Ann Rehabil Med.
2012 Aug;36(4):433-446. 10.5535/arm.2012.36.4.433.
The Impacts of ACE Activity according to ACE I/D Polymorphisms on Muscular Functions of People Aged 65
- Affiliations
-
- 1Department of Rehabilitation Medicine, Hallym University College of Medicine, Seoul 134-701, Korea. imdrnam@gmail.com
- 2Department of Physiology and Biophysics, Antiaging Research Center, School of Medicine, Eulji University, Daejeon 301-832, Korea.
- 3Department of Physical Therapy, Hallym College, Chuncheon 200-711, Korea.
- KMID: 2266713
- DOI: http://doi.org/10.5535/arm.2012.36.4.433
Abstract
OBJECTIVE
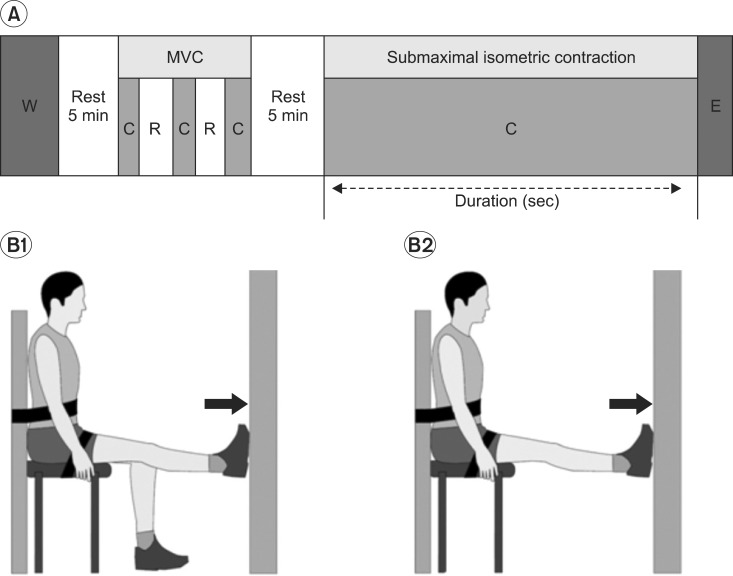
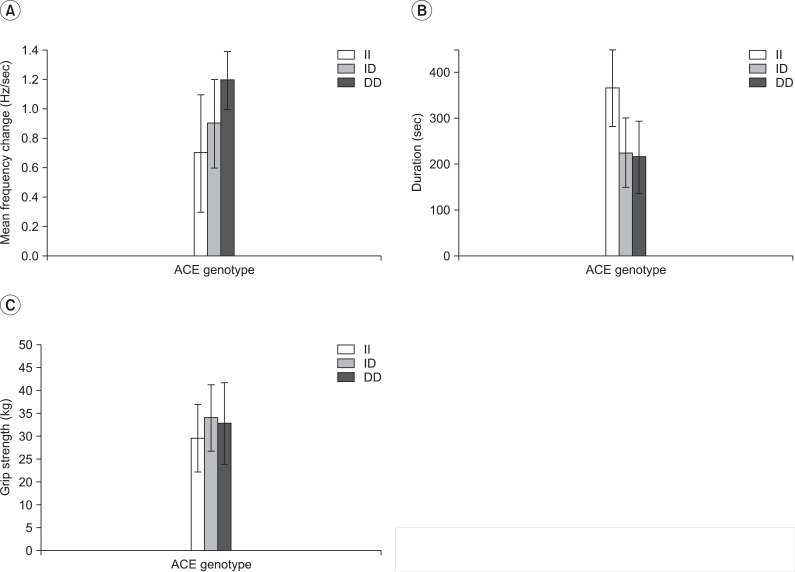
To investigate associations between angiotensin-converting enzyme (ACE) polymorphisms and muscle fatigability in 65-year-old Koreans. METHOD: The study participants were 49 Koreans aged 65 years. ACE insertion/deletion (I/D) polymorphisms were determined by polymerase chain reaction and serum ACE activity, by spectrophotometry. Body mass index (BMI), body fat mass (BFM), and lean body mass (LBM) were determined. To evaluate muscle fatigability, dynamic Electromyography was used to measure maximum voluntary isometric contractions (MVICs) of ankle plantar flexor muscles. Patients were seated with their hips flexed at 90degrees, knees fully extended, and ankles at 0degrees. Continuous submaximal VICs (40% MVIC) were then performed, and contraction duration and EMG frequency changes during the initial 2 min were measured. A self-reported physical activity questionnaire was used to evaluate effects of ACE activity levels on muscle fatigability.
RESULTS
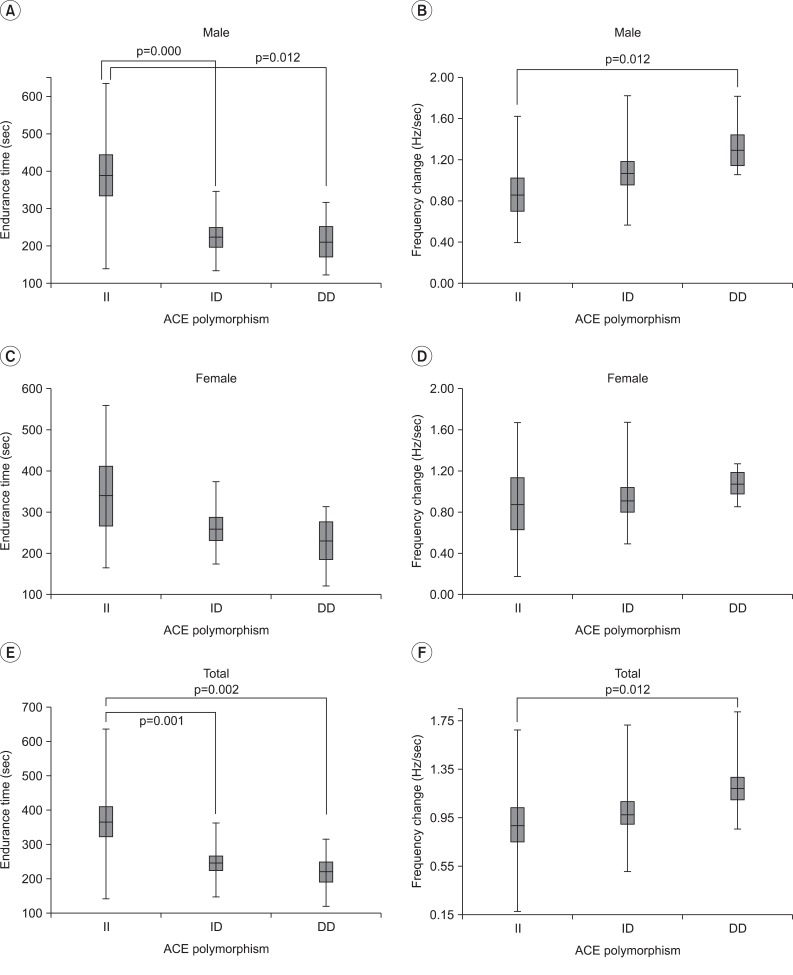
Among the 49 volunteers, 15 showed II genotype; 22, ID genotype; and 12, DD genotype. Serum ACE activity levels were significantly higher in DD genotype subjects than in II genotype subjects (p<0.05). Furthermore, the duration of submaximal isometric contractions was longer in II and ID genotype subjects than in DD genotype subjects (p<0.05). Dynamic EMG showed significantly lower mean frequency changes in II genotype subjects than in DD genotype subjects (p<0.05). However, LBM, BFM, and BMI were independent of ACE genotypes.
CONCLUSION
ACE II genotype subjects showed significantly higher resistant to muscle fatigue than that by DD genotype subjects. However, body composition and BMI showed no correlations with ACE I/D polymorphisms.
MeSH Terms
Figure
Reference
-
1. Rankinen T, Bray MS, Hagberg JM, Pérusse L, Roth SM, Wolfarth B, Bouchard C. The human gene map for performance and health-related fitness phenotypes: the 2005 update. Med Sci Sports Exerc. 2006; 38:1863–1888. PMID: 17095919.2. Myerson SG, Hemingway H, Budget R, Martin J, Humphries S, Montogmery H. Human angiotensin I-converting enzyme gene and endurance performance. J Appl Physiol. 1999; 87:1313–1316. PMID: 10517757.3. Nazarov IB, Woods DR, Monthomery HE, Shneider OV, Kazakov VI, Tomilin NT, Rogozkin VA. The angiotensin converting enzyme I/D polymorphism in Russian athletes. Eur J Hum Genet. 2001; 9:797–801. PMID: 11781693.
Article4. Woods D, Hickman M, Jamshidi Y, Brull D, Vassiliou V, Jones A, Humphries S, Montgomery H. Elite swimmers and the D allele of the ACE I/D polymorphism. Hum Genet. 2001; 108:230–232. PMID: 11354635.
Article5. Vigano A, Trutschnigg B, Kilgour RD, Hamel N, Hornby L, Lucar E, Foulkes W, Tremblay ML, Morais JA. Relationship between angiotensin-converting enzyme gene polymorphism and body composition, functional performance, and blood biomarkers in advanced cancer patients. Clin Cancer Res. 2009; 15:2442–2447. PMID: 19258445.
Article6. Rigat B, Hubert C, Alhenc-Gelas F, Cambien F, Corvol P, Soubrier F. An insertion/deletion polymorphism in the angiotensin I-converting enzyme gene accounting for half the variance of serum enzyme levels. J Clin Invest. 1990; 86:1343–1346. PMID: 1976655.
Article7. Dietze GJ, Henriksen EJ. Angiotensin-converting enzyme in skeletal muscle: sentinel of blood pressure control and glucose homeostasis. J Renin Angiotensin Aldosterone Syst. 2008; 9:75–88. PMID: 18584583.8. Alvarez R, Terrados N, Ortolano R, Iglesias-Cubero G, Reguero JR, Batalla A, Cortina A, Fernández-García B, Rodríguez C, Braga S, et al. Genetic variation in the renin-angiotensin system and athletic performance. Eur J Appl Physiol. 2000; 82:117–120. PMID: 10879452.
Article9. Sanders PM, Russell ST, Tisdale MJ. Angiotensin II directly induces muscle protein catabolism through the ubiquitin-proteasome proteolytic pathway and may play a role in cancer cachexia. Br J Cancer. 2005; 93:425–434. PMID: 16052213.
Article10. Greenlund LJ, Nair KS. Sarcopenia-consequences, mechanisms, and potential therapies. Mech Ageing Dev. 2003; 124:287–299. PMID: 12663126.
Article12. Sumukadas D, Struthers AD, McMurdo ME. Sarcopenia-a potential target for Angiotensin-converting enzyme inhibition? Gerontology. 2006; 52:237–242. PMID: 16849867.13. Basmajian JV, De Luca CJ. Muscles alive-their functions revealed by electromyography. 1985. 5th ed. Baltimore: Williams & Wilkins;p. 201–220.14. Ali A, Vasudevan R, Ismail P, Thiam Seong CL, Chakravarthi S. Analysis of insertion/deletion polymorphisms of the angiotensin converting enzyme gene in Malaysian end-stage renal disease patients. J Renin Angiotensin Aldosterone Syst. 2011; 18:1–7.
Article15. Kasahara Y, Ashihara Y. Colorimetry of angiotensin-l converting enzyme activity in serum. Clin Chem. 1981; 27:1922–1925. PMID: 6271420.16. Rantanen T, Era P, Kauppinen M, Heikkinen E. Maximal isometric muscle strength and socioeconomic status, health, and physical activity in 75-year-old persons. J Aging Phys Act. 1994; 2:206–220.
Article17. Vandervoort AA, Hayes KC, Belanger AY. Strength and endurance of skeletal muscle in the elderly. Physiotherapy Canada. 1986; 38:167–173.
Article18. Wilder RP, Greene JA, Winters KL, Long WB 3rd, Gubler K, Edlich RF. Physical fitness assessment: an update. J Long Term Eff Med Implants. 2006; 16:193–204. PMID: 16700660.
Article19. Nordez A, Guével A, Casari P, Catheline S, Cornu C. Assessment of muscle hardness changes induced by a submaximal fatiguing isometric contraction. J Electromyogr Kinesiol. 2009; 19:484–491. PMID: 18158253.
Article20. Hermens HJ, Freriks B, Disselhorst-Klug C, Rau G. Development of recommendations for SEMG sensors and sensor placement procedures. J Electromyogr Kinesiol. 2000; 10:361–374. PMID: 11018445.
Article21. Jun AY, Choi EH, Yoo YS, Park DS, Nam HS. The activities of trapezius and deltoid in rotator cuff tear patients injected local anesthetics in subacromial space. J Korean Acad Rehabil Med. 2010; 34:316–324.22. Mademli L, Arampatzis A. Behaviour of the human gastrocnemius muscle architecture during submaximal isometric fatigue. Eur J Appl Physiol. 2005; 94:611–617. PMID: 15906075.
Article23. Choe MA, Kim J, Jeon MY, Chae YR. Evaluation of the Korean version of physical activity scale for the elderly (K-PASE). Korean J Women Health Nurs. 2010; 16:47–59.
Article24. Jones A, Montgomery HE, Woods DR. Human performance: a role for the ACE genotype? Exerc Sport Sci Rev. 2002; 30:184–190. PMID: 12398116.
Article25. Frederiksen H, Gaist D, Bathum L, Andersen K, McGue M, Vaupel JW, Christensen K. Angiotensin I-converting enzyme (ACE) gene polymorphism in relation to physical performance, cognition and survival--a follow-up study of elderly Danish twins. Ann Epidemiol. 2003; 13:57–65. PMID: 12547486.
Article26. Tobina T, Ayabe M, Yoshitake Y, Kimura Y, Miyazaki H, Ishii K, Zhang B, Saku K, Shindo M, Kiyonaga A, et al. Relationship between angiotensin converting enzyme gene I/D polymorphism and muscle strength in elderly. International Journal of Sport and Health Science. 2006; 4:460–464.
Article27. Laforest S, St-Pierre DM, Cyr J, Gayton D. Effects of age and regular exercise on muscle strength and endurance. Eur J Appl Physiol Occup Physiol. 1990; 60:104–111. PMID: 2335167.
Article28. Ng JK, Richardson CA. Reliability of electromyographic power spectral analysis of back muscle endurance in healthy subjects. Arch Phys Med Rehabil. 1996; 77:259–264. PMID: 8600868.
Article29. Edwards RH. Human muscle function and fatigue. Ciba Found Symp. 1981; 82:1–18. PMID: 6117420.
Article30. Tesch PA, Komi PV, Jacobs I, Karlsson J, Viitasalo JT. Influence of lactate accumulation of EMG frequency spectrum during repeated concentric contractions. Acta Physiol Scand. 1983; 119:61–67. PMID: 6650206.
Article31. Mannion AF, Dolan P. Electromyographic median frequency changes during isometric contraction of the back extensors to fatigue. Spine. 1994; 19:1223–1229. PMID: 8073313.
Article32. Merletti R, Roy S. Myoelectric and mechanical manifestations of muscle fatigue in voluntary contractions. J Orthop Sports Phys Ther. 1996; 24:342–353. PMID: 8938600.
Article33. Hagberg M. Muscular endurance and surface electromyogram in isometric and dynamic exercise. J Appl Physiol. 1981; 51:1–7. PMID: 7263402.
Article34. Fuglevand AJ, Zackowski KM, Huey KA, Enoka RM. Impairment of neuromuscular propagation during human fatiguing contractions at submaximal forces. J Physiol. 1993; 460:549–572. PMID: 8387589.
Article35. Garg A, Hegmann KT, Schwoerer BJ, Kapellusch JM. The effect of maximum voluntary contraction on endurance times for the shoulder girdle. International Journal of Industrial Ergonomics. 2002; 30:103–113.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Study on Angiotensin Converting Enzyne Activity in Pulmonary Tuberculosis
- An I/D Polymorphism in Angiotensin-Converting Enzyme Gene in Myocardial Infarction
- Angiotensin Converting Enzyme (ACE) in Serum and Bronchoalveolar Lavage (BAL) Fluid in Patients with Active Pulmonary Tuberculosis
- Angiotensin Converting Enzyme in Human Adult Respiratory Distress Syndrome
- Association of Angiotensin-converting Enzyme Gene Polymorphism with the Disease Activity of Systemic Lupus Erythematosus in Korean Children