Korean J Hematol.
2009 Dec;44(4):249-254. 10.5045/kjh.2009.44.4.249.
t(9;22) with 5'ABL1 Deletion and t(6;19) in Biphenotypic Acute Leukemia
- Affiliations
-
- 1Department of Laboratory Medicine, Gachon University Gil Hospital, Incheon, Korea. jyahn@gilhospital.com
- 2Department of Laboratory Medicine, University of Ulsan College of Medicine and Asan Medical Center, Seoul, Korea.
- KMID: 2252104
- DOI: http://doi.org/10.5045/kjh.2009.44.4.249
Abstract
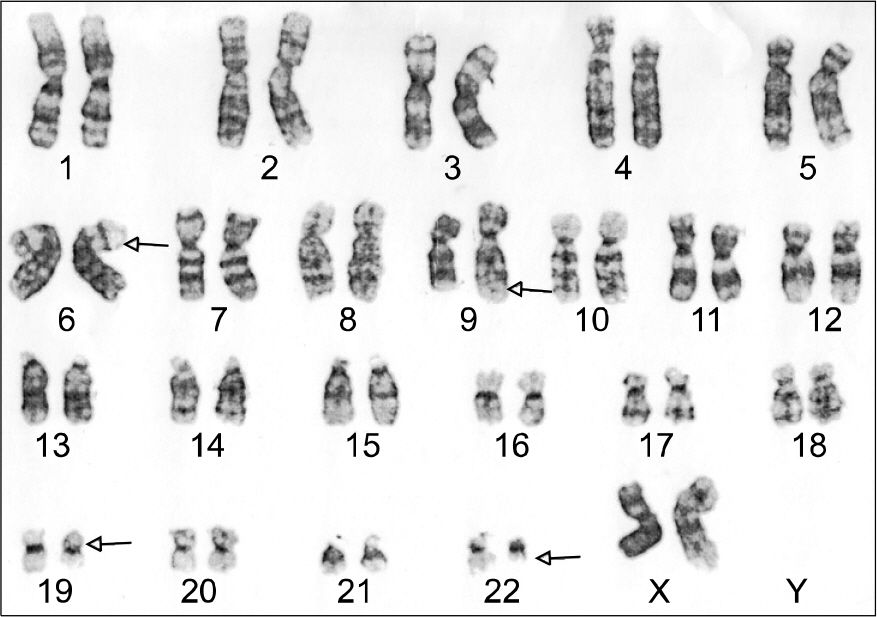
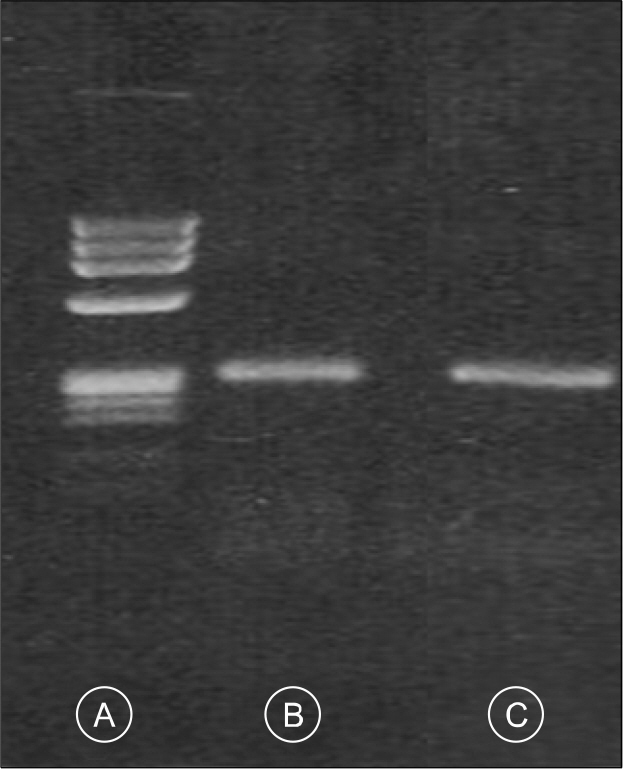
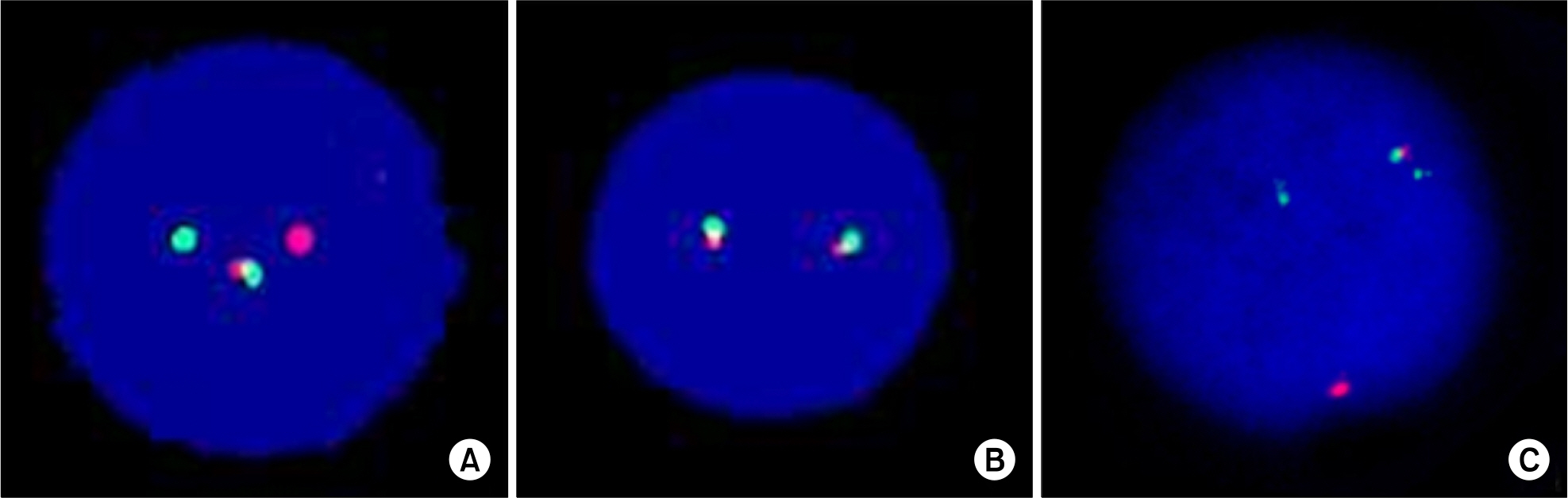
- Biphenotypic acute leukemia (BAL) is a rare type of leukemia, comprises 4% of all acute leukemias. It is more common in adults and the clinical features, as related to marrow dysfunction, are similar to those found in other patients with acute leukemia. BAL commonly shows a dimorphic blast population with, one resembling lymphoblasts and the other resembling myeloblasts. The majority of BAL patients express B-lymphoid and myeloid markers. BAL can be diagnosed by morphologic studies and by a comprehensive panel of immunological markers, as well as cytogenetic/molecular studies, such as fluorescence in situ hybridization (FISH) and reverse transcriptase-polymerase chain reaction (RT-PCR). In addition, its prognosis is relatively poor. We present here a 27 year-old female patient who showed lymphoblasts and myeloblasts on her marrow studies and these cells were positive for myeloid and B-lymphoid markers on the immunophenotypic studies. Chromosome analysis revealed 46,XX,t(6;19)(p23;p13.1),t(9;22)(q34;q11.2). A major (b3a2) type of BCR-ABL1 mRNA transcript was detected by RT-PCR, and a 5'ABL1 deletion was identified by FISH.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Choi HW, Shin MG, Kim HJ, et al. Biphenotypic acute leukemia with BCR-ABL mRNA transcript b3a2 type: a case report with review of the literature. Korean J Lab Med. 2006; 26:249–54.2. Shaffer LG, Slovak ML, Campbell LJ, eds. ISCN (2009) An International System for Human Cytogenetic Nomenclature. Basel: Karger. 2009.3. Lee DS. Acute leukemia of ambiguous lineage. The Korean Society for Laboratory Medicine, editor. The Laboratory Medicine. 4th ed.Reston: E-Public;2009. p. 198–9.
Article4. Borowitz MJ, bene MC, Harris NL, Porwit A, Matutes E. Acute leukaemias of ambiguous lineage. Swerdlow SH, Campo E, Harris NL, editors. WHO classification of tumours of haematopoietic and lymphoid tissues. 4th ed.Lyon: IARC Press;2006. p. 150–2.5. Legrand O, Perrot JY, Simonin G, et al. Adult biphenotypic acute leukaemia: an entity with poor prognosis which is related to unfavourable cytogenetics and P-glycoprotein over-expression. Br J Haematol. 1998; 100:147–55.
Article6. Cuneo A, Ferrant A, Michaux JL, et al. Philadelphia chromosome-positive acute myeloid leukemia: cy-toimmunologic and cytogenetic features. Haematologica. 1996; 81:423–7.7. Montgomery KD, Winter SS, Frost JD, et al. Myeloid antigen positive acute lymphoblastic leukemia with the philadelphia translocation and a jumping translocation of 1q in a child. Leukemia. 2004; 18:1548–50.
Article8. Shin S, Park SS, Cho HI, Hur MN, Lee YJ. Analysis of breakpoints of bcr-abl fusion gene using RT-PCR. Korean J Lab Med. 1999; 19:369–74.9. Park TS, Lee ST, Song JW, et al. Biphenotypic acute leukemia with b2a2 fusion transcript and trisomy 21. Cancer Genet and Cytogenet. 2009; 188:129–31.
Article10. Kim YK, Lee JJ, Lee BH, et al. Successful autologous peripheral blood stem cell transplantation after molecular remission using imatinib mesalate in a patient with philadelphia chromosome-positive acute myeloid leukemia. Korean J Hemato Stem Cell Trans. 2003; 8:55–8.11. Morel F, KA C, Le Bris MJ, et al. Deletion of 5'ABL region in philadelphia chromosome-positive chronic myeloid leukemia: frequency, origin and prognosis. Leuk Lymphoma. 2003; 44:1333–8.12. Huntly BJP, Guilhot F, Reid AG, et al. Imatinib improves but may not fully reverse the poor prognosis of patients with CML with derivative chromosome 9 deletions. Blood. 2003; 102:2205–12.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Acute Promyelocytic Leukemia with Co-existence of BCR-ABL1 and PML-RARA Rearrangements Detected by PCR
- A case report of adult acute biphenotypic leukemia-hand mirror variant
- A case of biphenotypic acute leukemia with expression of the AML1-ETO gene rearrangement
- A case of bullous pyoderma gangrenosum associated with refractory acute biphenotypic leukemia
- Relapse of Biphenotypic Acute Leukemia as a Breast Mass