J Rheum Dis.
2014 Aug;21(4):214-218. 10.4078/jrd.2014.21.4.214.
Pulmonary Cryptococcosis in a Patient with Ankylosing Spondylitis treated with Etanercept
- Affiliations
-
- 1Department of Internal Medicine, Konkuk University School of Medicine, Seoul, Korea.
- 2Division of Rheumatology, Department of Internal Medicine, Konkuk University School of Medicine, Seoul, Korea. kimhaerim@kuh.ac.kr
- 3Department of Pathology, Konkuk University School of Medicine, Seoul, Korea.
- KMID: 2222965
- DOI: http://doi.org/10.4078/jrd.2014.21.4.214
Abstract
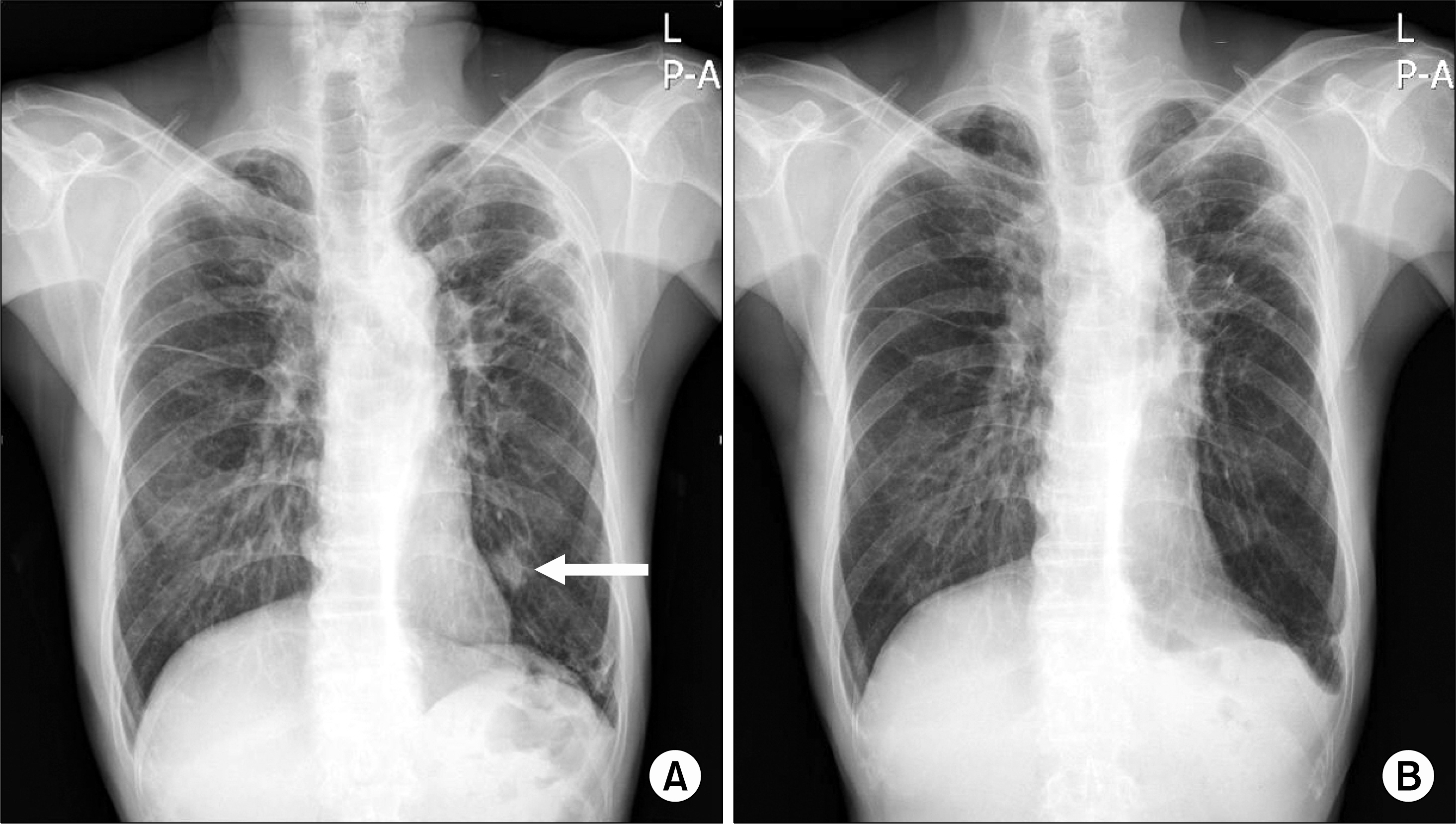
- Ankylosing spondylitis (AS) is a chronic inflammatory disorder, commonly characterized by inflammation of axial skeleton and development of enthesopathies. Tumor necrosis factor inhibitors (TNFi) shows good therapeutic responses in AS patients without good response to non-steroidal anti-inflammatory drugs. Although TNFi are relatively safe for AS patients, serious opportunistic infections, including tuberculosis and fungal infection, could develop. Here, according to our knowledge, we report a first Korean case of pulmonary cryptococcosis in a patient with AS treated with etanercept. A 64 year-old man with AS visited due to a newly appeared pulmonary nodule on a routine chest radiography. He had been administered etanercept for 5 months. Histologic findings of the lung nodule showed characteristic features of cryptococcosis. Etanercept was discontinued and oral fluconazole was administrated, as there was no evidence of central nervous system involvement. After 7 months of treatment, chest CT showed an improvement of the pulmonary lesion.
Keyword
MeSH Terms
Figure
Reference
-
1. Gorman JD, Sack KE, Davis JC Jr. Treatment of ankylosing spondylitis by inhibition of tumor necrosis factor alpha. N Engl J Med. 2002; 346:1349–56.2. Baddley JW, Winthrop KL, Chen L, Liu L, Grijalva CG, Delzell E, et al. Non-viral opportunistic infections in new users of tumour necrosis factor inhibitor therapy: results of the SAfety Assessment of Biologic ThERapy (SABER) Study. Ann Rheum Dis. In press. 2013.3. Bergstrom L, Yocum DE, Ampel NM, Villanueva I, Lisse J, Gluck O, et al. Increased risk of coccidioidomycosis in patients treated with tumor necrosis factor alpha antagonists. Arthritis Rheum. 2004; 50:1959–66.4. Hoang JK, Burruss J. Localized cutaneous Cryptococcus albidus infection in a 14-year-old boy on etanercept therapy. Pediatr Dermatol. 2007; 24:285–8.
Article5. Braun J, van den Berg R, Baraliakos X, Boehm H, Burgos-Vargas R, Collantes-Estevez E, et al. 2010 update of the ASAS/EULAR recommendations for the management of ankylosing spondylitis. Ann Rheum Dis. 2011; 70:896–904.
Article6. Machado MA, Barbosa MM, Almeida AM, de Araújo VE, Kakehasi AM, Andrade EI, et al. Treatment of ankylosing spondylitis with TNF blockers: a meta-analysis. Rheumatol Int. 2013; 33:2199–213.
Article7. Mazza J, Rossi A, Weinberg JM. Innovative uses of tumor necrosis factor alpha inhibitors. Dermatol Clin. 2010; 28:559–75.8. Berry MA, Hargadon B, Shelley M, Parker D, Shaw DE, Green RH, et al. Evidence of a role of tumor necrosis factor alpha in refractory asthma. N Engl J Med. 2006; 354:697–708.9. Dalakas MC. Novel future therapeutic options in myas-thenia gravis. Autoimmun Rev. 2013; 12:936–41.
Article10. Tsiodras S, Samonis G, Boumpas DT, Kontoyiannis DP. Fungal infections complicating tumor necrosis factor alpha blockade therapy. Mayo Clin Proc. 2008; 83:181–94.11. Salmon-Ceron D, Tubach F, Lortholary O, Chosidow O, Bretagne S, Nicolas N, et al. RATIO group. Drug-specific risk of non-tuberculosis opportunistic infections in patients receiving anti-TNF therapy reported to the 3-year prospective French RATIO registry. Ann Rheum Dis. 2011; 70:616–23.
Article12. Park HS, Lee JB, Park JY, Shim KN, Sung YA, Koo HS, et al. A Case of Esophageal Aspergillosis Developed in Patient with Rheumatoid Arthritis. Infect Chemother. 2007; 39:327–31.13. Lee KS, Lee HY, Lee SW, Jung HJ, Song JS. A Case of Candida Bursitis Associated with Etanercept Treatment in a Patient with Rheumatoid Arthritis. J Korean Rheum Assoc. 2008; 15:175–9.
Article14. Jonathan C, William GP, Steven MO. Infectious Diseases. 3rd ed.p. 1823–52. Edinburgh: Mosby Elsevier;2010.15. Strangfeld A, Eveslage M, Schneider M, Bergerhausen HJ, Klopsch T, Zink A, et al. Treatment benefit or survival of the fittest: what drives the time-dependent decrease in serious infection rates under TNF inhibition and what does this imply for the individual patient? Ann Rheum Dis. 2011; 70:1914–20.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- TNF Inhibitors and Uveitis in Ankylosing Spondylitis
- A Case of Ankylosing Spondylitis Accompanying Sarcoidosis
- Etanercept Treatment in Ankylosing Spondylitis Hip Lesions
- IgA nephropathy in a patient with ankylosing spondylitis well controlled with etanercept
- A Case of Varicelliform Zoster in a Patient Treated with Etanercept for Ankylosing Spondylitis