Korean J Obstet Gynecol.
2010 Mar;53(3):254-263. 10.5468/kjog.2010.53.3.254.
The relationship between serum leptin level and metabolic syndrome in postmenopausal women
- Affiliations
-
- 1Department of Obstetrics and Gynecology, The Catholic University of Korea College of Medicine, Seoul, Korea. yolew@catholic.ac.kr
- KMID: 2273851
- DOI: http://doi.org/10.5468/kjog.2010.53.3.254
Abstract
OBJECTIVE
Menopause status may lead to increases of body fat, abdominal obesity, and the incidence of metabolic syndrome (MS). Leptin is an adipokine that is secreted by adipocytes and plays an important role in regulating energy homeostasis and the reproductive system. This study examined the relationship among obesity, MS, and serum leptin levels in pre- and postmenopausal women.
METHODS
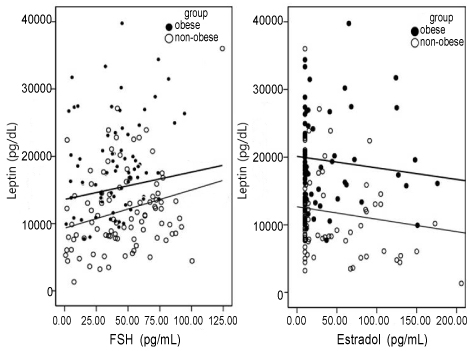
We divided 168 women who visited St. Vincent Hospital of the Catholic University of Korea in 2006 and 2007 into premenopausal vs. postmenopausal, obese vs. non-obese groups based on their body mass index (BMI) and the presence of MS. We measured serum follicle-stimulating hormone (FSH) level, serum estradiol level, BMI, the waist-hip ratio (WHR) and visceral fat area (VFA), serum fasting glucose, lipid profile, blood pressure, and serum leptin level.
RESULTS
Of 56 premenopausal and 112 postmenopausal women, there were 21 (37.5%) premenopausal and 51 (45.5%) postmenopausal women with MS. In the non-obese premenopausal and postmenopausal women, there were positive correlations between FSH, markers of abdominal obesity such as WHR and VFA, and serum leptin after adjusting for BMI in postmenopausal women. In the MS group, only WHR was correlated with the serum leptin level after adjusting for BMI in all groups.
CONCLUSION
Increased serum FSH level and abdominal obesity lead to an increased serum leptin level in postmenopausal women. Further studies are needed to clarify the relationship between leptin and the metabolic syndrome, risk of cardiovascular disease in postmenopausal women.
Keyword
MeSH Terms
-
Adipocytes
Adipokines
Adipose Tissue
Blood Pressure
Body Mass Index
Cardiovascular Diseases
Estradiol
Fasting
Female
Follicle Stimulating Hormone
Glucose
Homeostasis
Humans
Incidence
Intra-Abdominal Fat
Korea
Leptin
Menopause
Obesity
Obesity, Abdominal
Postmenopause
Waist-Hip Ratio
Adipokines
Estradiol
Follicle Stimulating Hormone
Glucose
Leptin
Figure
Cited by 1 articles
-
The effect of salt usage behavior on sodium intake and excretion among Korean women
Jeung Yun Lee, Dong Sook Cho, Hyun Ju Kim
Nutr Res Pract. 2012;6(3):232-237. doi: 10.4162/nrp.2012.6.3.232.
Reference
-
1. Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999-2000. JAMA. 2002. 288:1723–1727.
Article2. Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 2003. 348:1625–1638.
Article3. Bray GA. Medical consequences of obesity. J Clin Endocrinol Metab. 2004. 89:2583–2589.
Article4. Kuczmarski RJ, Flegal KM, Campbell SM, Johnson CL. Increasing prevalence of overweight among US adults. The National Health and Nutrition Examination Surveys, 1960 to 1991. JAMA. 1994. 20:205–211.
Article5. Poehlman ET, Toth MJ, Gardner AW. Changes in energy balance and body composition at menopause: a controlled longitudinal study. Ann Intern Med. 1995. 123:673–675.6. Pasquali R, Casimirri F, Labate AM, Tortelli O, Pascal G, Anconetani B, et al. Body weight, fat distribution and the menopausal status in women. The VMH Collaborative Group. Int J Obes Related Metab Disord. 1994. 18:614–621.7. Björkelund C, Lissner L, Andersson S, Lapidus L, Bengtsson C. Reproductive history in relation to relative weight and fat distribution. Int J Obes Related Metab Disord. 1996. 20:213–219.8. Carr MC. The emergence of the metabolic syndrome with menopause. J Clin Endocrinol Metab. 2003. 88:2404–2411.
Article9. Lindheim SR, Buchanan TA, Duffy DM, Vijod MA, Kojima T, Stanczyk FZ, et al. Comparison of estimates of insulin sensitivity in pre- and postmenopausal women using the insulin tolerance test and the frequently sampled intravenous glucose tolerance test. J Soc Gynecol Investig. 1994. 1:150–154.10. Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among U.S. adults: findings from the third National Health and Nutrition Examination Survey. JAMA. 2002. 287:356–359.
Article11. Malik S, Wong ND, Franklin SS, Kamath TV, L'Italien GJ, Pio JR, et al. Impact of the metabolic syndrome on mortality from coronary heart disease, cardiovascular disease, and all causes in United States adults. Circulation. 2004. 110:1245–1250.
Article12. Després JP. Abdominal obesity as important component of insulin resistance syndrome. Nutrition. 1993. 9:452–459.13. Kannel WB, Cupples LA, Ramaswami R, Stokes J 3rd, Kreger BE, Higgins M. Regional obesity and risk of cardiovascular disease; the Framingham Study. J Clin Epidemiol. 1991. 44:183–190.
Article14. Prins JB, Adipose tissue. Adipose tissue as an endocrine organ. Best Pract Res Clin Endocrinol Metab. 2002. 16:639–651.
Article15. Caro JF, Sinha MK, Kolaczynski JW, Zhang PL, Considine RV. Leptin: the tale of an obesity gene. Diabetes. 1996. 45:1455–1462.
Article16. Nagatani S, Guthikonda P, Thompson RC, Tsukamura H, Maeda KI, Foster DL. Evidence for GnRH regulation by leptin: leptin administration prevents reduced LH secretion during fasting. Neuroendocrinology. 1998. 67:370–376.17. Duggal PS, Van Der Hoek KH, Milner CR, Ryan NK, Armstrong DT, Magoffin DA, et al. The in vivo and in vitro effects of exogenous leptin on ovulation in the rat. Endocrinology. 2000. 141:1971–1976.
Article18. Agarwal SK, Vogel K, Weitsman SR, Magoffin DA. Leptin antagonizes the insulin-like growth factor-I augmentation of steroidogenesis in granulose and theca cells of the human ovary. J Clin Endocrinol Metab. 1999. 84:1072–1076.19. Soules MR, Sherman S, Parrott E, Rebar R, Santoro N, Utian W, et al. Executive summary: Stages of Reproductive Aging Workshop (STRAW). Fertil Steril. 2001. 76:874–878.
Article20. Examination Committee of Criteria for 'Obesity Disease' in Japan. Japan Society for the Study of Obesity. New criteria for 'obesity disease' in Japan. Circ J. 2002. 66:987–992.21. Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med. 1998. 15:539–553.
Article22. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002. 106:3143–3421.24. Gambacciani M, Ciaponi M, Cappagli B, De Simone L, Orlandi R, Genazzani AR. Prospective evaluation of body weight and body fat distribution in early postmenopausal women with and without hormonal replacement therapy. Maturitas. 2001. 39:125–132.
Article25. Lovejoy JC, Champagne CM, de Jonge L, Xie H, Smith SR. Increased visceral fat and decreased energy expenditure during the menopausal transition. Int J Obes (Lond). 2008. 32:949–958.
Article26. Park YW, Zhu S, Palaniappan L, Heshka S, Carnethon MR, Heymsfield SB. The metabolic syndrome: prevalence and associated risk factor findings in the US population from the Third National Health and Nutrition Examination Survey, 1988-1994. Arch Intern Med. 2003. 163:427–436.27. Zhang Y, Proenca R, Maffei M, Barone M, Leopold L, Friedman J. Positional cloning of the mouse obese gene and its human homologue. Nature. 1994. 372:425–432.
Article28. Hileman SM, Pierroz DD, Flier JS. Leptin, nutrition, and reproduction: Timing is everything. J Clin Endocrinol Metab. 2000. 85:804–807.
Article29. Friedman JM, Halaas JL. Leptin and the regulation of body weight in mammals. Nature. 1998. 395:763–770.
Article30. Buettner C, Muse ED, Cheng A, Chen L, Scherer T, Pocai A, et al. Letpin controls adipose tissue lipogenesis via central, STAT3-independent mechanisms. Nat Med. 2008. 14:667–675.31. Greco AV, Mingrone G, Giancaterini A, Manco M, Morroni M, Cinti S, et al. Insulin resistance in morbid obesity: reversal with intramyocellular fat depletion. Diabetes. 2002. 51:144–151.
Article32. Buettner C, Pocai A, Muse ED, Etgen AM, Myers MG Jr, Rossetti L. Critical role of STAT3 in leptin's metabolic actions. Cell Metabol. 2006. 4:49–60.
Article33. Wallace AM, McMahon AD, Packard CJ, Kelly A, Shepherd J, Gaw A, et al. Plasma leptin and the risk of cardiovascular disease in the west of Scotland coronary prevention study (WOSCOPS). Circulation. 2001. 104:3052–3056.
Article34. Moschos S, Chan JL, Mantzoros CS. Leptin and reproduction: a review. Fertil Steril. 2002. 77:433–444.
Article35. Shimizu H, Shimomura Y, Nakanishi Y, Futawatari T, Ohtani K, Sato N, et al. Estrogen increases in vivo leptin production in rats and human subjects. J Endocrinol. 1997. 154:285–292.
Article36. Chu MC, Cosper P, Orio F, Carmina E, Lobo RA. Insulin resistance in postmenopausal women with metabolic syndrome and the measurements of adiponectin, leptin, resistin, ghrelin. Am J Obstet Gynecol. 2006. 194:100–104.37. Sowers MR, Wildman RP, Mancuso P, Eyvazzadeh AD, Kaovonen-Gutierrez CA, Rillamas-Sun E, et al. Change in adipocytokines and ghrelin with menopause. Maturitas. 2008. 59:149–157.
Article38. Lapidus L, Bengtsson C, Larsson B, Pennert K, Rybo E, Sjöström L. Distribution of adipose tissue and risk of cardiovascular disease and death: a 12 year follow up of participants in the population study of women in Gothenburg. Br Med J (Clin Res Ed). 1984. 289:1257–1261.39. Mahabir S, Baer D, Johnson LL, Roth M, Campbell W, Clevidence B, et al. Body mass index, percent body fat and regional body fat distribution in relation to leptin concentrations in healthy, non-smoking postmenopausal women in a feeding study. Nutr J. 2007. 6:3.
Article40. Ritland LM, Alekel DL, Matvienko OA, Hanson KB, Stewart JW, Hanson LN, et al. Centrally located body fat is related to appetitive hormones in healthy postmenopausal women. Eur J Endocriol. 2008. 158:889–897.
Article41. Huang KC, Lin RC, Kormas N, Lee LT, Chen CY, Gill TP, et al. Plasma leptin is associated with insulin resistance independent of age, body mass index, fat mass, lipid and pubertal development in nondiabetic adolescents. Int J Obes Relat Metab Disord. 2004. 28:470–475.42. Franks PW, Brage S, Luan J, Ekelund U, Rahman M, Farooqi S, et al. Leptin predicts a worsening of the feature of the metabolic syndrome independently of obesity. Obes Res. 2005. 13:1476–1484.43. Wellen KE, Hotamisligil GS. Obesity-induced inflammatory changes in adipose tissue. J Clin Invest. 2003. 112:1785–1788.
Article44. Patel SB, Reams GP, Spear RM, Freeman RH, Villarreal D. Leptin: linking obesity, the metabolic syndrome, and cardiovascular disease. Curr Hypertens Rep. 2008. 10:131–137.
Article45. Ryo M, Maeda K, Onda T, Katashima M, Okumiya A, Nishida M, et al. A new simple method for the measurement of visceral fat accumulation by bioelectrical impedance. Diabetes Care. 2005. 28:451–453.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Association between Serum Leptin Concentration and Bone Mineral Density in Healthy Korean Women
- Relationship between serum leptin level and bone mineral density and bone markers in postmenopausal women
- Effect of postmenopausal hormone replecement therapy on leptin level and body composition
- Serum Leptin Levels in Relation to Quantitative Ultrasound Values of Calcaneus in Korean Postmenopausal Women in Chung-Up District
- The Relations between Bone Density and Plasma Leptin in Postmenopausal Women