Korean J Urol.
2007 Feb;48(2):189-194. 10.4111/kju.2007.48.2.189.
Diagnostic Value of Polymerase Chain Reaction in Patients with Chronic Pelvic Pain Syndrome: using Semen as a Specimen
- Affiliations
-
- 1Department of Urology, National Medical Center, Seoul, Korea. bestandro@ hanmail.net
- KMID: 2139759
- DOI: http://doi.org/10.4111/kju.2007.48.2.189
Abstract
-
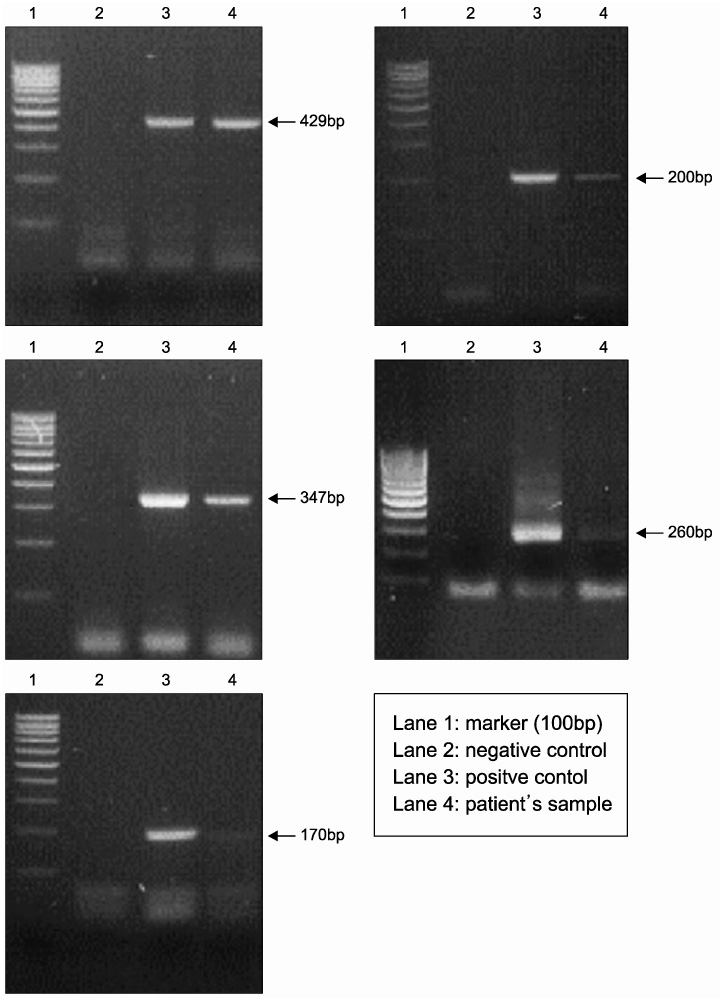
PURPOSE: Specific microorganisms, such as Chlamydia and Mycoplasma, are rarely detected in chronic pelvic pain syndrome, but fastidious and non-culturable microorganisms may be important in its etiology. The objective of this study was to evaluate the usefulness and significance of polymerase chain reaction (PCR) in the diagnosis of the etiologies of chronic pelvic pain syndrome, especially using semen as a specimen.
MATERIALS AND METHODS
Between August 2005 and July 2006, 237 patients, with a mean age of 39 years (range 25-67 years), were evaluated for chronic pelvic pain syndrome. PCR testing of the semen was performed in all cases to establish the persistence of C. trachomatis, T. vaginalis, M. hominis, M. genitalium and U. urealyticum.
RESULTS
Of the 237 patients, 79 (33.3%) and 158 (66.7%) were categories IIIa and IIIb, respectively. On PCR, using semen, 18 (22.8%) of the 79 category IIIa and 26 (16.5%) of the 158 category IIIb cases were found to have positive PCRs for the causative microorganisms of CPPS. In a total of 53 isolates presenting positive PCR, the common causative microorganisms were U. urealyticum, C. trachomatis, M. genitalium, T. vaginalis and M. hominis in 23 (43.4%), 16 (30.1%), 11 (20.8%), 2 (3.8%) and 1 case (1.9%), respectively. CONCLISIONS: PCR is revolutionizing the diagnosis of many infectious diseases, particularly those caused by microorganisms that are difficult to cultivate. Moreover, PCR shows nearly 100% accuracy in terms of sensitivity and specificity. PCR using semen, which can detect various microorganisms suggestive of the etiologies of chronic pelvic pain syndrome, is expected to play an important role in the diagnosis, treatment and follow up of chronic pelvic pain syndrome in urology.
Keyword
MeSH Terms
Figure
Reference
-
1. Lipsky BA. Urinary tract infections in men. Ann Intern Med. 1989. 110:138–150.2. Roberts RO, Lieber MM, Rhodes T, Girman CJ, Bostwick DG, Jacobsen SJ. Prevalence of a physician-assigned diagnosis of prostatitis: the olmsted county study of urinary symptoms and health status among men. Urology. 1998. 51:578–584.3. Fowler JE Jr. Gillenwater JA, Grayhack JT, Howard SS, Duckett JW, editors. Prostatitis. Adult and pediatric urology. 1991. 2nd ed. St. Louis: Mosky-Year Book;1395–1423.4. Yoo YN. Prostatitis. Korean J Urol. 1994. 35:575–585.5. Krieger JN, McGonagle LA. Diagnostic considerations and interpretation of microbiological findings for evaluation of chronic prostatitis. J Clin Microbiol. 1989. 27:2240–2244.6. Weidner W, Schiefer HG, Krauss H, Jantos CH, Friedrich HJ, Altmannsberger M. Chronic prostatitis: a through search for etiologically involved microorganism in 1,461 patients. Infection. 1991. 19:Suppl 3. 119S.7. Blacklock NJ. Anatomical factors in prostatitis. Br J Urol. 1974. 46:47–54.8. Nickel JC, Nyberg LM, Hennenfent M. Reserch guidelines for chronic prostatitis: consensus report from the first National Institutes of Health International Prostatitis Collaborative Network. Urology. 1999. 54:229–233.9. Wennimger K, Heiman JR, Rothman I, Berghuis JP, Berger RE. Sickness impact of chronic nonbacterial prostatitis and its correlates. J Urol. 1996. 155:965–968.10. von Lackum WH. Clinical and experimental data on prostatic infection. J Urol. 1927. 18:293–306.11. Campbell MF. Campbell MF, editor. The male reproductive tract: the prostate. Principles of urology: an introductory text to the desease of the urological tract. Campbell's urology. 1957. 1st ed. Philadelphia: WB Saunders;311–313.12. Drach GW, Fair WR, Meares EM, Stamey TA. Classification of benign diseases associated with prostatic pain: prostatitis or prostatodynia? J Urol. 1978. 120:266.13. Lopez-Plaza I, Bostwick DG. Bostwick DG, editor. Prostatitis. Pathology of the prostate. 1990. 1st ed. New York: Churchill Livingstone;15–30.14. Shoskes DA, Hakim L, Ghoniem G, Jackson CL. Long-term results of multimodal therapy for chronic prostatitis/chronic pelvic pain syndrome. J Urol. 2003. 169:1406–1410.15. Batstone GR, Doble A, Batstone D. Chronic prostatitis. Curr Opin Urol. 2003. 13:23–29.16. Meares EM Jr. Acute and chronic prostatitis: diagnosis and treatment. Infect Dis Clin North Am. 1987. 1:855–873.17. Roberts RO, Lieber MM, Bostwick DG, Jacobsen SJ. A review of clinical and pathological prostatitis syndromes. Urology. 1997. 49:809–821.18. Eisenstein BI. The polymerase chain reaction: a new method of using molecular genetics for medical diagnosis. N Engl J Med. 1990. 322:178–183.19. Perter JB. The polymerase chain reaction: amplifying our option. Rev Inf Dis. 1991. 13:166–171.20. Kim KH, Ha GY, Lee KS. Detection of mycobacterium tuberculosis in urine using polymerase chain reaction. Korean J Urol. 2004. 45:924–928.21. Krieger JN, Riley DE, Roberts MC, Berger RE. Prokaryotic DNA sequences in patients with chronic idiopathic prostatitis. J Clin Microbiol. 1996. 34:3120–3128.22. Ha JS, Kim SW, Cho YH. Detection of cryptic microorganisms by polymerase chain reaction assay in chronic pelvic pain syndrome. Korean J Urol. 2002. 43:396–401.23. Mandar R, Raukas E, Turk S, Korrovits P, Punab M. Mycoplasmas in semen of chronic prostatitis patients. Scand J Urol Nephrol. 2005. 39:479–482.24. Badalyan RR, Fanarjyan SV, Aghajanyan IG. Chlamydial and ureaplasmal infection in patients with nonbacterial chronic prostatitis. Andrologia. 2003. 35:263–265.25. Budia A, Palmero JL, Broseta E, Tejadillos S, Benedicto A, Queipo JA, et al. Value of semen culture in the diagnosis of chronic bacterial prostatitis: a simlified method. Scand J Urol Nephrol. 2006. 40:326–331.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Results of Microorganism Detection by Multiplex Polymerase Chain Reaction in Patients with Chronic Pelvic Pain Syndrome
- Detection of Cryptic Microorganisms by Polymerase Chain Reaction Assay in Chronic Pelvic Pain Syndrome
- The Diagnostic Values of the Polymerase Chain Reaction in Prostatitis
- Clinical Usefulness of Polymerase Chain Reaction for the Diagnosis of Pyosalpinx Caused by Tuberculosis
- The Diagnosis of Chronic Pelvic Pain: How Can We Detect Urological Pain?