J Korean Med Sci.
2013 Jan;28(1):55-61. 10.3346/jkms.2013.28.1.55.
Changes in Anti-Group A Rotavirus Antibody Seroprevalence and Levels in the Western Gyeongnam Province of Korea Over 16 Years
- Affiliations
-
- 1Department of Pediatrics, Gyeongsang National University School of Medicine, Gyeongsang Institute of Health Science, Jinju, Korea. hsyoun@gnu.ac.kr
- 2Department of Otorhinolaryngology, Gyeongsang National University School of Medicine, Gyeongsang Institute of Health Science, Jinju, Korea.
- 3Department of Microbiology, Gyeongsang National University School of Medicine, Gyeongsang Institute of Health Science, Jinju, Korea.
- 4Department of Microbiology, Chung-Ang University College of Medicine, Seoul, Korea.
- KMID: 2158001
- DOI: http://doi.org/10.3346/jkms.2013.28.1.55
Abstract
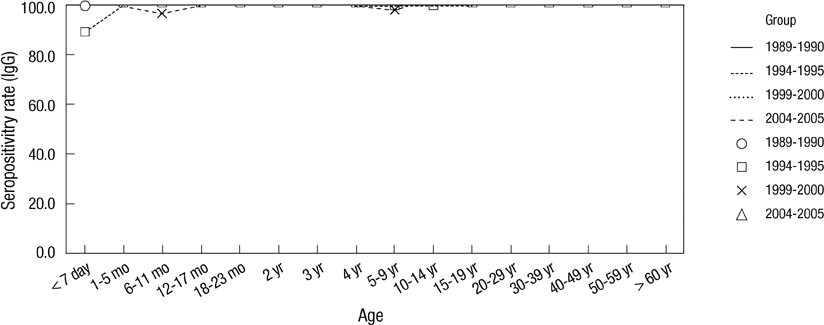
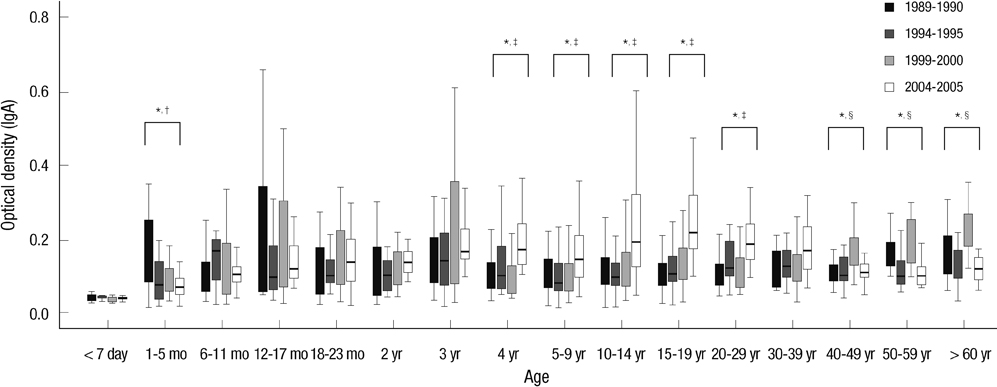
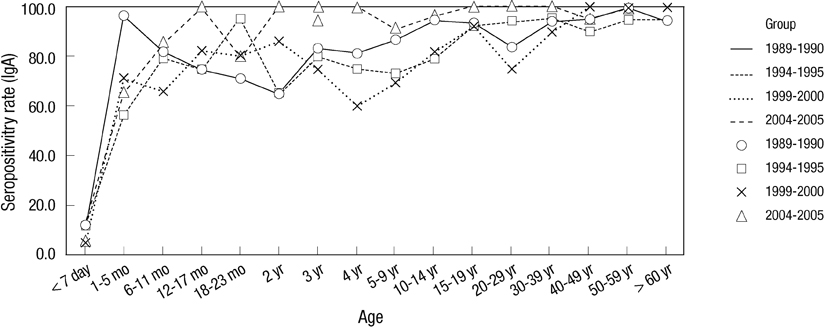
- To observe how anti-group A rotavirus antibody seropositivity rates and levels have changed in the western region of Gyeongnam Province, 2,030 serum samples collected at four collection periods (1989-1990, 1994-1995, 1999-2000, and 2004-2005) were tested by Enzyme-Linked Immunosorbent Assay for IgG, and IgA antibodies reacting to recombinant VP6 protein. The seroprevalences exhibit no regular patterns over a 16-yr period. For all four collection periods, the anti-rVP6 IgG levels rose steadily during the first 5 months of life, after which they remained high. However, the 2-9 yr and 10-39 yr groups had significantly higher IgG levels in 1999-2000 and 2004-2005, respectively, than in the other collection periods. The 1-5 mo, 40- > or = 60 yr, and 4-29 yr groups had significantly higher IgA levels in 1989-1990, 1999-2000, and 2004-2005, respectively. The 4 yr (25.0%), 5-9 yr (18.8%), 10-14 yr (41.1%), 20-29 yr (35.0%), and 30-39 yr (20.0%) groups in 2004-2005 had significant higher IgA seropositivity rate compared to the other three collection periods. These observations suggest that in the western region of Gyeongnam Province since the late 1990s, rotavirus reinfection has occurred more frequently than previously, with all ages being at risk.
Keyword
MeSH Terms
-
Adult
Aged
Antibodies, Viral/*blood
Antigens, Viral/genetics/immunology/metabolism
Capsid Proteins/genetics/immunology/metabolism
Child
Child, Preschool
Enzyme-Linked Immunosorbent Assay
Female
Humans
Immunoglobulin A/blood
Immunoglobulin G/blood
Infant
Infant, Newborn
Male
Middle Aged
Recombinant Proteins/biosynthesis/genetics/immunology
Republic of Korea/epidemiology
Rotavirus/isolation & purification/*metabolism
Rotavirus Infections/*epidemiology/virology
Seroepidemiologic Studies
Time Factors
Young Adult
Antibodies, Viral
Antigens, Viral
Capsid Proteins
Immunoglobulin A
Immunoglobulin G
Recombinant Proteins
VP6 protein, Rotavirus
Figure
Reference
-
1. Centers for Disease Control and Prevention. Atkinson WHJ, McIntyre L, Wolfe S, editors. Rotavirus. Epidemiology and Prevention of Vaccine-preventable Diseases. 2007. 10th ed. Washington, DC: Public Health Foundation;295–306.2. Seo JK, Sim JG. Overview of rotavirus infections in Korea. Pediatr Int. 2000. 42:406–410.3. Chae JH, Kim MJ, Kim DH, Lee KY, Kang JH, Lee JS. Epidemiologic study of rotavirus gastroenteritis, in Daejeon, Korea, 2001-2005. Korean J Pediatr Infect Dis. 2007. 14:155–161.4. Kim JS, Lee HS, Choi JH, Shin YJ, Koo ML, Kim SS, Kim HS, Kim EA, Yoon SW, Kwon JH, et al. A study of acute gastroenteritis in neonates transferred from postpartum care centers. Korean J Pediatr Infect Dis. 2003. 10:186–192.5. Park SI, Kwon HO, Lee JH, Jung SJ. Clinical features of rotaviral gastroenteritis in neonates. Korean J Pediatr. 2005. 48:1121–1125.6. Seo HJ, Jung YJ, Park SK, Choi SH, Lee JH, Kim MJ, Chang YS, Park WS. Rotavirus-associated neonatal necrotizing enterocolitis. Korean J Pediatr. 2009. 52:56–60.7. Veláquez FR, Matson DO, Guerrero ML, Shults J, Calva JJ, Morrow AL, Glass RI, Pickering LK, Ruiz-Palacios GM. Serum antibody as a marker of protection against natural rotavirus infection and disease. J Infect Dis. 2000. 182:1602–1609.8. Griffin DD, Fletcher M, Levy ME, Ching-Lee M, Nogami R, Edwards L, Peters H, Montague L, Gentsch JR, Glass RI. Outbreaks of adult gastroenteritis traced to a single genotype of rotavirus. J Infect Dis. 2002. 185:1502–1505.9. Ward RL, Bernstein DI, Shukla R, Young EC, Sherwood JR, McNeal MM, Walker MC, Schiff GM. Effects of antibody to rotavirus on protection of adults challenged with a human rotavirus. J Infect Dis. 1989. 159:79–88.10. Seo JH, Kim SY, Park JS, Lim JY, Park CH, Woo HO, Youn HS, Kim W, Kang HL, Baik SC, et al. Usefulness of Escherichia coli-expressed recombinant VP6 proteins of group A rotavirus in serodiagosis of rotavirus infection. Korean J Pediatr Gastroenterol Nutr. 2010. 13:134–145.11. Ray PG, Kelkar SD, Walimbe AM, Biniwale V, Mehendale S. Rotavirus immunoglobulin levels among Indian mothers of two socio-economic groups and occurrence of rotavirus infection among their infants up to six months. J Med Virol. 2007. 79:341–349.12. Cox MJ, Azevedo RS, Nokes DJ, Beards GM, McCrae MA, Massad E, Medley GF. Seroepidemiolgy of group A rotavirus in suburban São Paulo, Brazil. Epidemiol Infect. 1998. 120:327–334.13. Lee JI, Park SH, Kim MS, Oh YH, Yu IS, Choi BH, Lee GC, Kim MS, Jang SY, Lee CH. Surveillance of acute gastroenteritis in Seoul, Korea, during May 2004 and June 2007. J Bacteriol Virol. 2009. 39:363–371.14. Kim CR, Oh JW, Yun MK, Lee JH, Kang JO. Rotavirus infection in neonates at a university hospital in Korea. Infect Control Hosp Epidemiol. 2009. 30:893–895.15. Iijima Y, Iwamoto T, Nukuzuma S, Ohishi H, Hayashi K, Kobayashi N. An outbreak of rotavirus infection among adults in an institution for rehabilitation: long-term residence in a closed community as a risk factor for rotavirus illness. Scand J Infect Dis. 2006. 38:490–496.16. Burns JW, Siadat-Pajouh M, Krishnaney AA, Greenberg HB. Protective effect of rotavirus VP6-specific IgA monoclonal antibodies that lack neutralizing activity. Science. 1996. 272:104–107.17. Grimwood K, Lund JCS, Coulson BS, Hudson IL, Bishop RF, Barnes GL. Comparison of serum and mucosal antibody responses following severe acute rotavirus gastroenteritis in young children. J Clin Microbiol. 1988. 26:732–738.18. Tsunemitsu H, Jiang B, Saif LJ. Detection of group C rotavirus antigens and antibodies in animals and humans by ELISA. J Clin Microbiol. 1992. 30:2129–2134.19. O'Ryan M, Linhares AC. Update on Rotarix: an oral human rotavirus vaccine. Expert Rev Vaccines. 2009. 8:1627–1641.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Seroprevalence of Toxoplasma gondii Among Primary School Children in Shandong Province, China
- Shifting in Seroprevalence of HBsAg and Anti-HCV during Recent 10 Years in Adults Resident in Daegu and Gyeongbuk Province
- Patterns of Acute Hepatitis A and Anti-HAV Seroprevalence of Kyungin Province
- Seroprevalence of Toxoplasma gondii Infection among HIV/AIDS Patients in Eastern China
- Seroepidemiology of Hepatitis A and Hepatitis B in Korean Children