diagnosed with central nervous system atypical teratoid/rhabdoid tumors: the Head Start III experience. Pediatr Blood Cancer. 2014; 61:95–101.
Article20. Chi SN, Zimmerman MA, Yao X, Cohen KJ, Burger P, Biegel JA, et al. Intensive multimodality treatment for children with newly diagnosed CNS atypical teratoid rhabdoid tumor. J Clin Oncol. 2009; 27:385–9.21. Lee SH, Son MH, Sung KW, Choi YB, Lee NH, Yoo KH, et al. Toxicity of tandem high-dose chemotherapy and autologous stem cell transplantation using carboplatin-thiotepa-etoposide and cyclophosphamide-melphalan regimens for malignant brain tumors in children and young adults. J Neurooncol. 2014; 120:507–13.
Article22. Duffner PK, Horowitz ME, Krischer JP, Friedman HS, Burger PC, Cohen ME, et al. Postoperative chemotherapy and delayed radiation in children less than three years of age with malignant brain tumors. N Engl J Med. 1993; 328:1725–31.
Article23. Grill J, Sainte-Rose C, Jouvet A, Gentet JC, Lejars O, Frappaz D, et al. Treatment of medulloblastoma with postoperative chemotherapy alone: an SFOP prospective trial in young children. Lancet Oncol. 2005; 6:573–80.
Article24. Pai Panandiker AS, Merchant TE, Beltran C, Wu S, Sharma S, Boop FA, et al. Sequencing of local therapy affects the pattern of treatment failure and survival in children with atypical teratoid rhabdoid tumors of the central nervous system. Int J Radiat Oncol Biol Phys. 2012; 82:1756–63.
Article25. Chen YW, Wong TT, Ho DM, Huang PI, Chang KP, Shiau CY, et al. Impact of radiotherapy for pediatric CNS atypical teratoid/rhabdoid tumor (single institute experience). Int J Radiat Oncol Biol Phys. 2006; 64:1038–43.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Tandem High-Dose Chemotherapy and Autologous Stem Cell Transplantation in Young Children with Atypical Teratoid/Rhabdoid Tumor of the Central Nervous System
- A Case of Central Nervous System Atypical Teratoid/Rhabdoid Tumor of The 4th Ventricle : A Highly Malignant Tumor in Infancy and Childhood Frequently Mistaken for Medulloblastoma
- A Case of Atypical Teratoid/Rhabdoid Tumor Arising from the Supratentorial Area
- Atypical Teratoid Rhabdoid Tumors in Adult Patient with Multiple Lesions
- Imaging Findings of Atypical Teratoid/Rhabdoid Tumor of Infancy & Childhood in CNS: Report of Two Cases