Korean Circ J.
2011 Oct;41(10):583-589. 10.4070/kcj.2011.41.10.583.
Telmisartan Versus Valsartan in Patients With Hypertension: Effects on Cardiovascular, Metabolic, and Inflammatory Parameters
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Korea University College of Medicine, Seoul, Korea. withnoel@empal.com
- KMID: 2297917
- DOI: http://doi.org/10.4070/kcj.2011.41.10.583
Abstract
- BACKGROUND AND OBJECTIVES
Angiotensin-receptor blockers (ARBs) have beneficial effects on cardiovascular, metabolic, and inflammatory parameters in addition to controlling blood pressure (BP). However, few comparative clinical studies have been conducted with different ARBs. We compared these effects in patients with uncomplicated hypertension who were receiving telmisartan or valsartan.
SUBJECTS AND METHODS
The subjects were patients with essential hypertension (48.4+/-9.6 years) who were randomly assigned to take either telmisartan (80 mg/day, n=30) or valsartan (160 mg/day, n=30) for 12 weeks. Their anthropometric, laboratory, vascular, and echocardiographic data were measured at baseline and at the end of the study.
RESULTS
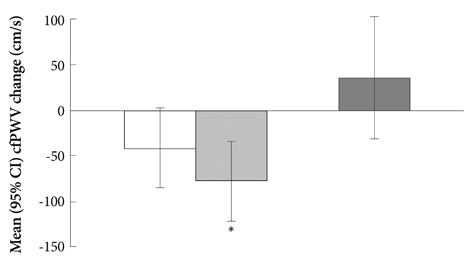
Baseline characteristics were not significantly different between the two groups, except for the carotid-femoral pulse wave velocity (cfPWV; telmisartan group vs. valsartan group; 841.2+/-131.0 vs. 761.1+/-104.4 cm/s, p<0.05). After 12 weeks, BP had fallen to a similar extent with mean reductions in the systolic and diastolic BP of 20.7+/-18.1 and 16.3+/-13.0 mm Hg (p<0.001, respectively) for the telmisartan and 22.5+/-17.0 and 16.8+/-9.3 mm Hg (p<0.001, respectively) for the valsartan group. Although the cfPWV and left ventricular mass index (LVMI) fell significantly only with the administration of telmisartan, they were not significantly different when baseline cfPWV was considered. The differences in the cfPWV and LVMI changes from baseline between the two groups were also not significant after adjusting for baseline cfPWV. No significant changes in other vascular, metabolic, or inflammatory parameters were observed with either treatment.
CONCLUSION
The effects of a 12-week treatment with the two ARBs, telmisartan and valsartan, on cardiovascular, metabolic, and inflammatory parameters were not different in patients with uncomplicated hypertension.
Keyword
MeSH Terms
Figure
Reference
-
1. Sierra C, de la Sierra A. Antihypertensive, cardiovascular, and pleiotropic effects of angiotensin-receptor blockers. Curr Opin Nephrol Hypertens. 2005. 14:435–441.2. Mancia G, De Backer G, Dominiczak A, et al. 2007 guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2007. 28:1462–1536.3. Jung AD, Kim W, Park SH, et al. The effect of telmisartan on endothelial function and arterial stiffness in patients with essential hypertension. Korean Circ J. 2009. 39:180–184.4. Yusuf S, Sleight P, Pogue J, Bosch J, Davies R, Dagenais G. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients: the Heart Outcomes Prevention Evaluation Study Investigators. N Engl J Med. 2000. 342:145–153.5. Dahlöf B, Devereux RB, Kjeldsen SE, et al. Cardiovascular morbidity and mortality in the Losartan Intervention for Endpoint Reduction in Hypertension Study (LIFE): a randomized trial against atenolol. Lancet. 2002. 359:995–1003.6. Benson SC, Pershadsingh HA, Ho CI, et al. Identification of telmisartan as a unique angiotensin II receptor antagonist with selective PPAR-gamma-modulating activity. Hypertension. 2004. 43:993–1002.7. Schupp M, Janke J, Clasen R, Unger T, Kintscher U. Angiotensin type 1 receptor blockers induce peroxisome proliferator-activated receptor-gamma activity. Circulation. 2004. 109:2054–2057.8. Weiss D, Kools JJ, Taylor WR. Angiotensin II-induced hypertension accelerates the development of atherosclerosis in apoE-deficient mice. Circulation. 2001. 103:448–454.9. Koh KK, Ahn JY, Han SH, et al. Pleiotropic effects of angiotensin II receptor blocker in hypertensive patients. J Am Coll Cardiol. 2003. 42:905–910.10. Fliser D, Buchholz K, Haller H. Antiinflammatory effects of angiotensin II subtype 1 receptor blockade in hypertensive patients with microinflammation. Circulation. 2004. 110:1103–1107.11. Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985. 28:412–419.12. Hwang WM, Bae JH, Kim KY, Synn YC. Impacts of atherosclerotic coronary risk factors on atherosclerotic surrogates in patients with coronary artery disease. Korean Circ J. 2005. 35:131–139.13. Safar ME, Smulyan H. Measurements of arterial stiffness: are they ready for clinical use? Curr Cardiovasc Risk Rep. 2008. 2:268–273.14. Corretti MC, Anderson TJ, Benjamin EJ, et al. Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodil-ation of the brachial artery: a report of the International Brachial Ar-tery Reactivity Task Force. J Am Coll Cardiol. 2002. 39:257–265.15. Devereux RB, Alonso DR, Lutas EM, et al. Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy find-ings. Am J Cardiol. 1986. 57:450–458.16. Kim KI, Kim Y, Kim HJ, et al. Current status and characteristics of hypertension treatment by primary physicians in Korea: data from Ko-rean Epidemiology Study on Hypertension (KEY study). Am J Hypertens. 2008. 21:884–889.17. Neutel JM. Choosing among renin-angiotensin system blockers for the management of hypertension: from pharmacology to clinical efficacy. Curr Med Res Opin. 2010. 26:213–222.18. Smith DH, Cramer MJ, Neutel JM, Hettiarachchi R, Koval S. Comparison of telmisartan versus losartan: meta-analysis of titration-to-response studies. Blood Press Monit. 2003. 8:111–117.19. Lacourcière Y, Krzesinski JM, White WB, Davidai G, Schumacher H. Sustained antihypertensive activity of telmisartan compared with valsartan. Blood Press Monit. 2004. 9:203–210.20. Song HG, Kim EJ, Seo HS, et al. Relative contributions of different cardiovascular risk factors to significant arterial stiffness. Int J Cardiol. 2010. 139:263–268.21. Dhakam Z, McEniery CM, Yasmin , Cockcroft JR, Brown MJ, Wilkinson IB. Atenolol and eprosartan: differential effects on central blood pressure and aortic pulse wave velocity. Am J Hypertens. 2006. 19:214–219.22. Karalliedde J, Smith A, DeAngelis L, et al. Valsartan improves arterial stiffness in type 2 diabetes independently of blood pressure lowering. Hypertension. 2008. 51:1617–1623.23. Hirata K, Vlachopoulos C, Adji A, O'Rourke MF. Benefits from angiotensin-converting enzyme inhibitor 'beyond blood pressure lowering': beyond blood pressure or beyond the brachial artery? J Hypertens. 2005. 23:551–556.24. Yamamoto K, Mano T, Yoshida J, et al. ACE inhibitor and angiotensin II type 1 receptor blocker differently regulate ventricular fibrosis in hypertensive diastolic heart failure. J Hypertens. 2005. 23:393–400.25. Brooks WW, Bing OH, Robinson KG, Slawsky MT, Chaletsky DM, Conrad CH. Effect of angiotensin-converting enzyme inhibition on myocardial fibrosis and function in hypertrophied and failing myocardium from the spontaneously hypertensive rat. Circulation. 1997. 96:4002–4010.26. Ciulla MM, Paliotti R, Esposito A, et al. Different effects of antihypertensive therapies based on losartan or atenolol on ultrasound and biochemical markers of myocardial fibrosis: results of a randomized trial. Circulation. 2004. 110:552–557.27. Lang RM, Bierig M, Devereux RB, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005. 18:1440–1463.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of Telmisartan Compared with Valsartan on Plasma Adiponectin Levels and Arterial Stiffness in Patients with Type 2 Diabetes: A Pilot Study
- Comparison of effects of telmisartan versus valsartan on post-induction hypotension during noncardiac surgery: a prospective observational study
- Telmisartan-induced sprue-like enteropathy: a case report and a review of patients using non-olmesartan angiotensin receptor blockers
- Cardiac and kidney outcomes after sacubitril-valsartan therapy: recovery of cardiac function relative to kidney function decline
- Mixed?effects analysis of increased rosuvastatin absorption by coadministered telmisartan