Infect Chemother.
2011 Feb;43(1):64-67. 10.3947/ic.2011.43.1.64.
Emphysematous prostatitis combined with a liver abscess caused by Klebsiella pneumoniae
- Affiliations
-
- 1Department of Internal Medicine, Sam Anyang General Hospital, Anyang, Korea. sstone99@hanmail.net
- KMID: 2170336
- DOI: http://doi.org/10.3947/ic.2011.43.1.64
Abstract
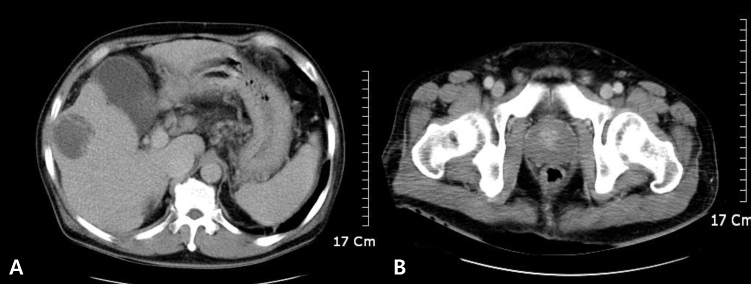
- Emphysematous prostatitis is a rare condition that is characterized by gas and abscess accumulation in the prostate. This uncommon but serious disease requires special attention because of its nonspecific presentation such as dysuria, frequency, urgency, fever, acute urinary retension and/or perineal pain. We report here on a case of emphysematous prostatitis that was combined with a liver abscess caused by Klebsiella pneumoniae. A 55-year-old man was admitted due to a 3-day history of urinary retention with a febrile sensation. He had histories of liver cirrhosis and uncontrolled diabetes mellitus. After blood and urine cultures, levofloxacin 500 mg was started intravenously. On the third hospital day, he displayed septic shock. The kidneys-ureters bladder (KUB) X-ray showed pockets of air-accumulation in the lower pelvic cavity, and abdominopelvic computed tomography (CT) with contrast enhancement taken on the third day showed a 5-cm liver abscess with an emphysematous prostate. Intravenous antibiotics was changed to metronidazole 500 mg q.i.d. and cefotaxime 2 g t.i.d. On the sixth day, transurethral resection and drainage were performed under spinal anesthesia. However, the postoperative bleeding continued and hypovolemic shock persisted, which then provoked multiorgan failure. The patient died on the 11th hospital day. K. pneumoniae was cultured from the liver abscess aspirate, blood and prostatic tissue, and the bacteria were sensitive to both levofloxacin and cefotaxime. Emphysematous prostatitis is a difficult to diagnose because of its rarity and nonspecific symptoms. A delayed diagnosis can cause high mortality and morbidity, so making a prompt clinical diagnosis of this condition is essential. Appropriate antibiotics with early adequate incision and drainage are also needed.
Keyword
MeSH Terms
-
Abscess
Anesthesia, Spinal
Anti-Bacterial Agents
Bacteria
Cefotaxime
Delayed Diagnosis
Diabetes Mellitus
Drainage
Dysuria
Fever
Hemorrhage
Humans
Klebsiella
Klebsiella pneumoniae
Liver
Liver Abscess
Liver Cirrhosis
Metronidazole
Middle Aged
Ofloxacin
Pneumonia
Prostate
Prostatitis
Sensation
Shock
Shock, Septic
Urinary Bladder
Urinary Retention
Anti-Bacterial Agents
Cefotaxime
Metronidazole
Ofloxacin
Figure
Reference
-
1. Kuo PH, Huang KH, Lee CW, Lee WJ, Chen SJ, Liu KL. Emphysematous prostatitis caused by K. pneumoniae. J Formos Med Assoc. 2007. 106:74–77.2. Bae GB, Kim SW, Shin BC, Oh JT, Do BH, Park JH, Lee JM, Kim NS. Emphysematous prostatic abscess due to K. pneumoniae: report of a case and review of the literature. J Korean Med Sci. 2003. 18:758–760.
Article3. Bartkowski DP, Lanesky JR. Emphysematous prostatitis and cystitis secondary to Candida albicans. J Urol. 1988. 139:1063–1065.4. Thorner DA, Sfakianos JP, Cabrera F, Lang EK, Colon I. Emphysematous prostatitis in a diabetic patient. J Urol. 2010. 183:2025.
Article5. Sampathkumar K, Murali TR, Sooraj YS, Mahaldar AR. Emphysematous prostatitis in renal transplant. Indian J Urol. 2007. 23:476–478.
Article6. Chung DR, Lee SS, Lee HR, Kim HB, Choi HJ, Eom JS, Kim JS, Choi YH, Lee JS, Chung MH, Kim YS, Lee H, Lee MS, Park CK. Korean Study Group for Liver Abscess. Emerging invasive liver abscess caused by K1 serotype K. pneumoniae in Korea. J Infect. 2007. 54:578–583.
Article7. Ko WC, Paterson DL, Sagnimeni AJ, Hansen DS, Von Gottberg A, Mohapatra S, Casellas JM, Goossens H, Mulazimoglu L, Trenholme G, Klugman KP, McCormack JG, Yu VL. Community-acquired K. pneumoniae bacteremia: global differences in clinical patterns. Emerg Infect Dis. 2002. 8:160–166.
Article8. Kang CI, Kim SH, Bang JW, Kim HB, Kim NJ, Kim EC, Oh MD, Choe KW. Community-acquired versus nosocomial K. pneumoniae bacteremia: clinical features, treatment outcomes, and clinical implication of antimicrobial resistance. J Korean Med Sci. 2006. 21:816–822.
Article9. Nadasy KA, Domiati-Saad R, Tribble MA. Invasive K. pneumoniae syndrome in North America. Clin Infect Dis. 2007. 45:e25–e28.10. Cheng DL, Liu YC, Yen MY, Liu CY, Wang RS. Septic metastatic lesions of pyogenic liver abscess. Their association with K. pneumoniae bacteremia in diabetic patients. Arch Intern Med. 1991. 151:1557–1559.
Article11. Tsay RW, Siu LK, Fung CP, Chang FY. Characteristics of bacteremia between community-acquired and nosocomial K. pneumoniae infection: risk factor for mortality and the impact of capsular serotypes as a herald for community-acquired infection. Arch Intern Med. 2002. 162:1021–1027.
Article12. Lee HC, Chuang YC, Yu WL, Lee NY, Chang CM, Ko NY, Wang LR, Ko WC. Clinical implications of hypermucoviscosity phenotype in K. pneumoniae isolates: association with invasive syndrome in patients with community-acquired bacteraemia. J Intern Med. 2006. 259:606–614.
Article13. Kawai T. Hypermucoviscosity: an extremely sticky phenotype of K. pneumoniae associated with emerging destructive tissue abscess syndrome. Clin Infect Dis. 2006. 42:1359–1361.
Article14. Ma LC, Fang CT, Lee CZ, Shun CT, Wang JT. Genomic heterogeneity in K. pneumoniae strains is associated with primary pyogenic liver abscess and metastatic infection. J Infect Dis. 2005. 192:117–128.
Article15. Yang CC, Yen CH, Ho MW, Wang JH. Comparison of pyogenic liver abscess caused by non-K. pneumoniae and K. pneumoniae. J Microbiol Immunol Infect. 2004. 37:176–184.16. Fung CP, Chang FY, Lee SC, Hu BS, Kuo BI, Liu CY, Ho M, Siu LK. A global emerging disease of K. pneumoniae liver abscess: is serotype K1 an important factor for complicated endophthalmitis? Gut. 2002. 50:420–424.
Article17. Fang CT, Chuang YP, Shun CT, Chang SC, Wang JT. A novel virulence gene in K. pneumoniae strains causing primary liver abscess and septic metastatic complications. J Exp Med. 2004. 199:697–705.
Article18. Lederman ER, Crum NF. Pyogenic liver abscess with a focus on K. pneumoniae as a primary pathogen: an emerging disease with unique clinical characteristics. Am J Gastroenterol. 2005. 100:322–331.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Emphysematous Prostatic Abscess Due to Klebsiella pneumoniae: Report of a Case And Review of the Literature
- Rapidly Fatal Emphysematous Osteomyelitis with Multiple Septic Emboli and Liver Abscess Caused by Klebsiella pneumoniae
- A Case of Endogenous endophthalmitis Caused by Klebsiella Pneumoniae from Emphysematous Pyelonephritis
- Spondylodiscitis with Epidural Abscess Caused by Klebsiella pneumoniae
- Occurrence of liver abscess in patients with acute prostatitis