Korean J Urol.
2009 Nov;50(11):1120-1124.
Results of Microorganism Detection by Multiplex Polymerase Chain Reaction in Patients with Chronic Pelvic Pain Syndrome
- Affiliations
-
- 1Department of Urology, National Medical Center, Seoul, Korea.
- 2Hole In One Urologic Clinic, Seoul, Korea. nmcuro@hanmail.net
Abstract
- PURPOSE
The aim of this study was to evaluate the results of multiplex polymerase chain reaction (PCR) in patients with chronic pelvic pain syndrome (CPPS) and the significance of microorganisms as the causative factor of CPPS.
MATERIALS AND METHODS
We evaluated the frequency of 19 possible causative microorganisms of prostatitis in 849 patients who had prostatitis symptoms from April 2007 to March 2009 by using multiplex PCR. All of the enrolled patients were category III by the definition of the NIH Chronic Prostatitis Workshop.
RESULTS
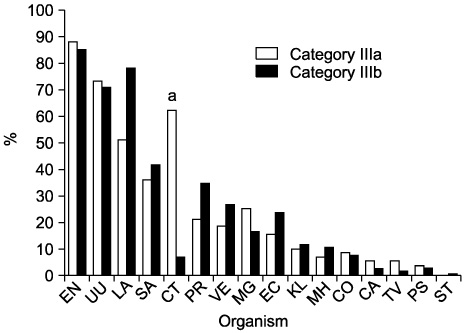
Of the 849 patients, 414 (49%) and 435 (51%) were categories IIIa (inflammatory CPPS) and IIIb (noninflammatory CPPS). On multiplex PCR, using the third voided urine specimen (VB3), 369 (89%) of the 414 category IIIa and 367 (84%) of the 435 category IIIb cases were found to have positive PCR results for causative microorganisms. The common microorganisms were Enterococcus, Ureaplasma urealyticum, Lactobacillus, Streptococcus agalactiae, and Chlamydia trachomatis in 173 (18%), 144 (15%), 129 (13%), 78 (8%), and 69 cases (7%), respectively.
CONCLUSIONS
There were too many positive PCR results for causative microorganisms in the CPPS patients despite negative urine culture examination. Therefore, it is necessary to rule out contamination of the specimen to achieve reliable results with multiplex PCR. However, multiplex PCR can detect various unknown microorganisms suggestive of the etiology of CPPS, particularly those that are difficult to cultivate. PCR is expected to play an important role in the diagnosis of CPPS, but further studies will be required to define the usefulness of molecular tests.
Keyword
MeSH Terms
Figure
Reference
-
1. Fowler JE Jr. Gillenwater JA, Grayhack JT, Howard SS, Duckett JW, editors. Prostatitis. Adult and pediatric urology. 1991. 2nd ed. St. Louis: Mosby-Year Book;1395–1423.2. Woo YN. Prostatitis. Korean J Urol. 1994. 35:575–585.3. Krieger JN, Egan KJ, Ross SO, Jacobs R, Berger RE. Chronic pelvic pains represent the most prominent urogenital symptoms of chronic prostatitis. Urology. 1996. 48:715–721.4. Alexander RB, Trissel D. Chronic prostatitis: results of an internet survey. Urology. 1996. 48:568–574.5. Krieger JN, Egan KJ. Comprehensive evaluation and treatment of 75 men referred to chronic prostatitis clinic. Urology. 1991. 38:11–19.6. Shoskes DA, Hakim L, Ghoniem G, Jackson CL. Long-term results of multimodal therapy for chronic prostatitis/chronic pelvic pain syndrome. J Urol. 2003. 169:1406–1410.7. Nickel JC. Effective office management of chronic prostatitis. Urol Clin North Am. 1998. 25:677–684.8. Berger RE, Krieger JN, Rothman I, Muller CH, Hillier SL. Bacteria in the prostate tissue of men with idiopathic prostatic inflammation. J Urol. 1997. 157:863–865.9. Ponniah S, Arah I, Alexander RB. PSA is a candidate self-antigen in autoimmune chronic prostatitis/chronic pelvic pain syndrome. Prostate. 2000. 44:49–54.10. Zermann DH, Ishigooka M, Doggweiler R, Schmidt RA. Neurourological insights into the etiology of genitourinary pain in men. J Urol. 1999. 161:903–908.11. Mehik A, Hellström P, Sarpola A, Lukkarinen O, Järvelin MR. Fears, sexual disturbances and personality features in men with prostatitis: a population-based cross-sectional study in Finland. BJU Int. 2001. 88:35–38.12. Bjerklund Johansen TE, Grüneberg RN, Guibert J, Hofstetter A, Lobel B, Naber KG, et al. The role of antibiotics in the treatment of chronic prostatitis: a consensus statement. Eur Urol. 1998. 34:457–466.13. Batstone GR, Doble A. Chronic prostatitis. Curr Opin Urol. 2003. 13:23–29.14. Johnson RE, Green TA, Schachter J, Jones RB, Hook EW 3rd, Black CM, et al. Evaluation of nucleic acid amplification tests as reference tests for Chlamydia trachomatis infections in asymptomatic men. J Clin Microbiol. 2000. 38:4382–4386.15. Kim SW, Lee JY, Park WJ, Cho YH, Yoon MS. The diagnostic values of the polymerase chain reaction in prostatitis. Korean J Infect Dis. 2000. 32:265–273.16. Ha JS, Kim SW, Cho YH. Detection of cryptic microorganisms by polymerase chain reaction assay in chronic pelvic pain syndrome. Korean J Urol. 2002. 43:396–401.17. Heo C, Hong SJ, Gil MC. Diagnostic value of polymerase chain reaction in patients with chronic pelvic pain syndrome: using semen as a specimen. Korean J Urol. 2007. 48:189–194.18. Kim TH, Kim TH, Kim HR, Lee MK, Myung SC, Kim YS. Detection of cryptic microorganisms in patients with chronic prostatitis by multiplex polymerase chain reaction. Korean J Urol. 2007. 48:304–309.19. Litwin MS, McNaughton-Collins M, Fowler FJ Jr, Nickel JC, Calhoun EA, Pontari MA, et al. The National Institutes of Health chronic prostatitis symptom index: development and validation of a new outcome measure. Chronic Prostatitis Collaborative Research Network. J Urol. 1999. 162:369–375.20. Krieger JN, Nyberg L Jr, Nickel JC. NIH consensus definition and classification of prostatitis. JAMA. 1999. 282:236–237.21. Blacklock NJ. Anatomical factors in prostatitis. Br J Urol. 1974. 46:47–54.22. Krieger JN, Riley DE, Roberts MC, Berger RE. Prokaryotic DNA sequences in patients with chronic idiopathic prostatitis. J Clin Microbiol. 1996. 34:3120–3128.23. Roberts RO, Lieber MM, Bostwick DG, Jacobsen SJ. A review of clinical and pathological prostatitis syndromes. Urology. 1997. 49:809–821.24. Lopez-Plaza I, Bostwick DG. Bostwick DG, editor. Prostatitis. Pathology of the prostate. 1990. 1st ed. New York: Churchill Livingstone;15–30.25. Moulder JW. Barron AL, editor. Characteristics of Chlamydia. Microbiology of chlamydia. 1988. Boca Raton: CRC Press;4–19.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Detection of Cryptic Microorganisms in Patients with Chronic Prostatitis by Multiplex Polymerase Chain Reaction
- Rapid Diagnosis of Duchenne Muscular Dystrophy DMD by Multiplex Polymerase Chain Reaction PCR using Uncultured Amniocytes
- Diagnostic Value of Polymerase Chain Reaction in Patients with Chronic Pelvic Pain Syndrome: using Semen as a Specimen
- Clinical Usefulness of Polymerase Chain Reaction for the Diagnosis of Pyosalpinx Caused by Tuberculosis
- Detection of Cryptic Microorganisms by Polymerase Chain Reaction Assay in Chronic Pelvic Pain Syndrome