Ewha Med J.
2014 Mar;37(1):46-51. 10.12771/emj.2014.37.1.46.
A Favorable Treatment Response of Erlotinib in Lung Adenocarcinoma with Concomitant Activating EGFR Mutation and ROS1 Rearrangement
- Affiliations
-
- 1Division of Medical Oncology, Yonsei Cancer Center, Seoul, Korea. cbc1971@yuhs.ac
- 2Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2171274
- DOI: http://doi.org/10.12771/emj.2014.37.1.46
Abstract
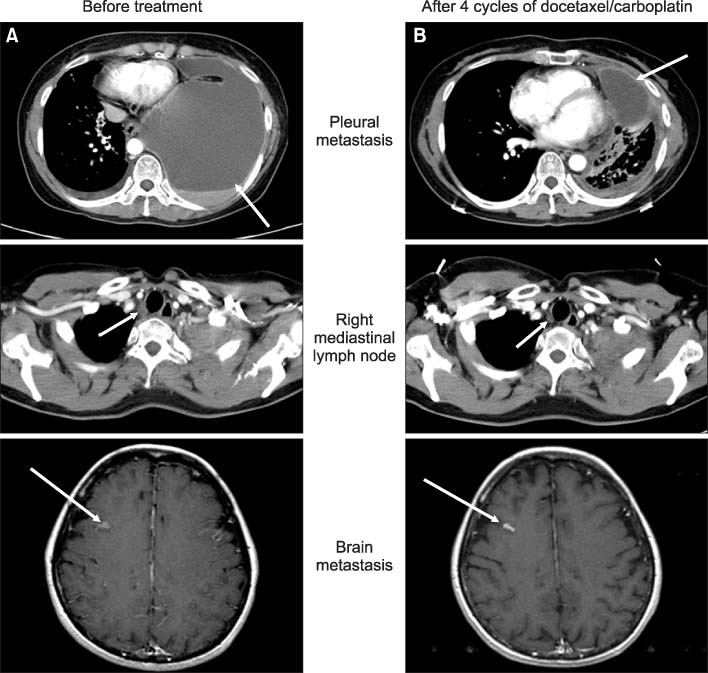
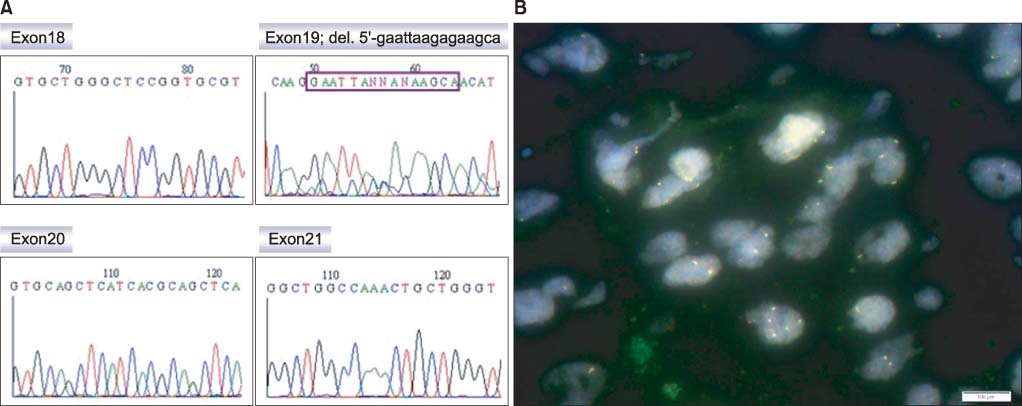
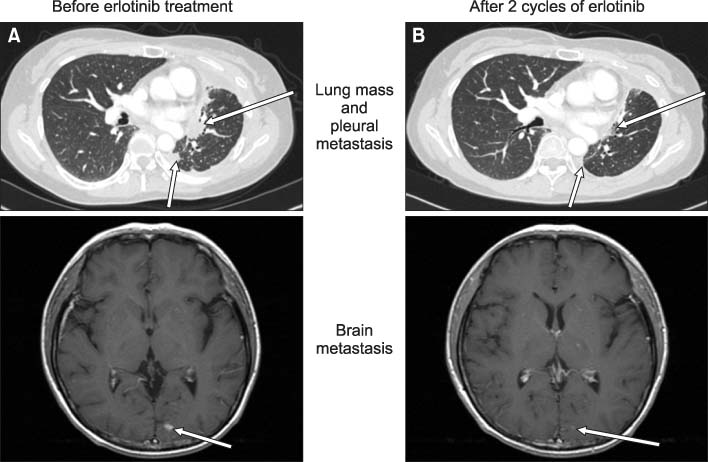
- The rearrangement of c-ros oncogene 1 (ROS1) has been recently identified as an important molecular target in non small cell lung cancer (NSCLC). ROS1 rearrangement and epidermal growth factor receptor (EGFR) mutation were mutually exclusive each other in previous studies, and the clinical implication of co-existence of the two genetic alterations has not been determined. We report a case of 46-year-old female never-smoker NSCLC patient whose tumor harbored ROS1 rearrangement and EGFR mutation concomitantly. She had undergone curative surgery for stage IIIA NSCLC, and the recurrence in left pleura and brain occurred at 2 years after the surgery. She received several lines of chemotherapy including docetaxel plus carboplatin, erlotinib, pemetrexed, and gemcitabine. Erlotinib therapy showed a favorable treatment response with progression-free survival of 9.5 months and partial response of tumor on radiologic evaluations. This case represents a successful erlotinib treatment in a NSCLC patient with concurrent ROS1 rearrangement and EGFR mutation.
Keyword
MeSH Terms
Figure
Reference
-
1. Jung KW, Won YJ, Kong HJ, Oh CM, Seo HG, Lee JS. Cancer statistics in Korea: incidence, mortality, survival and prevalence in 2010. Cancer Res Treat. 2013; 45:1–14.2. Oxnard GR, Binder A, Janne PA. New targetable oncogenes in non-small-cell lung cancer. J Clin Oncol. 2013; 31:1097–1104.3. Soda M, Choi YL, Enomoto M, Takada S, Yamashita Y, Ishikawa S, et al. Identification of the transforming EML4-ALK fusion gene in non-small-cell lung cancer. Nature. 2007; 448:561–566.4. Shaw AT, Yeap BY, Mino-Kenudson M, Digumarthy SR, Costa DB, Heist RS, et al. Clinical features and outcome of patients with non-small-cell lung cancer who harbor EML4-ALK. J Clin Oncol. 2009; 27:4247–4253.5. Davies KD, Le AT, Theodoro MF, Skokan MC, Aisner DL, Berge EM, et al. Identifying and targeting ROS1 gene fusions in nonsmall cell lung cancer. Clin Cancer Res. 2012; 18:4570–4579.6. Rikova K, Guo A, Zeng Q, Possemato A, Yu J, Haack H, et al. Global survey of phosphotyrosine signaling identifies oncogenic kinases in lung cancer. Cell. 2007; 131:1190–1203.7. Bergethon K, Shaw AT, Ou SH, Katayama R, Lovly CM, McDonald NT, et al. ROS1 rearrangements define a unique molecular class of lung cancers. J Clin Oncol. 2012; 30:863–870.8. Ju YS, Lee WC, Shin JY, Lee S, Bleazard T, Won JK, et al. A transforming KIF5B and RET gene fusion in lung adenocarcinoma revealed from whole-genome and transcriptome sequencing. Genome Res. 2012; 22:436–445.9. Shaw AT, Camidge DR, Engelman JA, Solomon BJ, Kwak EL, Clark JW, et al. Clinical activity of crizotinib in advanced nonsmall cell lung cancer (NSCLC) harboring ROS1 gene rearrangement. J Clin Oncol. 2012; 30 suppl. abstr 7508.10. Gainor JF, Varghese AM, Ou SH, Kabraji S, Awad MM, Katayama R, et al. ALK rearrangements are mutually exclusive with mutations in EGFR or KRAS: an analysis of 1,683 patients with nonsmall cell lung cancer. Clin Cancer Res. 2013; 19:4273–4281.11. Birchmeier C, Sharma S, Wigler M. Expression and rearrangement of the ROS1 gene in human glioblastoma cells. Proc Natl Acad Sci U S A. 1987; 84:9270–9274.12. Tiseo M, Gelsomino F, Boggiani D, Bortesi B, Bartolotti M, Bozzetti C, et al. EGFR and EML4-ALK gene mutations in NSCLC: a case report of erlotinib-resistant patient with both concomitant mutations. Lung Cancer. 2011; 71:241–243.13. Tanaka H, Hayashi A, Morimoto T, Taima K, Tanaka Y, Shimada M, et al. A case of lung adenocarcinoma harboring EGFR mutation and EML4-ALK fusion gene. BMC Cancer. 2012; 12:558.14. Kuo YW, Wu SG, Ho CC, Shih JY. Good response to gefitinib in lung adenocarcinoma harboring coexisting EML4-ALK fusion gene and EGFR mutation. J Thorac Oncol. 2010; 5:2039–2040.15. Charest A, Wilker EW, McLaughlin ME, Lane K, Gowda R, Coven S, et al. ROS fusion tyrosine kinase activates a SH2 domain-containing phosphatase-2/phosphatidylinositol 3-kinase/mammalian target of rapamycin signaling axis to form glioblastoma in mice. Cancer Res. 2006; 66:7473–7481.16. Takeuchi K, Soda M, Togashi Y, Suzuki R, Sakata S, Hatano S, et al. RET, ROS1 and ALK fusions in lung cancer. Nat Med. 2012; 18:378–381.17. Kim HR, Lim SM, Kim HJ, Hwang SK, Park JK, Shin E, et al. The frequency and impact of ROS1 rearrangement on clinical outcomes in never smokers with lung adenocarcinoma. Ann Oncol. 2013; 24:2364–2370.18. Camidge DR, Kono SA, Lu X, Okuyama S, Baron AE, Oton AB, et al. Anaplastic lymphoma kinase gene rearrangements in non-small cell lung cancer are associated with prolonged progression-free survival on pemetrexed. J Thorac Oncol. 2011; 6:774–780.19. Takeda M, Okamoto I, Sakai K, Tanaka K, Terashima M, Nishio K, et al. Successful long-term treatment with pemetrexed of NSCLC associated with EML4-ALK and low thymidylate synthase expression. Clin Lung Cancer. 2012; 13:157–159.20. Kim HR, Shim HS, Chung JH, Lee YJ, Hong YK, Rha SY, et al. Distinct clinical features and outcomes in never-smokers with nonsmall cell lung cancer who harbor EGFR or KRAS mutations or ALK rearrangement. Cancer. 2012; 118:729–739.21. Cufer T, Ovcaricek T, O'Brien ME. Systemic therapy of advanced non-small cell lung cancer: major-developments of the last 5-years. Eur J Cancer. 2013; 49:1216–1225.22. Shaw AT, Yeap BY, Solomon BJ, Riely GJ, Gainor J, Engelman JA, et al. Effect of crizotinib on overall survival in patients with advanced non-small-cell lung cancer harbouring ALK gene rearrangement: a retrospective analysis. Lancet Oncol. 2011; 12:1004–1012.23. Shaw AT, Kim DW, Nakagawa K, Seto T, Crino L, Ahn MJ, et al. Crizotinib versus chemotherapy in advanced ALK-positive lung cancer. N Engl J Med. 2013; 368:2385–2394.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Successful Rechallenge with Gefitinib for an Initial Erlotinib-Responder with Advanced Lung Adenocarcinoma
- Sequential Responses of Adenocarcinoma of the Lung to Erlotinib after Gefitinib in Never Smoker Korean Woman
- Overview of ALK and ROS1 Rearranged Lung Cancer
- A Case of Patient with Lung Adenocarcinoma with Double Rare EGFR Mutation of G719C and L861Q
- Molecular Diagnosis in Lung Cancer