Perilla oil improves blood flow through inhibition of platelet aggregation and thrombus formation
- Affiliations
-
- 1College of Veterinary Medicine, Chungbuk National University, Cheongju, Korea. solar93@cbu.ac.kr rheemh@knu.ac.kr
- 2Misuba RTech Co., Ltd., Asan, Korea.
- 3Department of Food Science and Nutrition, Hoseo University, Asan, Korea.
- 4College of Veterinary Medicine, Kyungpook National University, Daegu, Korea. solar93@cbu.ac.kr rheemh@knu.ac.kr
- KMID: 2312116
- DOI: http://doi.org/10.5625/lar.2014.30.1.21
Abstract
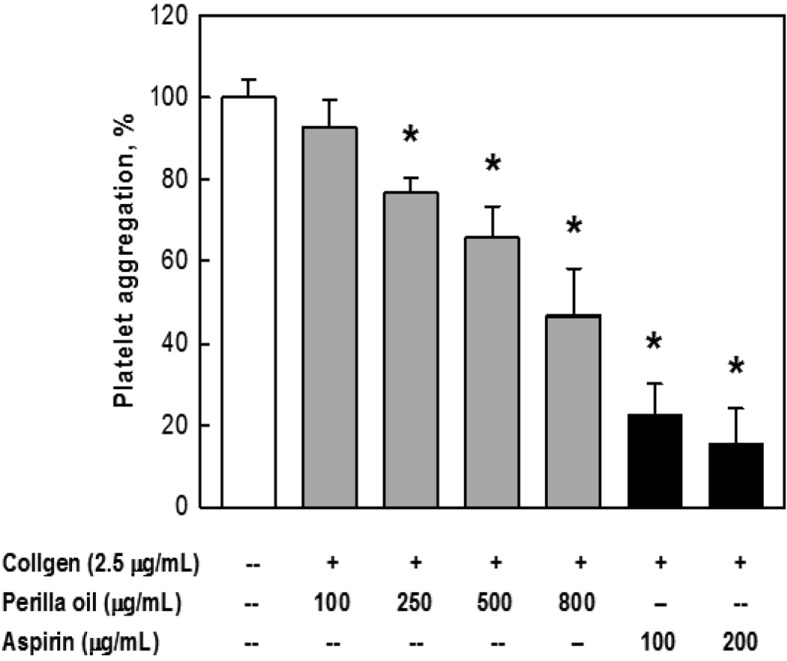
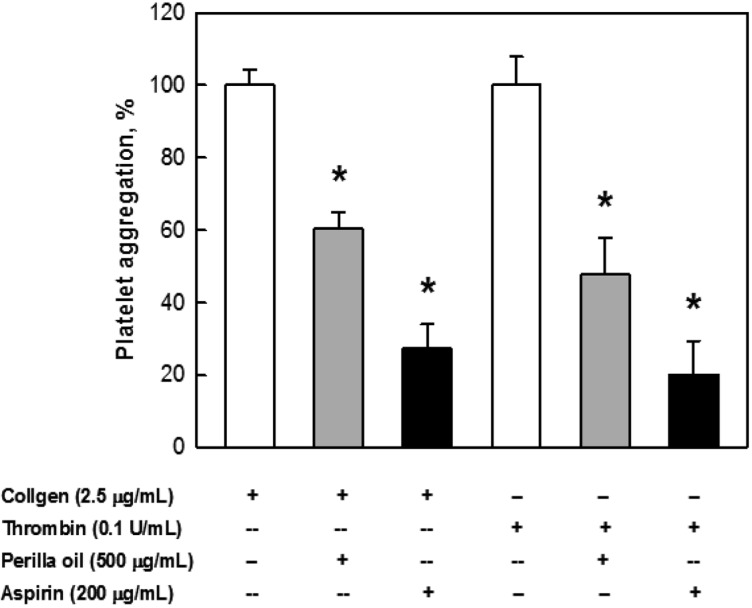
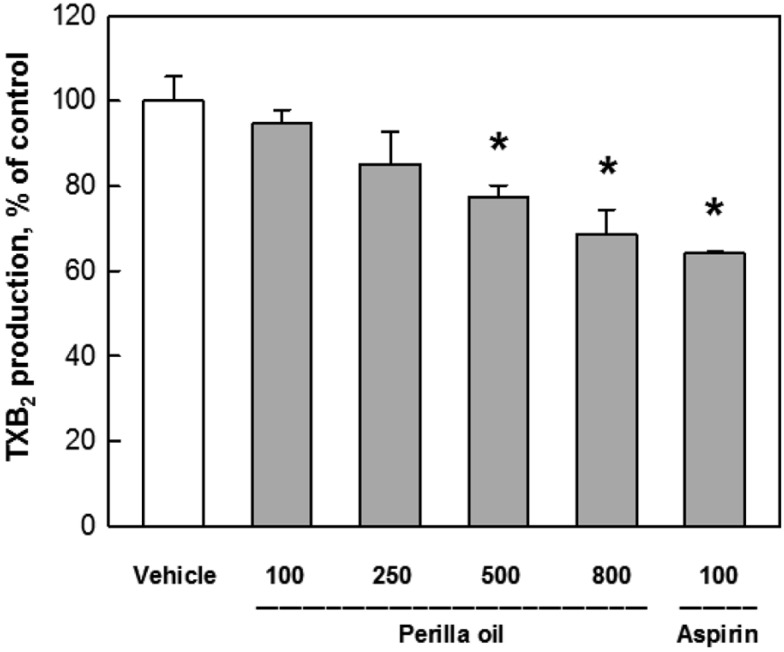
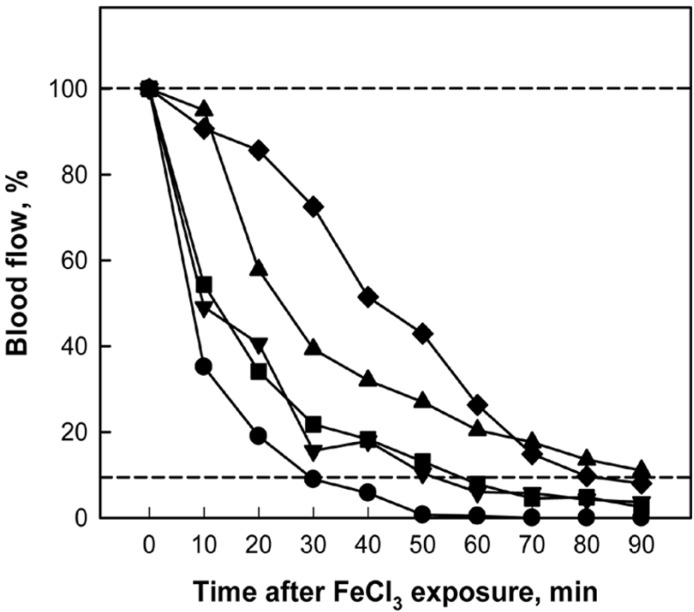
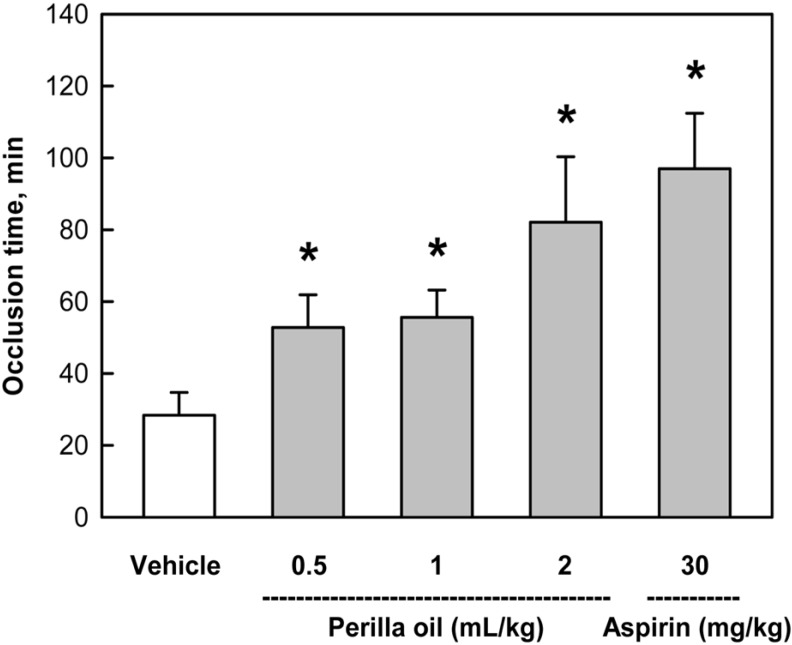
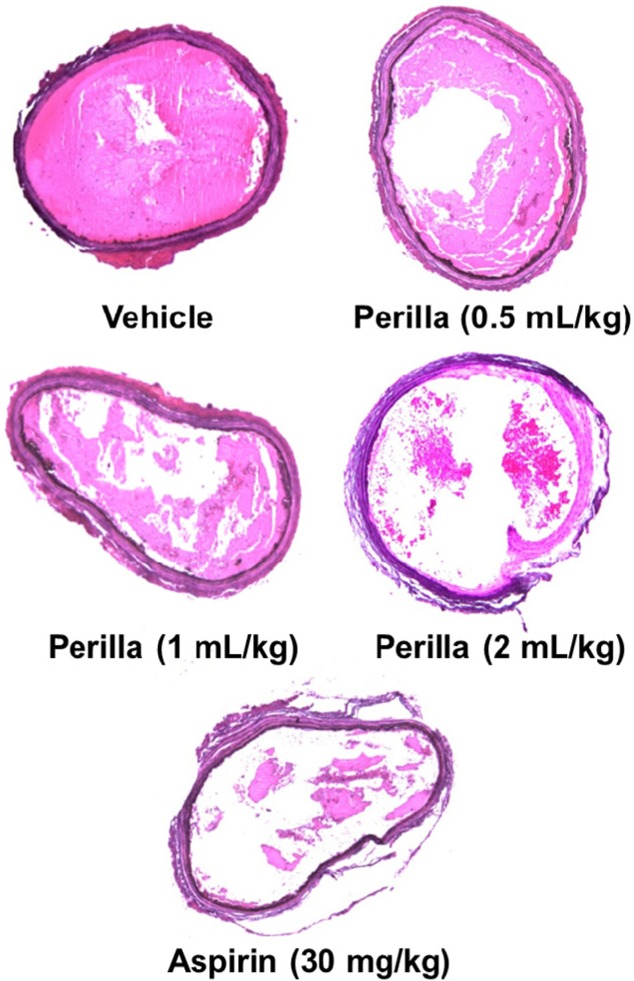
- The inhibitory effects of perilla oil on the platelet aggregation in vitro and thrombosis in vivo were investigated in comparison with aspirin, a well-known blood flow enhancer. Rabbit platelet-rich plasma was incubated with perilla oil and aggregation inducers collagen or thrombin, and the platelet aggregation rate was analyzed. Perilla oil significantly inhibited both the collagen- and thrombin-induced platelet aggregations, in which the thromboxane B2 formation from collagen-activated platelets were reduced in a concentration-dependent manner. Rats were administered once daily by gavage with perilla oil for 1 week, carotid arterial thrombosis was induced by applying 35% FeCl3-soaked filter paper for 10 min, and the blood flow was monitored with a laser Doppler probe. Perilla oil delayed the FeCl3-induced arterial occlusion in a dose-dependent manner, doubling the occlusion time at 0.5 mL/kg. In addition, a high dose (2 mL/kg) of perilla oil greatly prevented the occlusion, comparable to the effect of aspirin (30 mg/kg). The results indicate that perilla oil inhibit platelet aggregation by blocking thromboxane formation, and thereby delay thrombosis following oxidative arterial wall injury. Therefore, it is proposed that perilla oil could be a good candidate without adverse effects for the improvement of blood flow.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
Protective effects of perilla oil and alpha linolenic acid on SH-SY5Y neuronal cell death induced by hydrogen peroxide
Ah Young Lee, Ji Myung Choi, Myoung Hee Lee, Jaemin Lee, Sanghyun Lee, Eun Ju Cho
Nutr Res Pract. 2018;12(2):93-100. doi: 10.4162/nrp.2018.12.2.93.Anti-atherosclerotic effects of perilla oil in rabbits fed a high-cholesterol diet
Yeseul Cha, Ja Young Jang, Young-Hwan Ban, Haiyu Guo, Kyungha Shin, Tae-Su Kim, Sung-Pyo Lee, Jieun Choi, Eun-Suk An, Da-Woom Seo, Jung-Min Yon, Ehn-Kyoung Choi, Yun-Bae Kim
Lab Anim Res. 2016;32(3):171-179. doi: 10.5625/lar.2016.32.3.171.Blood flow-improving activity of methyl jasmonate-treated adventitious roots of mountain ginseng
Young-Hwan Ban, Yeseul Cha, Jieun Choi, Eun Suk An, Ji Young Lee, Nu Ry Han, Da Woom Seo, Gooyoung Jung, Da-Hye Jeong, Man Hee Rhee, Ehn-Kyoung Choi, Yun-Bae Kim
Lab Anim Res. 2017;33(2):105-113. doi: 10.5625/lar.2017.33.2.105.
Reference
-
1. Majid A, Delanty N, Kantor J. Antiplatelet agents for secondary prevention of ischemic stroke. Ann Pharmacother. 2001; 35(10):1241–1247. PMID: 11675854.
Article2. Jackson SP, Nesbitt WS, Kulkarni S. Signaling events underlying thrombus formation. J Thromb Haemost. 2003; 1(7):1602–1612. PMID: 12871297.
Article3. Farndale RW, Sixma JJ, Barnes MJ, de Groot PG. The role of collagen in thrombosis and hemostasis. J Thromb Haemost. 2004; 2(4):561–573. PMID: 15102010.
Article4. Konno C, Oshima Y, Hikino H. Morusinol, isoprenoid flavone from Morus root barks. Planta Med. 1977; 32(2):118–124. PMID: 905426.5. Cowan DH. Platelet adherence to collagen: role of prostaglandin-thromboxane synthesis. Br J Haematol. 1981; 49(3):425–434. PMID: 6794597.
Article6. Dogné JM, Hanson J, de Leval X, Pratico D, Pace-Asciak CR, Drion P, Pirotte B, Ruan KH. From the design to the clinical application of thromboxane modulators. Curr Pharm Des. 2006; 12(8):903–923. PMID: 16533159.7. Arita H, Nakano T, Hanasaki K. Thromboxane A2: its generation and role in platelet activation. Prog Lipid Res. 1989; 28(4):273–301. PMID: 2534976.
Article8. Gilmer JF, Murphy MA, Shannon JA, Breen CG, Ryder SA, Clancy JM. Single oral dose study of two isosorbide-based aspirin prodrugs in the dog. J Pharm Pharmacol. 2003; 55(10):1351–1357. PMID: 14607016.
Article9. Lee JJ, Yang H, Yoo YM, Hong SS, Lee D, Lee HJ, Lee HJ, Myung CS, Choi KC, Jeung EB. Morusinol extracted from Morus alba inhibits arterial thrombosis and modulates platelet activation for the treatment of cardiovascular disease. J Atheroscler Thromb. 2012; 19(6):516–522. PMID: 22472211.10. Kim HK, Choi S, Choi H. Suppression of hepatic fatty acid synthase by feeding alpha-linolenic acid rich perilla oil lowers plasma triacylglycerol level in rats. J Nutr Biochem. 2004; 15(8):485–492. PMID: 15302084.11. Huang MZ, Watanabe S, Kobayashi T, Nagatsu A, Sakakibara J, Okuyama H. Unusual effects of some vegetable oils on the survival time of stroke-prone spontaneously hypertensive rats. Lipids. 1997; 32(7):745–751. PMID: 9252963.
Article12. Okuyama H, Yamada K, Miyazawa D, Yasui Y, Ohara N. Dietary lipids impacts on healthy ageing. Lipids. 2007; 42(9):821–825. PMID: 17546469.
Article13. Lanzmann-Petithory D. Alpha-linolenic acid and cardiovascular diseases. J Nutr Health Aging. 2001; 5(3):179–183. PMID: 11458289.14. Vanschoonbeek K, de Maat MP, Heemskerk JW. Fish oil consumption and reduction of arterial disease. J Nutr. 2003; 133(3):657–660. PMID: 12612132.
Article15. De Caterina R, Cybulsky MA, Clinton SK, Gimbrone MA Jr, Libby P. Omega-3 fatty acids and endothelial leukocyte adhesion molecules. Prostaglandins Leukot Essent Fatty Acids. 1995; 52(2-3):191–195. PMID: 7540306.
Article16. Zhang L, Geng Y, Yin M, Mao L, Zhang S, Pan J. Low omega-6/omega-3 polyunsaturated fatty acid ratios reduce hepatic C-reactive protein expression in apolipoprotein E-null mice. Nutrition. 2010; 26(7-8):829–834. PMID: 20004083.17. Griffin MD, Sanders TA, Davies IG, Morgan LM, Millward DJ, Lewis F, Slaughter S, Cooper JA, Miller GJ, Griffin BA. Effects of altering the ratio of dietary n-6 to n-3 fatty acids on insulin sensitivity, lipoprotein size, and postprandial lipemia in men and postmenopausal women aged 45-70 y: the OPTILIP Study. Am J Clin Nutr. 2006; 84(6):1290–1298. PMID: 17158408.
Article18. de Lorgeril M, Renaud S, Mamelle N, Salen P, Martin JL, Monjaud I, Guidollet J, Touboul P, Delaye J. Mediterranean alpha-linolenic acid-rich diet in secondary prevention of coronary heart disease. Lancet. 1994; 343(8911):1454–1459. PMID: 7911176.
Article19. Heemskerk JW, Vossen RC, van Dam-Mieras MC. Polyunsaturated fatty acids and function of platelets and endothelial cells. Curr Opin Lipidol. 1996; 7(1):24–29. PMID: 8925184.
Article20. Jang JY, Kim TS, Cai J, Kim J, Kim Y, Shin K, Kim KS, Park SK, Lee SP, Choi EK, Rhee MH, Kim YB. Nattokinase improves blood flow by inhibiting platelet aggregation and thrombus formation. Lab Anim Res. 2013; 29(4):221–225. PMID: 24396387.
Article21. Born GV, Cross MJ. The aggregation of blood platelets. J Physiol. 1963; 168:178–195. PMID: 14056485.
Article22. Furie B, Furie BC. Thrombus formation in vivo. J Clin Invest. 2005; 115(12):3355–3362. PMID: 16322780.
Article23. Shimizu T, Igarashi J, Ohtuka Y, Oguchi S, Kaneko K, Yamashiro Y. Effects of n-3 polyunsaturated fatty acids and vitamin E on colonic mucosal leukotriene generation, lipid peroxidation, and microcirculation in rats with experimental colitis. Digestion. 2001; 63(1):49–54. PMID: 11173900.
Article24. Holy EW, Forestier M, Richter EK, Akhmedov A, Leiber F, Camici GG, Mocharla P, Lüscher TF, Beer JH, Tanner FC. Dietary α-linolenic acid inhibits arterial thrombus formation, tissue factor expression, and platelet activation. Arterioscler Thromb Vasc Biol. 2011; 31(8):1772–1780. PMID: 21571683.
Article25. Ascherio A, Rimm EB, Giovannucci EL, Spiegelman D, Stampfer M, Willett WC. Dietary fat and risk of coronary heart disease in men: cohort follow up study in the United States. BMJ. 1996; 313:84–90. PMID: 8688759.
Article26. Hu FB, Stampfer MJ, Manson JE, Rimm EB, Wolk A, Colditz GA, Hennekens CH, Willett WC. Dietary intake of alpha-linolenic acid and risk of fatal ischemic heart disease among women. Am J Clin Nutr. 1999; 69(5):890–897. PMID: 10232627.27. Huang MZ, Naito Y, Watanabe S, Kobayashi T, Kanai H, Nagai H, Okuyama H. Effect of rapeseed and dietary oils on the mean survival time of stroke-prone spontaneously hypertensive rats. Biol Pharm Bull. 1996; 19(4):554–557. PMID: 8860957.
Article28. Ratnayake S, Lewandowski P. Rapid bioassay-guided screening of toxic substances in vegetable oils that shorten the life of SHRSP rats. Lipids Health Dis. 2010; 9:13. PMID: 20122175.
Article29. Sanbongi C, Takano H, Osakabe N, Sasa N, Natsume M, Yanagisawa R, Inoue KI, Sadakane K, Ichinose T, Yoshikawa T. Rosmarinic acid in perilla extract inhibits allergic inflammation induced by mite allergen, in a mouse model. Clin Exp Allergy. 2004; 34(6):971–977. PMID: 15196288.
Article30. Lin CS, Kuo CL, Wang JP, Cheng JS, Huang ZW, Chen CF. Growth inhibitory and apoptosis inducing effect of Perilla frutescens extract on human hepatoma HepG2 cells. J Ethnopharmacol. 2007; 112(3):557–567. PMID: 17574356.
Article31. Kim MJ, Kim HK. Perilla leaf extract ameliorates obesity and dyslipidemia induced by high-fat diet. Phytother Res. 2009; 23(12):1685–1690. PMID: 19444921.
Article32. Ueda H, Yamazaki C, Yamazaki M. Inhibitory effect of perilla leaf extract and luteolin on mouse skin tumor promotion. Biol Pharm Bull. 2003; 26(4):560–563. PMID: 12673045.
Article33. Kim EK, Lee SJ, Lim BO, Jeon YJ, Song MD, Park TK, Lee KH, Kim B, Lee SR, Moon SH. Antioxidative and neuroprotective effects of enzymatic extracts from leaves of Perilla frutescens var. japonica. Food Sci Biotechnol. 2008; 17:279–286.34. Rao ChV, Ojha SK, Radhakrishnan K, Govindarajan R, Rastogi S, Mehrotra S, Pushpangadan P. Antiulcer activity of Utleria salicifolia rhizome extract. J Ethnopharmacol. 2004; 91(2-3):243–249. PMID: 15120446.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nattokinase improves blood flow by inhibiting platelet aggregation and thrombus formation
- Anti-atherosclerotic effects of perilla oil in rabbits fed a high-cholesterol diet
- Acute Ischemic Stroke Associated with Essential Thrombocythemia and Suspected Platelet Aggregation in Intracranial Artery
- Rescue Utilization of Abciximab (ReoPro) for the Thrombus
- A study on clinical usefulness of platelet aggregation test in whole blood