J Korean Neurosurg Soc.
2016 Mar;59(2):161-164. 10.3340/jkns.2016.59.2.161.
Preoperative Extrapontine Myelinolysis with Good Outcome in a Patient with Pituitary Adenoma
- Affiliations
-
- 1Department of Neurosurgery, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences, Beijing, P.R. China. xingbingemail@aliyun.com
- 2Department of Neurology, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences, Beijing, P.R. China.
- 3Department of Pathology, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences, Beijing, P.R. China.
- KMID: 2192048
- DOI: http://doi.org/10.3340/jkns.2016.59.2.161
Abstract
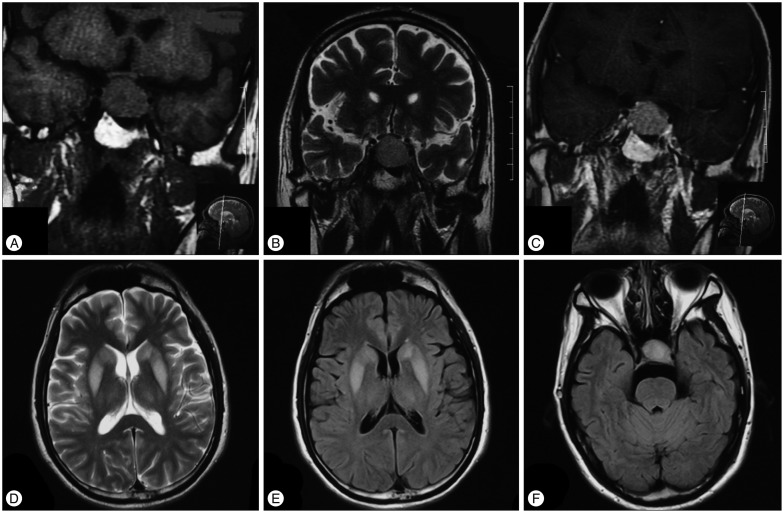
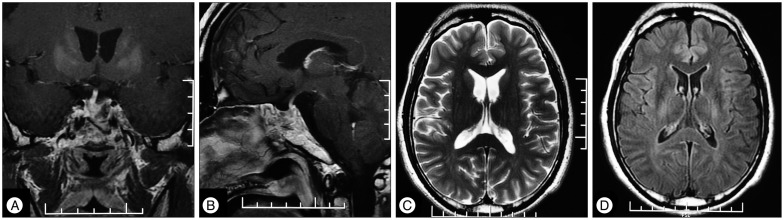
- Few preoperative extrapontine myelinolysis (EPM) cases with pituitary adenoma have been reported. No such case had long follow-up to see the outcome of EPM. We reported a 38-year-old man complaining of nausea, malaise and transient loss of consciousness who was found to have severe hyponatremia. Neurologic deficits including altered mental status, behavioral disturbances, dysarthria and dysphagia developed despite slow correction of hyponatremia. Endocrine and imaging studies revealed hypopituitarism, nonfunctional pituitary macroadenoma and extrapontine myelinolysis. Transsphenoidal surgery was performed after three weeks of supportive therapy, when neurological symptoms improved significantly. The patient recovered function completely 3 months after surgery. Our case indicates that outcome of EPM can be good even with prolonged periods of severe neurologic impairment.
MeSH Terms
Figure
Reference
-
1. Diederich S, Franzen NF, Bähr V, Oelkers W. Severe hyponatremia due to hypopituitarism with adrenal insufficiency : report on 28 cases. Eur J Endocrinol. 2003; 148:609–617. PMID: 12773132.2. Gankam Kengne F, Soupart A, Pochet R, Brion JP, Decaux G. Re-induction of hyponatremia after rapid overcorrection of hyponatremia reduces mortality in rats. Kidney Int. 2009; 76:614–621. PMID: 19606078.
Article3. Gocht A, Colmant HJ. Central pontine and extrapontine myelinolysis : a report of 58 cases. Clin Neuropathol. 1987; 6:262–270. PMID: 3322623.4. Kallakatta RN, Radhakrishnan A, Fayaz RK, Unnikrishnan JP, Kesavadas C, Sarma SP. Clinical and functional outcome and factors predicting prognosis in osmotic demyelination syndrome (central pontine and/or extrapontine myelinolysis) in 25 patients. J Neurol Neurosurg Psychiatry. 2011; 82:326–331. PMID: 20826870.
Article5. King JD, Rosner MH. Osmotic demyelination syndrome. Am J Med Sci. 2010; 339:561–567. PMID: 20453633.
Article6. Laureno R, Karp BI. Myelinolysis after correction of hyponatremia. Ann Intern Med. 1997; 126:57–62. PMID: 8992924.
Article7. Liamis G, Milionis HJ, Elisaf M. Endocrine disorders : causes of hyponatremia not to neglect. Ann Med. 2011; 43:179–187. PMID: 20964584.8. Lin SH, Hung YH, Lin YF. Severe hyponatremia as the presenting feature of clinically non-functional pituitary adenoma with hypopituitarism. Clin Nephrol. 2002; 57:85–88. PMID: 11837807.
Article9. Menger H, Jörg J. Outcome of central pontine and extrapontine myelinolysis (n=44). J Neurol. 1999; 246:700–705. PMID: 10460448.10. Murad MH, Fernández-Balsells MM, Barwise A, Gallegos-Orozco JF, Paul A, Lane MA, et al. Outcomes of surgical treatment for nonfunctioning pituitary adenomas : a systematic review and meta-analysis. Clin Endocrinol (Oxf). 2010; 73:777–791. PMID: 20846296.
Article11. Nakano H, Ohara Y, Bandoh K, Miyaoka M. A case of central pontine myelinolysis after surgical removal of a pituitary tumor. Surg Neurol. 1996; 46:32–36. PMID: 8677485.
Article12. Oelkers W. Hyponatremia and inappropriate secretion of vasopressin (antidiuretic hormone) in patients with hypopituitarism. N Engl J Med. 1989; 321:492–496. PMID: 2548097.
Article13. Oya S, Tsutsumi K, Ueki K, Kirino T. Reinduction of hyponatremia to treat central pontine myelinolysis. Neurology. 2001; 57:1931–1932. PMID: 11723299.
Article14. Srimanee D, Bhidayasiri R, Phanthumchinda K. Extrapontine myelinolysis in preoperative sellar region tumor : report of two cases. J Med Assoc Thai. 2009; 92:1548–1553. PMID: 19938750.15. Sterns RH, Riggs JE, Schochet SS Jr. Osmotic demyelination syndrome following correction of hyponatremia. N Engl J Med. 1986; 314:1535–1542. PMID: 3713747.
Article16. Tosaka M, Kohga H. Extrapontine myelinolysis and behavioral change after transsphenoidal pituitary surgery : case report. Neurosurgery. 1998; 43:933–936. PMID: 9766322.
Article17. Verbalis JG, Goldsmith SR, Greenberg A, Korzelius C, Schrier RW, Sterns RH, et al. Diagnosis, evaluation, and treatment of hyponatremia : expert panel recommendations. Am J Med. 2013; 126(10 Suppl 1):S1–S42. PMID: 24074529.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Central Pontine and Extrapontine Myelinolysis ; Frequent association with pituitary-adrenal axis dysfunction
- A Case of Subacute Onset Choreoathetosis as Sequelae of Central Pontine and Extrapontine Myelinolysis
- Neuropsychological Findings of Extrapontine Myelinolysis without Central Pontine Myelinolysis: Initial and Follow-up Evaluation
- Central Pontine and EXtrapontine Myelinolysis
- Central Pontine and Extrapontine Myelinolysis in a Patient with Traumatic Brain Injury Following Not Rapid Correction of Hyponatremia: A Case Report