Korean J Urol.
2008 Jan;49(1):43-48.
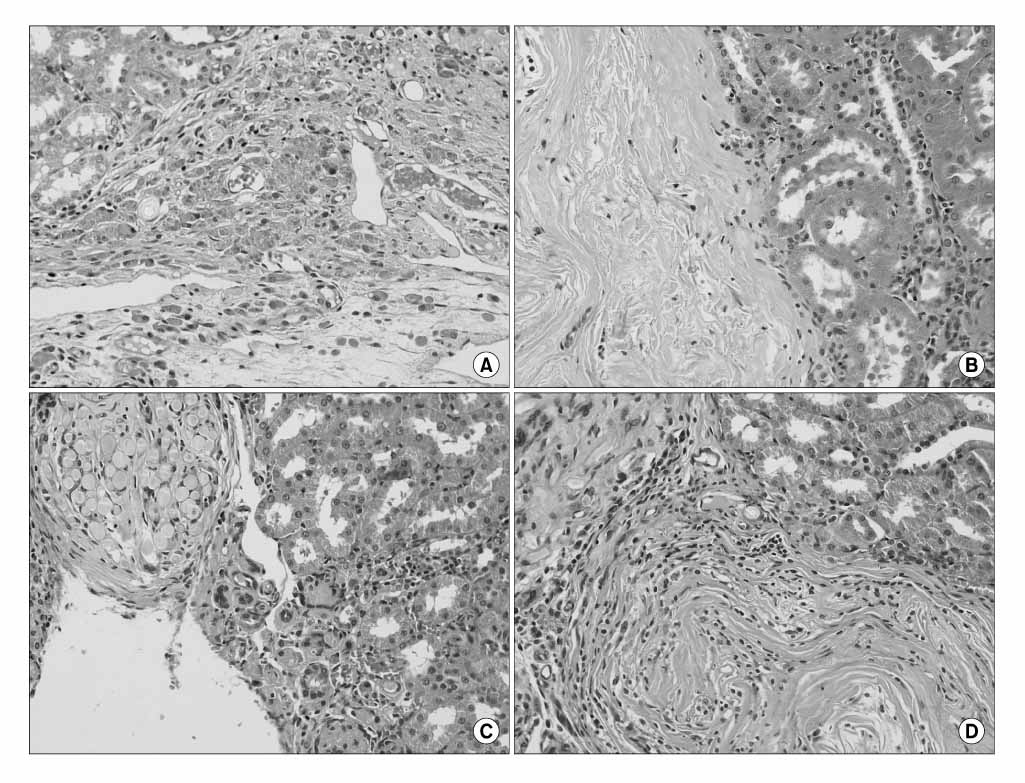
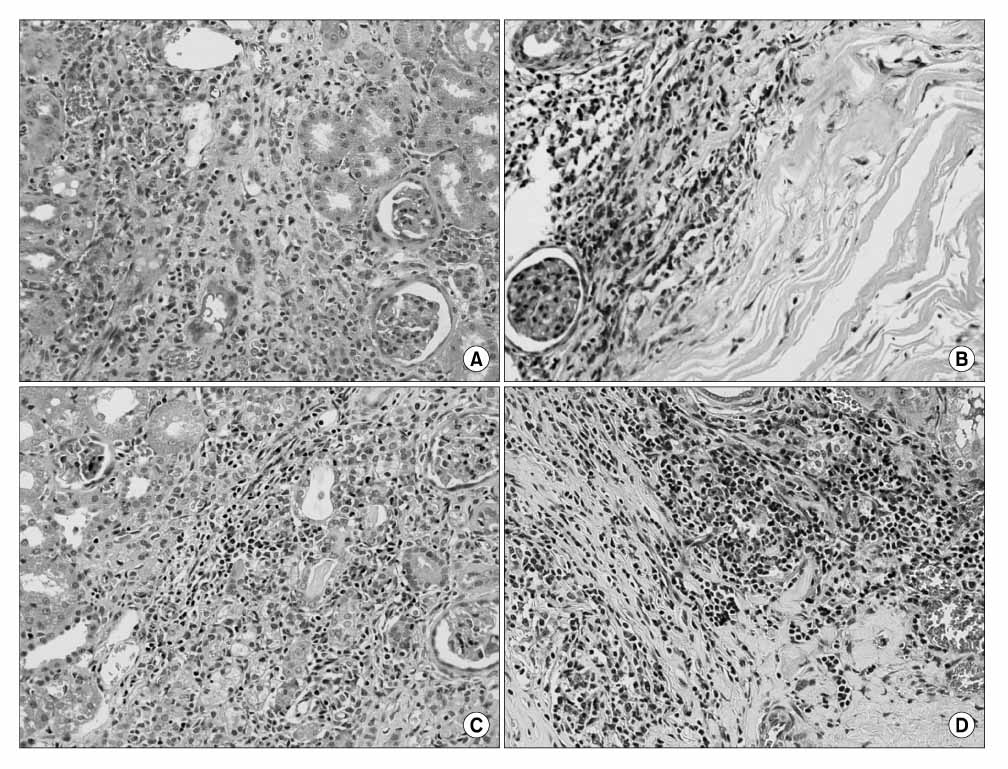
Comparison of the Intraparenchymal Biocompatibility of Oxidized Regenerated Cellulose and Porcine Small Intestine Submucosa in Rat Kidney
- Affiliations
-
- 1Department of Urology, Urological Science Institute, Yonsei University College of Medicine, Seoul, Korea. syang313@yumc.yonsei.ac.kr
- 2Department of Pathology, Urological Science Institute, Yonsei University College of Medicine, Seoul, Korea.
Abstract
-
PURPOSE: The objective of this study was to evaluate the biological properties of a variety of materials that could be used in partial nephrectomy.
MATERIALS AND METHODS
54 Sprague-Dawley rats(9 for each group) divided into an experimental period of 4 and 12 weeks, respectively. 2 other groups were the negative control for this experiment. We inserted oxidized regenerated cellulose and porcine small intestine submucosa into the defected renal parenchyme in the experimental groups. At the end of the observation periods, the animals were killed and their specimens prepared for histological examination to evaluate the different materials biocompatibility.
RESULTS
The reaction of the tissue to the materials diminished with time. After analyzing both periods, the inflammatory reactions to oxidized regenerated cellulose and porcine small intestine submucosa were considered slight. There were no significant differences between oxidized regenerated cellulose and porcine small intestine submucosa. Oxidized regenerated cellulose and porcine small intestine submucosa showed biocompatibility in this test model at both time periods.
CONCLUSIONS
It was concluded that there was no difference of biocompatibility between oxidized regenerated cellulose and porcine small intestine submucosa. Both materials are safe, biocompatible materials that can be inserted into the renal parenchyma.
Keyword
MeSH Terms
Figure
Reference
-
1. Polascik TJ, Pound CR, Meng MV, Partin AW, Marshall FF. Partial nephrectomy: technique, complications and pathological findings. J Urol. 1995. 154:1312–1318.2. O'connor RC, Harding JN 3rd, Steinberg GD. Novel modification of partial nephrectomy technique using porcine small intestine submucosa. Urology. 2002. 60:906–909.3. Sousa CJ, Loyola AM, Versiani MA, Biffi JC, Oliveira RP, Pascon EA. A comparative histological evaluation of the biocompatibility of materials used in apical surgery. Int Endod J. 2004. 37:738–748.4. Federation Dentaire Internationale. Recommended standard practices for the biological evaluation of dental materials. Int Dent J. 1980. 30:174–176.5. Kim WJ, Chung JI, Hong JH, Kim CS, Jung SI, Yoon DK. Epidemiologic study for urologic cancer in Korea (1998-2002). Korean J Urol. 2004. 45:1081–1088.6. Jayson M, Sanders H. Increased incidence of serendipitously discovered renal cell carcinoma. Urology. 1998. 51:203–205.7. Fergany AF, Hafez KS, Novick AC. Long-term results of nephron sparing surgery for localized renal cell carcinoma: 10-year followup. J Urol. 2000. 163:442–445.8. Nam JK, Cha CS, Chung MK. The treatment outcomes of a partial nephrectomy in the management of renal cell carcinomas. Korean J Urol. 2004. 45:1100–1105.9. Pierce AM, Wiebkin OW, Wilson DF. Surgicel: its fate following implantation. J Oral Pathol. 1984. 13:661–670.10. Bornemisza G, Ladanyi J, Furka I, Miko I. Effect of absorbable cellulose on the renal parenchyma. Acta Chir Acad Sci Hung. 1976. 17:329–333.11. Liatsikos EN, Dinlenc CZ, Kapoor R, Bernardo NO, Pikhasov D, Anderson AE, et al. Ureteral reconstruction: small intestine submucosa for the management of strictures and defects of the upper third of the ureter. J Urol. 2001. 165:1719–1723.12. Xie H, Shaffer BS, Wadia Y, Gregory KW. Use of reconstructed small intestine submucosa for urinary tract replacement. ASAIO J. 2000. 46:268–272.13. Kropp BP. Small-intestinal submucosa for bladder augmentation: a review of preclinical studies. World J Urol. 1998. 16:262–267.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A randomized controlled trial to compare the efficacy of regenerated and non-regenerated oxidized cellulose gauze for the secondary treatment of local bleeding in patients undergoing hepatic resection
- Efficacy of Oxidized Regenerated Cellulose, SurgiGuard®, in Porcine Surgery
- Antiadhesive effect and safety of oxidized regenerated cellulose after thyroidectomy: a prospective, randomized controlled study
- Wound healing effect of regenerated oxidized cellulose versus fibrin sealant patch: An in vivo study
- AN EXPERIMENTAL STUDY ON THE EFFECTS OF OXIDIZED CELLULOSE COVERAGE ON THE CORTICAL BONY DEFECTS