J Korean Diabetes.
2014 Jun;15(2):124-128. 10.4093/jkd.2014.15.2.124.
Radiation Induced Peripheral Arterial Disease associated with Diabetes which Initially Considered as Diabetic Foot Disease
- Affiliations
-
- 1Department of Internal Medicine, Endocrinology and Metabolism, Kosin University College of Medicine, Busan, Korea. mir316@naver.com
- KMID: 2173905
- DOI: http://doi.org/10.4093/jkd.2014.15.2.124
Abstract
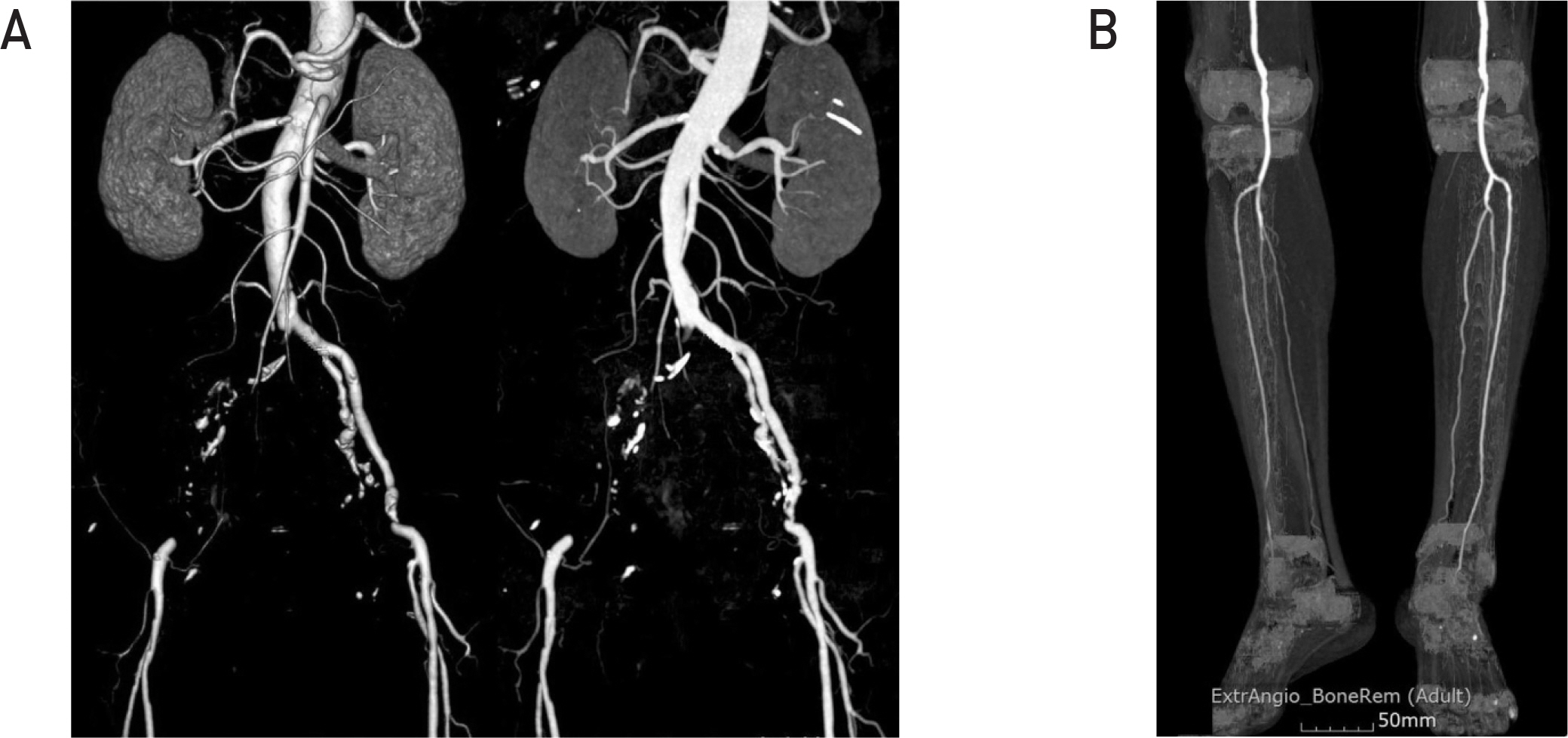
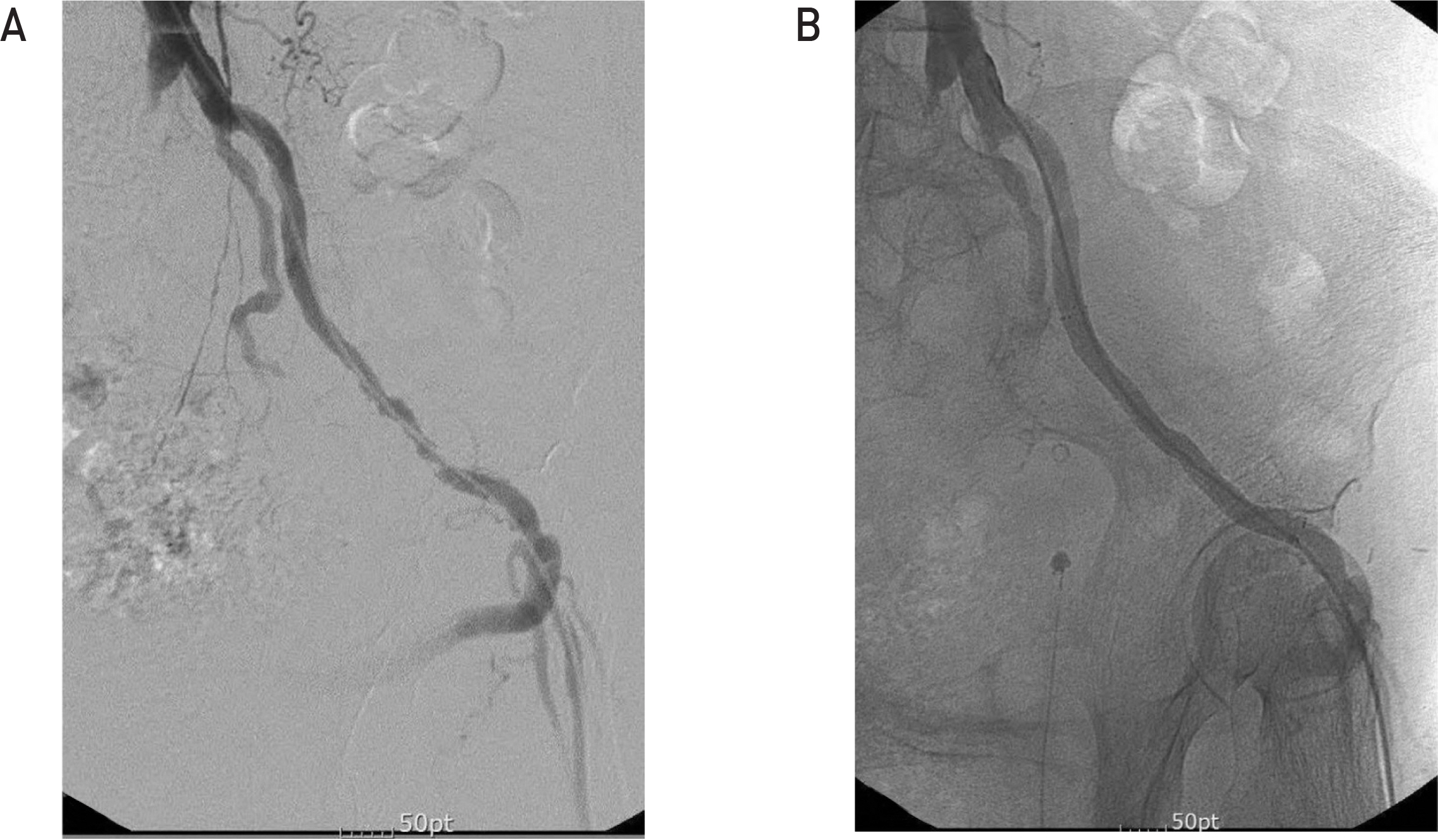
- Therapeutic high-dose radiation can induce atherosclerotic changes of affected arteries. Radiation-associated atherosclerotic diseases of coronary, carotid and subclavian arteries have been demonstrated for years in cancer survivors, but peripheral arterial disease (PAD) associated with radiation is rarely reported. PAD is one of the major macrovascular complications of diabetes and is associated with morbidity and increased mortality. We experienced a case of PAD associated with radiation therapy in a 65-year-old diabetic female patient who had undergone cervical cancer treatment 19 years prior. Computed tomographic angiogram showed occlusion and stenosis from common iliac arteries to superficial femoral arteries. However, both infrapopliteal arteries that are commonly involved in diabetes associated PAD were preserved. She was successfully treated with percutaneous angioplasty combined with femoro-femoral bypass operation. Based on the extent and severity of arterial stenosis in this non-smoking diabetic woman who had a history of high-dose radiation to her pelvis, we concluded that atherosclerotic lesions in this patient were caused by high-dose pelvic irradiation and then exacerbated by diabetes. Therefore, special attention should be given to diabetic patients with history of pelvic irradiation with regard to development of atherosclerosis of peripheral arteries, especially in the pelvic area.
MeSH Terms
Figure
Reference
-
References
1. Hughes WF, Carson CL, Laffaye HA. Subclavian artery occlusion 42 years after mastectomy and radiotherapy. Am J Surg. 1984; 147:698–700.
Article2. Har-Shai Y, Schein M, Molek AD, Peled IJ, Best LA. Ruptured mycotic aneurysm of the subclavian artery after irradiation. A case report. Eur J Surg. 1993; 159:59–60.3. American Diabetes Association. Peripheral arterial disease in people with diabetes. Diabetes Care. 2003; 26:3333–41.4. Kannel WB, McGee DL. Update on some epidemiologic features of intermittent claudication: the Framingham Study. J Am Geriatr Soc. 1985; 33:13–8.
Article5. Beks PJ, Mackaay AJ, de Neeling JN, de Vries H, Bouter LM, Heine RJ. Peripheral arterial disease in relation to glycaemic level in an elderly Caucasian population: the Hoorn study. Diabetologia. 1995; 38:86–96.
Article6. Jude EB, Oyibo SO, Chalmers N, Boulton AJ. Peripheral arterial disease in diabetic and nondiabetic patients: a comparison of severity and outcome. Diabetes Care. 2001; 24:1433–7.7. Doi H, Kamikonya N, Takada Y, Fujiwara M, Tsuboi K, Miura H, Inoue H, Tanooka M, Nakamura T, Shikata T, Kimura T, Tsujimura T, Hirota S. Long-term sequential changes of radiation proctitis and angiopathy in rats. J Radiat Res. 2012; 53:217–24.
Article8. Butler MJ, Lane RH, Webster JH. Irradiation injury to large arteries. Br J Surg. 1980; 67:341–3.
Article9. Modrall JG, Sadjadi J. Early and late presentations of radiation arteritis. Semin Vasc Surg. 2003; 16:209–14.
Article10. Tetik O, Yetkin U, Calli AO, Ilhan G, Gurbuz A. Occlusive arterial disease after radiotherapy for testicular cancer: case report and review of the literature. Vascular. 2008; 16:239–41.
Article11. Ross HB, Sales JE. Post-irradiation femoral aneurysm treated by iliopopliteal bypass via the obturator foramen. Br J Surg. 1972; 59:400–5.
Article12. Jurado JA, Bashir R, Burket MW. Radiation-induced peripheral artery disease. Catheter Cardiovasc Interv. 2008; 72:563–8.
Article13. Moutardier V, Christophe M, Lelong B, Houvenaeghel G, Delpero JR. Iliac atherosclerotic occlusive disease complicating radiation therapy for cervix cancer: a case series. Gynecol Oncol. 2002; 84:456–9.
Article