J Rheum Dis.
2015 Jun;22(3):154-166. 10.4078/jrd.2015.22.3.154.
Compound K, a Metabolite of Ginsenosides, Attenuates Collagen-induced Arthritis in Mice
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University Bundang Hospital, Seongnam, Korea.
- 2Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea.
- 3Department of Dermatology and Histopathology, College of Medicine, Chung-Ang University, Seoul, Korea.
- 4Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea. ysong@snu.ac.kr
- 5Metabolab Inc., Cancer Research Institute, Seoul National University College of Medicine, Seoul, Korea.
- 6Department of Molecular Medicine and Biopharmaceutical Sciences, Graduate School of Convergence Science and Technology, Medical Research Center, Seoul National University, Seoul, Korea.
- KMID: 2222881
- DOI: http://doi.org/10.4078/jrd.2015.22.3.154
Abstract
OBJECTIVE
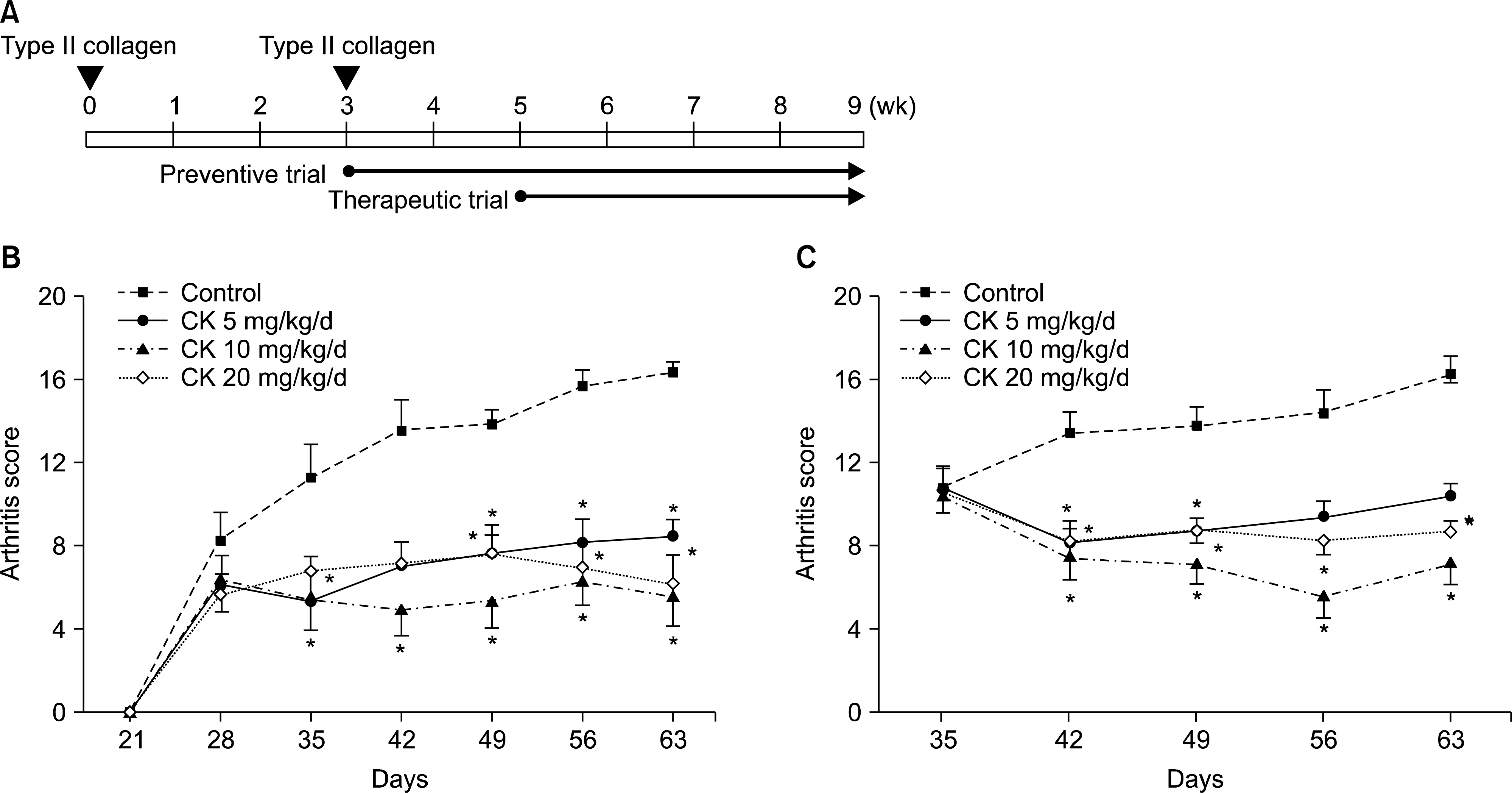
Although several ginsenosides have been reported to have anti-arthritic activity, few in vivo studies of the anti-arthritic effects of compound K (CK), a major metabolite of ginsenosides, have been conducted. Therefore, we investigated the preventative and therapeutic effects of CK on collagen-induced arthritis (CIA).
METHODS
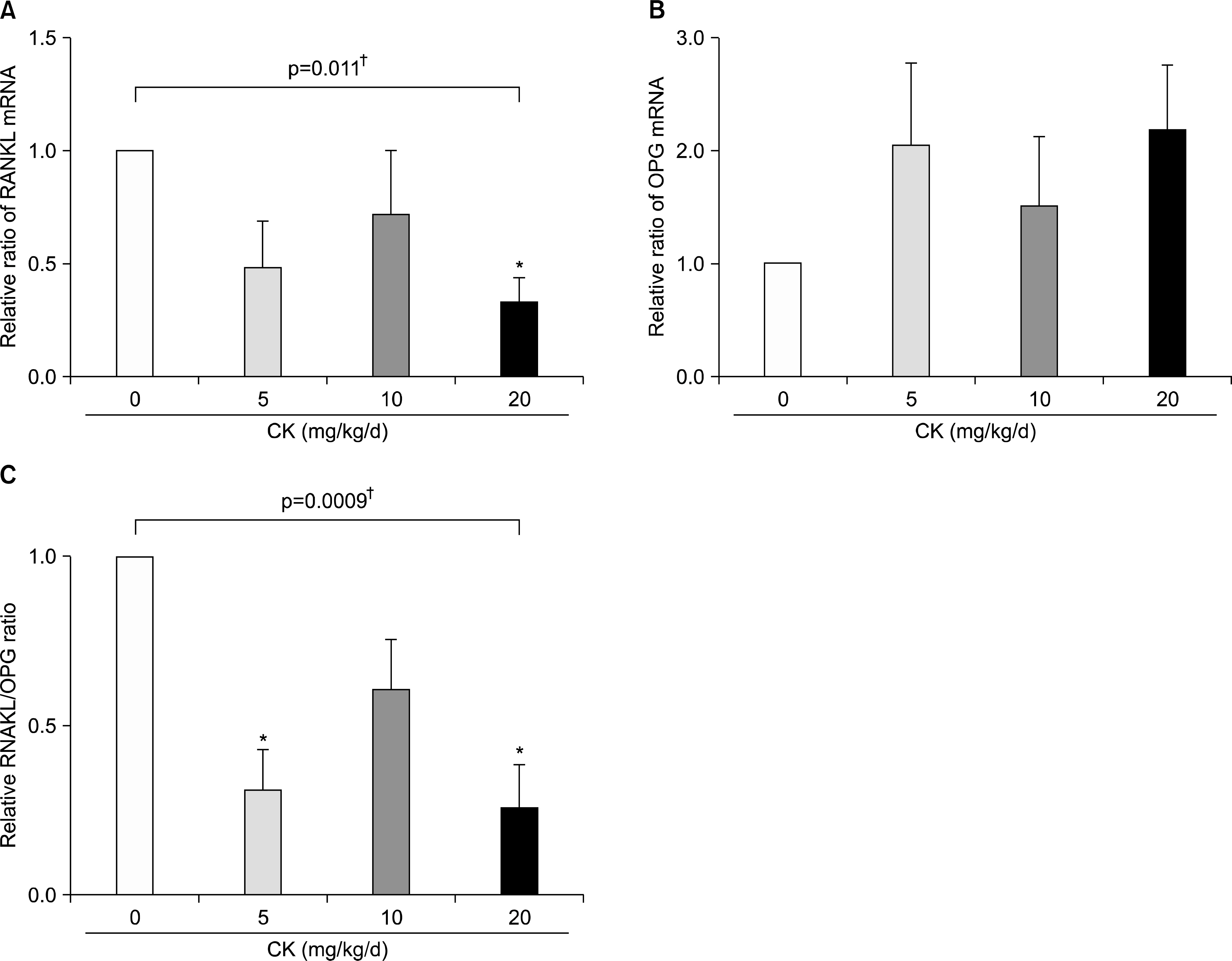
CK was administered to CIA mice preventively and therapeutically and post-treatment bone microarchitectural characteristics, histopathological changes, and serum levels of anti-collagen antibodies, tumor necrosis factor-alpha, and interleukin (IL)-17 were investigated. We also examined cytokine production by type II collagen (CII)-stimulated splenocytes and mRNA expression of matrix metalloproteinases (MMPs), tissue inhibitors of metalloproteinase (TIMP)-1, receptor activator of nuclear factor-kappaB ligand (RANKL), and osteoprotegerin (OPG) in the joint tissues.
RESULTS
CK reduced the severity of CIA preventively and therapeutically (all p<0.05). Additionally, CK dose-dependently decreased histopathological signs of arthritis and improved microarchitectural characteristics (all p<0.05) at 10 to 20 mg/kg/d in CIA mice. CK treatment significantly decreased the serum levels of anti-CII immunoglobulin G (p<0.01) and the secretion of interferon-gamma and IL-2 from stimulated splenocytes (all p<0.05). Furthermore, MMP-3/TIMP-1 and RANKL/OPG ratios were suppressed in CK treated mice (all p<0.01).
CONCLUSION
CK attenuated CIA via suppression of the humoral immune response and modulation of joint-destructive mediators. These results suggest that CK has therapeutic potential in rheumatoid arthritis.
MeSH Terms
-
Animals
Antibodies, Neoplasm
Arthritis
Arthritis, Experimental*
Arthritis, Rheumatoid
Collagen Type II
Ginsenosides*
Immunity, Humoral
Immunoglobulin G
Interferon-gamma
Interleukin-2
Interleukins
Joints
Matrix Metalloproteinases
Mice*
Necrosis
Osteoprotegerin
Panax
RANK Ligand
RNA, Messenger
Antibodies, Neoplasm
Collagen Type II
Ginsenosides
Immunoglobulin G
Interferon-gamma
Interleukin-2
Interleukins
Matrix Metalloproteinases
Osteoprotegerin
RANK Ligand
RNA, Messenger
Figure
Cited by 1 articles
-
Compound K Inhibits Interleukin-1β-induced Expression of Inflammatory Mediators and Matrix Metalloproteinases by Inhibiting Mitogen-activated Protein Kinase Activation in Chondrocytes
Eun Hye Park, Ji Soo Kim, Jeong Seok Lee, Yun Jong Lee, Yeong Wook Song, Eun Young Lee
J Rheum Dis. 2018;25(3):188-196. doi: 10.4078/jrd.2018.25.3.188.
Reference
-
1. Furneri G, Mantovani LG, Belisari A, Mosca M, Cristiani M, Bellelli S, et al. Systematic literature review on economic implications and pharmacoeconomic issues of rheumatoid arthritis. Clin Exp Rheumatol. 2012; 30(4 Suppl 73):S72–84.2. Smolen JS, Aletaha D, Bijlsma JW, Breedveld FC, Boumpas D, Burmester G, et al. T2T Expert Committee. Treating rheumatoid arthritis to target: recommendations of an international task force. Ann Rheum Dis. 2010; 69:631–7.
Article3. Jung YO, Kim HA. Recent paradigm shifts in the diagnosis and treatment of rheumatoid arthritis. Korean J Intern Med. 2012; 27:378–87.
Article4. Moreland L. Unmet needs in rheumatoid arthritis. Arthritis Res Ther. 2005; 7(Suppl 3):S2–8.5. Kim HA, Kim S, Chang SH, Hwang HJ, Choi YN. Anti-ar-thritic effect of ginsenoside Rb1 on collagen induced arthritis in mice. Int Immunopharmacol. 2007; 7:1286–91.
Article6. Chang SH, Choi Y, Park JA, Jung DS, Shin J, Yang JH, et al. Anti-inflammatory effects of BT-201, an n-butanol extract of Panax notoginseng, observed in vitro and in a collagen-induced arthritis model. Clin Nutr. 2007; 26:785–91.
Article7. Shin JS, Park N, Ra J, Kim Y, Shin M, Hong M, et al. Panax ginseng C.A. Meyer modulates the levels of MMP3 in S12 murine articular cartilage cell line. J Ethnopharmacol. 2009; 124:397–403.
Article8. Kim KR, Chung TY, Shin H, Son SH, Park KK, Choi JH, et al. Red ginseng saponin extract attenuates murine collagen-induced arthritis by reducing proinflammatory responses and matrix metalloproteinase-3 expression. Biol Pharm Bull. 2010; 33:604–10.
Article9. Du J, Cheng B, Zhu X, Ling C. Ginsenoside Rg1, a novel glucocorticoid receptor agonist of plant origin, maintains glucocorticoid efficacy with reduced side effects. J Immunol. 2011; 187:942–50.
Article10. Na JY, Kim S, Song K, Lim KH, Shin GW, Kim JH, et al. Anti-apoptotic activity of ginsenoside Rb1 in hydrogen peroxide-treated chondrocytes: stabilization of mitochondria and the inhibition of caspase-3. J Ginseng Res. 2012; 36:242–7.11. Kim S, Na JY, Song KB, Choi DS, Kim JH, Kwon YB, et al. Protective effect of ginsenoside Rb1 on hydrogen pero-xide-induced oxidative stress in rat articular chondrocytes. J Ginseng Res. 2012; 36:161–8.12. Cheng W, Wu D, Zuo Q, Wang Z, Fan W. Ginsenoside Rb1 prevents interleukin-1 beta induced inflammation and apoptosis in human articular chondrocytes. Int Orthop. 2013; 37:2065–70.
Article13. So MW, Lee EJ, Lee HS, Koo BS, Kim YG, Lee CK, et al. Protective effects of ginsenoside Rg3 on human osteoarthritic chondrocytes. Mod Rheumatol. 2013; 23:104–11.
Article14. Lee JH, Lim H, Shehzad O, Kim YS, Kim HP. Ginsenosides from Korean red ginseng inhibit matrix metalloproteinase-13 expression in articular chondrocytes and prevent cartilage degradation. Eur J Pharmacol. 2014; 724:145–51.
Article15. Yu K, Chen F, Li C. Absorption, disposition, and pharmacokinetics of saponins from Chinese medicinal herbs: what do we know and what do we need to know more? Curr Drug Metab. 2012; 13:577–98.
Article16. Choi YS, Kang EH, Lee EY, Gong HS, Kang HS, Shin K, et al. Joint-protective effects of compound K, a major ginsenoside metabolite, in rheumatoid arthritis: in vitro evidence. Rheumatol Int. 2013; 33:1981–90.
Article17. Wu H, Chen J, Wang Q, Jia X, Song S, Yuan P, et al. Ginsenoside metabolite compound K attenuates inflammatory responses of adjuvant-induced arthritis rats. Immunopharmacol Immunotoxicol. 2014; 36:124–9.
Article18. Liu KK, Wang QT, Yang SM, Chen JY, Wu HX, Wei W. Ginsenoside compound K suppresses the abnormal activation of T lymphocytes in mice with collagen-induced arthritis. Acta Pharmacol Sin. 2014; 35:599–612.
Article19. Chen J, Wu H, Wang Q, Chang Y, Liu K, Song S, et al. Ginsenoside metabolite compound K alleviates adjuvantinduced arthritis by suppressing T cell activation. Inflammation. 2014; 37:1608–15.
Article20. Kim HO, Lee SI. Experimental animal models for rheumatoid arthritis: methods and applications. J Rheum Dis. 2012; 19:189–95.
Article21. Zhou W, Feng MQ, Li JY, Zhou P. Studies on the preparation, crystal structure and bioactivity of ginsenoside compound K. J Asian Nat Prod Res. 2006; 8:519–27.
Article22. Brand DD, Latham KA, Rosloniec EF. Collagen-induced arthritis. Nat Protoc. 2007; 2:1269–75.
Article23. Wooley PH. Collagen-induced arthritis in the mouse. Methods Enzymol. 1988; 162:361–73.24. Xiao J, Shimada M, Liu W, Hu D, Matsumori A. Anti-inflammatory effects of eplerenone on viral myocarditis. Eur J Heart Fail. 2009; 11:349–53.
Article25. Wells JE, Rice TK, Nuttall RK, Edwards DR, Zekki H, Rivest S, et al. An adverse role for matrix metalloproteinase 12 after spinal cord injury in mice. J Neurosci. 2003; 23:10107–15.
Article26. Palmqvist P, Lundberg P, Persson E, Johansson A, Lundgren I, Lie A, et al. Inhibition of hormone and cytokine-stimulated osteoclastogenesis and bone resorption by interleukin-4 and interleukin-13 is associated with increased osteoprotegerin and decreased RANKL and RANK in a STAT6-dependent pathway. J Biol Chem. 2006; 281:2414–29.
Article27. Lee JH, Chun KJ, Kim HS, Kim SH, Lee KY, Kim DJ, et al. Changes in microarchitectural characteristics at the tibial epiphysis induced by collagen-induced rheumatoid arthritis over time. Clin Interv Aging. 2012; 7:373–82.28. Nandakumar KS, Bäcklund J, Vestberg M, Holmdahl R. Collagen type II (CII)-specific antibodies induce arthritis in the absence of T or B cells but the arthritis progression is enhanced by CII-reactive T cells. Arthritis Res Ther. 2004; 6:R544–50.29. Matsuda H, Samukawa K, Kubo M. Anti-inflammatory activity of ginsenoside Ro. Planta Med. 1990; 56:19–23.30. Leung KW, Wong AS. Pharmacology of ginsenosides: a literature review. Chin Med. 2010; 5:20.
Article31. Kim KA, Jung IH, Park SH, Ahn YT, Huh CS, Kim DH. Comparative analysis of the gut microbiota in people with different levels of ginsenoside Rb1 degradation to compound K. PLoS One. 2013; 8:e62409.
Article32. Kim HK. Pharmacokinetics of ginsenoside Rb1 and its metabolite compound K after oral administration of Korean Red Ginseng extract. J Ginseng Res. 2013; 37:451–6.
Article33. Gao YL, Liu ZF, Li CM, Shen JY, Yin HX, Li GS. Subchronic toxicity studies with ginsenoside compound K delivered to dogs via intravenous administration. Food Chem Toxicol. 2011; 49:1857–62.
Article34. Rowley MJ, Nandakumar KS, Holmdahl R. The role of collagen antibodies in mediating arthritis. Mod Rheumatol. 2008; 18:429–41.
Article35. Germann T, Bongartz M, Dlugonska H, Hess H, Schmitt E, Kolbe L, et al. Interleukin-12 profoundly upregulates the synthesis of antigen-specific complement-fixing IgG2a, IgG2b and IgG3 antibody subclasses in vivo. Eur J Immunol. 1995; 25:823–9.36. Terato K, Hasty KA, Reife RA, Cremer MA, Kang AH, Stuart JM. Induction of arthritis with monoclonal antibodies to collagen. J Immunol. 1992; 148:2103–8.37. Billiau A, Matthys P. Collagen-induced arthritis and related animal models: how much of their pathogenesis is autoimmune, how much is autoinflammatory? Cytokine Growth Factor Rev. 2011; 22:339–44.
Article38. Nakae S, Nambu A, Sudo K, Iwakura Y. Suppression of immune induction of collagen-induced arthritis in IL-17-deficient mice. J Immunol. 2003; 171:6173–7.
Article39. Mori L, Iselin S, De Libero G, Lesslauer W. Attenuation of collagen-induced arthritis in 55-kDa TNF receptor type 1 (TNFR1)-IgG1-treated and TNFR1-deficient mice. J Immunol. 1996; 157:3178–82.40. Lee ES, Choi JS, Kim MS, You HJ, Ji GE, Kang YH. Ginsenoside metabolite compound K differentially antag-onizing tumor necrosis factor-α-induced monocyte-endothelial trafficking. Chem Biol Interact. 2011; 194:13–22.
Article41. Choi K, Kim M, Ryu J, Choi C. Ginsenosides compound K and Rh(2) inhibit tumor necrosis factor-alpha-induced activation of the NF-kappaB and JNK pathways in human as-troglial cells. Neurosci Lett. 2007; 421:37–41.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of ginsenosides on the desflurane modulation in the recombinant serotonin type 3A receptor expressed in Xenopus laevis oocytes
- Fluorescence bioimaging analysis of collagen antibody-induced arthritis in male mice
- Effect of Interleukin-10 on Development of Murine Collagen-induced Arthritis
- Effect of ginsenosides in a mouse model of bone cancer pain
- Lessons for the pathogenesis of rheumatoid arthritis acquired from experimental animal models