Infect Chemother.
2010 Jun;42(3):198-202. 10.3947/ic.2010.42.3.198.
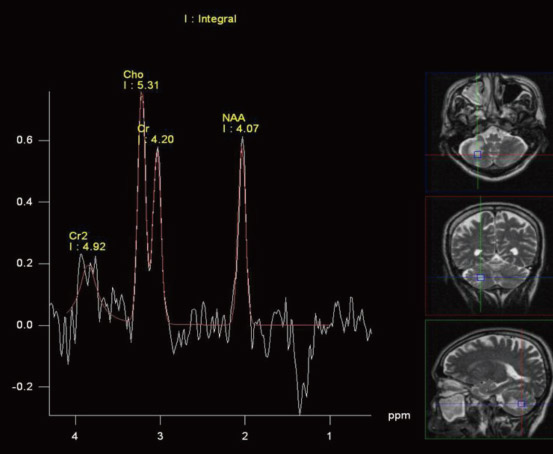
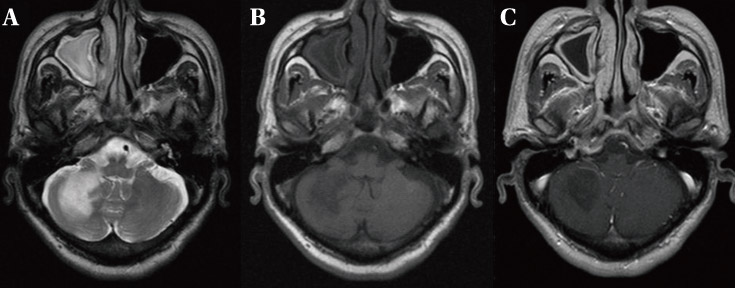
A Case of Immune Reconstitution Inflammatory Syndrome in AIDS-related Progressive Multifocal Leukoencephalopathy after Antiretroviral Therapy
- Affiliations
-
- 1Division of Infectious Diseases, Department of Internal Medicine, Eulji University College of Medicine, Daejeon, Korea. yhj822@medimail.co.kr
- 2Department of Radiology, Eulji University College of Medicine, Daejeon, Korea.
- KMID: 2170311
- DOI: http://doi.org/10.3947/ic.2010.42.3.198
Abstract
- Progressive multifocal leukoencephalopathy (PML) is a demyelinating disease of the central nervous system due to JC virus. In acquired immunodeficiency syndrome (AIDS) patients, JC virus infects myelin-producing oligodendrocytes causing a non-inflammatory lytic reaction leading to demyelination and brain death. We herein report a case of a 56-years-old AIDS man who developed immune reconstitution inflammatory syndrome and died while undergoing highly active antiretroviral therapy. In this patient, the PML involved the brainstem, causing mental confusion followed by recurrent aspiration, adult respiratory distress syndrome, and eventually to early death.
Keyword
MeSH Terms
Figure
Reference
-
1. D'Amico R, Sarkar S, Yusuff J, Azar E, Perlman DC. Immune reconstitution after potent antiretroviral therapy in AIDS patients with progressive multifocal leukoencephalopathy. Scand J Infect Dis. 2006. 39:347–350.2. Martinez JV, Mazziotti JV, Efron ED, Bonardo P, Jordan R, Sevlever G, Martinez M, Verbanaz SC, Salazar ZS, Pardal MF, Reisin R. Immune reconstitution inflammatory syndrome associated with PML in AIDS: a treatable disorder. Neurology. 2006. 67:1692–1694.
Article3. Kraemer C, Evers S, Nolting T, Arendt G, Husstedt IW. Cidofovir in combination with HAART and survival in AIDS-associated progressive multifocal leukoencephalopathy. J Neurol. 2008. 255:526–531.
Article4. Gray F, Chrétien F, Vallat-Decouvelaere AV, Scaravilli F. The changing pattern of HIV neuropathology in the HAART era. J Neuropathol Exp Neurol. 2003. 62:429–440.
Article5. Fedele CG, Ciardi M, Delia S, Echevarria JM, Tenorio A. Multiplex polymerase chain reaction for the simultaneous detection and typing of polyomavirus JC, BK and SV40 DNA in clinical samples. J Virol Methods. 1999. 82:137–144.
Article6. Berger JR. Progressive multifocal leukoencephalopathy. Curr Neurol Neurosci Rep. 2007. 7:461–469.
Article7. Chukwudelunzu FE. Progressive multifocal leukoencephalopathy as an initial manifestation of AIDS. Hosp Physician. 2001. 5:65–70.8. Lee MH, Chen YZ, Wang LS, Yen PS, Hsu YH. Progressive multifocal leukoencephalopathy in an AIDS patient. J Formos Med Assoc. 2007. 106:Suppl 3. S24–S28.
Article9. Aksamit AJ. Progressive multifocal leukoencephalopathy. Curr Treat Options Neurol. 2008. 10:178–185.
Article10. Major EO, Amemiya K, Tornatore CS, Houff SA, Berger JR. Pathogenesis and molecular biology of progressive multifocal leukoencephalopathy, the JC virus-induced demyelinating disease of the human brain. Clin Microbiol Rev. 1992. 5:49–73.
Article11. Koralnik IJ. New insights into progressive multifocal leukoencephalopathy. Curr Opin Neurol. 2004. 17:365–370.
Article12. Raina S, Kaushal SS, Gupta D, Himral P, Sawal N, Sood V, Goyal A. Progressive multifocal leukoencephalopathy--as a presenting manifestation of AIDS. J Assoc Physicians India. 2007. 55:797–801.13. Berger JR, Houff S. Progressive multifocal leukoencephalopathy: lessons from AIDS and natalizumab. Neurol Res. 2006. 28:299–305.
Article14. Berger JR, Levy RM, Flomenhoft D, Dobbs M. Predictive factors for prolonged survival in acquired immunodeficiency syndrome-associated progressive multifocal leukoencephalopathy. Ann Neurol. 1998. 44:341–349.
Article15. Koralnik IJ, Du Pasquier RA, Letvin NL. JC virus-specific cytotoxic T lymphocytes in individuals with progressive multifocal leukoencephalopathy. J Virol. 2001. 75:3483–3487.
Article16. Agostini HT, Ryschkewitsch CF, Stoner GL. Genotype profile of human polyomavirus JC excreted in urine of immunocompetent individuals. J Clin Microbiol. 1996. 34:159–164.
Article17. De Luca A, Ammassari A, Pezzotti P, Cinque P, Gasnault J, Berenguer J, Di Giambenedetto S, Cingolani A, Taoufik Y, Miralles P, Marra CM, Antinori A. Gesida 9/99, IRINA, ACTG 363 Study Groups. Cidofovir in addition to antiretroviral treatment is not effective for AIDS-associated progressive multifocal leukoencephalopathy: a multicohort analysis. AIDS. 2008. 22:1759–1767.
Article18. Tan K, Roda R, Ostrow L, McArthur J, Nath A. PML-IRIS in patients with HIV infection: clinical manifestations and treatment with steroids. Neurology. 2009. 72:1458–1464.
Article19. Berger JR. Steroids for PML-IRIS: a double-edged sword? Neurology. 2009. 72:1454–1455.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Molluscum Contagiosum as a Skin Manifestation of Immune Reconstitution Inflammatory Syndrome in an AIDS Patient Who Is Receiving HAART
- Herpes Zoster Immune Reconstitution Inflammatory Syndrome in a HIV-infected Patient: Case Report and Literature Review
- A Case of Cytomegalovirus Enterocolitis and Jejunal Perforation During Immune Reconstitution with Highly Active Antiretroviral Treatment
- Immune Reconstitution Inflammatory Syndrome Presenting as Cutaneous Miliary Tuberculosis in an HIV-Infected Patient
- A Case of Progressive Multifocal Leukoencephalopathy in a Patient with Acquired Immune Deficiency Syndrome