Endocrinol Metab.
2016 Sep;31(3):476-479. 10.3803/EnM.2016.31.3.476.
Cholestyramine Use for Rapid Reversion to Euthyroid States in Patients with Thyrotoxicosis
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Internal Medicine, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. ldj6026@catholic.ac.kr
- KMID: 2352989
- DOI: http://doi.org/10.3803/EnM.2016.31.3.476
Abstract
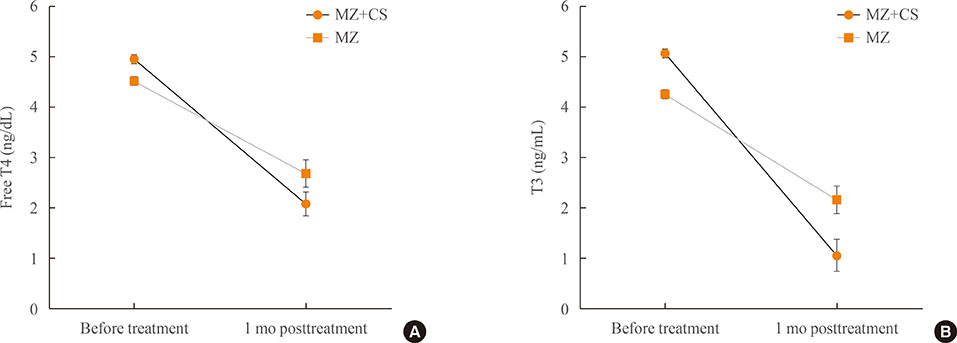
- Cholestyramine (CS) is an ion exchange resin, which binds to iodothyronines and would lower serum thyroid hormone level. The use of CS added to conventional antithyroid drugs to control thyrotoxicosis has been applied since 1980's, and several studies indicate that using CS in combination with methimazole (MZ) produces a more rapid decline in serum thyroid hormones than with only MZ treatment. Our recent retrospective review of five patients taking high dose MZ and CS, compared to age-, gender-, initial free thyroxine (T4) level-, and MZ dose-matched 12 patients with MZ use only, showed more rapid decline of both free T4 and triiodothyronine levels without more adverse events. CS could be safely applicable short-term adjunctive therapy when first-line antithyroid medications are not enough to adequately control severe thyrotoxicosis or side effects of antithyroid drug would be of great concern.
Keyword
MeSH Terms
Figure
Reference
-
1. Cooper DS. Antithyroid drugs. N Engl J Med. 2005; 352:905–917.2. Sebastián-Ochoa A, Quesada-Charneco M, Fernandez-Garcia D, Reyes-Garcia R, Rozas-Moreno P, Escobar-Jimenez F. Dramatic response to cholestyramine in a patient with Graves' disease resistant to conventional therapy. Thyroid. 2008; 18:1115–1117.3. Li H, Okuda J, Akamizu T, Mori T. A hyperthyroid patient with Graves' disease who was strongly resistant to methimazole: investigation on possible mechanisms of the resistance. Endocr J. 1995; 42:697–704.4. Mercado M, Mendoza-Zubieta V, Bautista-Osorio R, Espinoza-de los. Treatment of hyperthyroidism with a combination of methimazole and cholestyramine. J Clin Endocrinol Metab. 1996; 81:3191–3193.5. Solomon BL, Wartofsky L, Burman KD. Adjunctive cholestyramine therapy for thyrotoxicosis. Clin Endocrinol (Oxf). 1993; 38:39–43.6. Tsai WC, Pei D, Wang TF, Wu DA, Li JC, Wei CL, et al. The effect of combination therapy with propylthiouracil and cholestyramine in the treatment of Graves' hyperthyroidism. Clin Endocrinol (Oxf). 2005; 62:521–524.7. Yang Y, Hwang S, Kim M, Lim Y, Kim MH, Lee S, et al. Refractory Graves' disease successfully cured by adjunctive cholestyramine and subsequent total thyroidectomy. Endocrinol Metab (Seoul). 2015; 30:620–625.8. Shiroozu A, Okamura K, Ikenoue H, Sato K, Nakashima T, Yoshinari M, et al. Treatment of hyperthyroidism with a small single daily dose of methimazole. J Clin Endocrinol Metab. 1986; 63:125–128.9. Messina M, Milani P, Gentile L, Monaco A, Brossa C, Porta M, et al. Initial treatment of thyrotoxic Graves' disease with methimazole: a randomized trial comparing different dosages. J Endocrinol Invest. 1987; 10:291–295.10. Takata K, Kubota S, Fukata S, Kudo T, Nishihara E, Ito M, et al. Methimazole-induced agranulocytosis in patients with Graves' disease is more frequent with an initial dose of 30 mg daily than with 15 mg daily. Thyroid. 2009; 19:559–563.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Refractory Graves' Disease Successfully Cured by Adjunctive Cholestyramine and Subsequent Total Thyroidectomy
- A Case of Methimazole-Resistant Severe Graves' Disease: Dramatic Response to Cholestyramine
- Thyrotoxicosis Induced Sick Sinus Syndrome
- A Case of Thyrotoxic Periodic Paralysis Associated with Transient Thyrotoxicosis
- Thyrotoxicosis Associated with Autoimmune Thyroiditis in Children and Adolescents